For more than 3 decades, the criteria for successful replacement of teeth with restored dental implants followed a narrow construct of scientific and clinical protocols. Whether the goals of tooth replacement focused on a single site, a partially edentulous quadrant, or an edentulous arch, it was assumed that dental implants had to be located at sites where the alveolar bone was of sufficient quality, quantity, and morphology. Furthermore, the protective role of periimplant gingiva or detrimental effects of microorganisms in the gingival crevice surrounding the restored implant was seldom considered. These findings were among the original ideology proposed by Brånemark that assumed multiple root form dental implants should only be placed in healed edentulous sites, covered with alveolar mucosa for 3 to 6 months before second-stage abutment connection and restoration, and located mostly in the anterior region of the edentulous mandible. Single-tooth and partially edentulous treatment comprised less than 5% of their restorative cases, and dental implant placement distal to the mandibular foramen was considered experimental.
These principles were mandated to achieve a 1-year implant survival outcome of 88% in the anterior maxilla and 94% for the anterior mandible. For a series of dental implants penetrating the maxillary sinus, the result showed a 5- to 10-year functioning percentage between 70% and 72%. The scientific documentation of the Brånemark group and their protocol for osseointegration strongly influenced clinical applications of dental implant therapy until about the early 1990s.
To achieve osseointegration, which was considered to be intimate contact of bone to dental implant as assessed at the light microscopic level, this initial protocol required that the implant must be one inserted with a low trauma surgical technique, be placed with initial stability, and should not be functionally loaded until sufficient bone has been deposited in mineralized form.
This traditional clinical protocol for placing dental implants demanded a uniform intimate contact between the dental implant and surrounding walls of bone from the most coronal aspect of the implant to its most apical extent. This was achieved by employing a set of drills or burs that would successively increase in diameter. Bone to implant contact was further clinically enhanced by the use of an osteotomy that was narrower than the intended dental implant. Finally, the fixture was slowly turned or tapped into the osteotomy with copious and cool saline irrigation until the most apical extent engaged in osteotomy.
Subsequent to this initial protocol, it has been determined that it is not always possible to prepare an osteotomy without clinical voids or gaps surrounding the fixture. Subsequently, clinical guidelines were developed that led to employing principles of guided tissue regeneration to create mineralized tissue that supported frustrations or dehiscence at the time of implant placement. Seeing that the initial protocol for dental implant placement required a completely healed extraction site, the next logical phase of implant therapy focused on placing dental implants in extraction sockets immediately upon tooth removal and delivering a comfortable, aesthetic, semifunctional provisional restoration.
Many of the available studies concerning the placement of dental implants in extraction sites describe their use in the anterior and premolar regions, but careful applications of surgical principles resulted in predictable success of dental implants placed in extraction sites immediately following the removal of molars. This chapter will review principles associated with root form dental implants immediately placed in extraction sockets.
▪
HEALING OF EXTRACTION SOCKETS: THE RESPONSE OF ALVEOLAR BONE FOLLOWING ROUTINE TOOTH EXTRACTION (WITHOUT SOCKET GRAFTING, RIDGE PRESERVATION OR IMMEDIATE IMPLANT PLACEMENT)
Once a tooth is extracted, the remodeling of the alveolar bone and the adaptation of the gingiva and mucosal tissue could compromise an idealized dental implant location. Depending on the quality, quantity, and morphology of the alveolar bone, extensive presurgical protocols aimed at preparing the area for dental implant placement might be needed if the alveolar bone is allowed to remodel after extraction. One significant factor driving clinicians toward placing dental implants in extraction sockets is based, in part, on the desire to avoid these hard and soft tissue site development techniques. Understanding the process of alveolar bone remodeling after tooth extraction is crucial in planning the location of dental implant placement at the time of tooth removal.
