Introduction
In this study, we measured the impact of cone-beam computed tomography (CBCT) on orthodontic diagnosis and treatment planning.
Methods
Participant orthodontists shown traditional orthodontic records for 6 patients were asked to provide a diagnostic problem list, a hypothetical treatment plan, and a clinical certainty. They then evaluated a CBCT scan for each patient and noted any changes, confirmations, or enhancements to their diagnosis and treatment plan.
Results
The number of diagnosis and treatment plan changes varied widely by patient characteristics. The most frequently reported diagnosis and treatment plan changes occurred in patients with unerupted teeth, severe root resorption, or severe skeletal discrepancies. We found no benefit in terms of changes in treatment plan for patients when the reason for obtaining a CBCT scan was to examine for abnormalities of the temporomandibular joint or airway, or crowding. Orthodontic participants who own CBCT machines or use CBCT scans frequently in practice reported significantly more diagnosis and treatment plan changes and greater confidence after viewing the CBCT scans during the study.
Conclusions
The results of this study support obtaining a CBCT scan before orthodontic diagnosis and treatment planning when a patient has an unerupted tooth with delayed eruption or a questionable location, severe root resorption as diagnosed with a periapical or panoramic radiograph, or a severe skeletal discrepancy. We propose that CBCT scans should be ordered only when there is clear, specific, individual clinical justification.
Radiographs are an indispensible tool in the evaluation of the bony structures of the head and neck in pretreatment orthodontic diagnosis and treatment planning. Previous research has shown that lateral cephalograms and panoramic, anterior periapical, and posterior bitewing radiographs provide sufficient information for most orthodontic patients. These radiographic techniques provide 2-dimensional information about the maxillomandibular relationship, the position of the dentition in relation to basal and alveolar bones, the airway, skeletal or dental disease, root anatomy and angulation, and a gross visualization of the osseous anatomy of the temporomandibular joint (TMJ).
With the advent of cone-beam computed tomography (CBCT), it became possible to evaluate the hard and soft tissues of the maxillofacial region in 3 dimensions and in high spatial detail. Additionally, visualization of the craniofacial complex in 3 dimensions is also possible with surface reconstruction views. Such information has the potential to improve orthodontic diagnosis and treatment planning, including airway analysis, TMJ evaluation, positions of impacted teeth, orthognathic surgical planning, evaluation of skeletal asymmetries, root position and structure, and miniscrew placement. However, the use of CBCT entails both financial costs and potential risks from radiation exposure.
Some researchers have provided recommendations for ordering CBCT scans based on specific characteristics, including facial asymmetry, sleep apnea, impacted teeth, intent to use dental mini-implants, consideration of rapid maxillary expansion, and persistent TMJ symptoms. Others have advocated the routine used of CBCT in standard orthodontic diagnosis and treatment planning because of the additional diagnostic information that is potentially available. The decision to use any imaging modality before orthodontic treatment is justified when there is a reasonable expectation that a radiograph will result in a clinical benefit. This study was designed to measure the impact of CBCT in orthodontic diagnosis and treatment planning, and to determine the extent to which patient characteristics might provide benefits to clinicians in diagnosis and treatment planning.
Material and methods
The records and study models of 6 patients treated in the orthodontic clinic at the University of California at Los Angeles were selected and duplicated. The patient case records included, at a minimum, medical and dental histories; stone study models trimmed to centric relation; images of the full-mouth intraoral and extraoral photographs; lateral cephalometric, panoramic, and full-mouth series views; and the initial CBCT examination. All CBCT scans were made on a NewTom 3G machine (QR S.r.l., Verona, Italy) with a 12-in field of view and reconstructed with a 0.5-mm slice thickness.
The cases were selected to represent a broad range of clinical characteristics commonly encountered in orthodontic practices, including Class I, Class II, and Class III molar relationships, canine impactions, anterior open bites, anterior and posterior crossbites, dental crowding, airway and TMJ problems, and severe skeletal asymmetries ( Table I