▪
ADAPTIVE MORPHOLOGY OF THE MAXILLARY ALVEOLAR PROCESS: RESPONSE IN THE AESTHETIC ZONE (THIN LABIAL BONE)
After tooth extraction, the alveolar bone is affected by a complex and progressive process. These changes can have a significant influence on the planned dental implant site. According to Atwood, the alveolar ridge atrophy is a chronic, progressive, irreversible disease. This process results in profound loss in the height and width as a result of the massive loss of bone volume a few months after a tooth is extracted.
▪
ADAPTIVE MORPHOLOGY OF THE MAXILLARY ALVEOLAR PROCESS: RESPONSE IN THE AESTHETIC ZONE (THIN LABIAL BONE)
After tooth extraction, the alveolar bone is affected by a complex and progressive process. These changes can have a significant influence on the planned dental implant site. According to Atwood, the alveolar ridge atrophy is a chronic, progressive, irreversible disease. This process results in profound loss in the height and width as a result of the massive loss of bone volume a few months after a tooth is extracted.
▪
FACTORS THAT AFFECT THE AMOUNT OF BONE LOSS FOLLOWING AN EXTRACTION
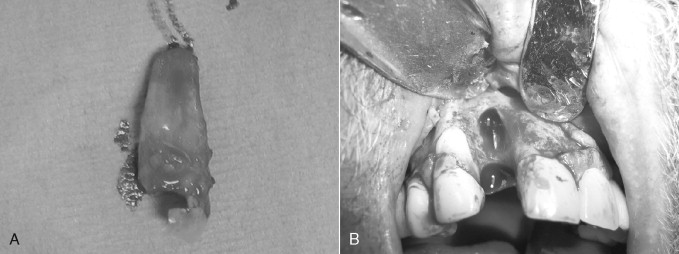
There are several factors that may influence the amount of bone loss that occurs following an extraction. The labial bone in the anterior maxilla is thin. Even a simple, atraumatic extraction may lead to extensive bone loss in this area as a result of the natural thin labial bone in this area. Atraumatic extraction techniques, including the use of Periotomes, minimizes trauma to the bone and soft tissue, thus minimizing the amount of bone loss resulting from the extraction. Extraction of endodontically treated teeth, teeth with curved roots, and retained roots of endodontically treated teeth all increase the possibility of a surgical flap and bone removal to extract the tooth ( Figure 33-1 A, B ).
▪
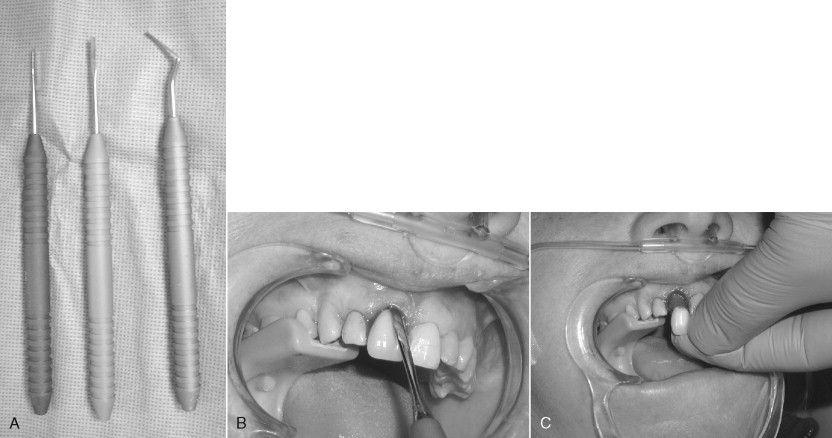
ATRAUMATIC EXTRACTION TECHNIQUES: THE USE OF PERIOTOMES
To minimize the amount of bone loss associated with a tooth extraction and to enhance the opportunity for immediate implant placement, atraumatic extraction techniques are extremely important. The use of Periotomes has greatly supported the opportunity to achieve an atraumatic extraction of a tooth ( Figure 33-2 A, B ). A Periotome is an instrument that is used to separate the periodontal attachments and fibers from the tooth root. Once the fibers or attachments are released from the roots, the tooth can be easily and atraumatically removed from the socket ( Figure 33-2 C ).
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


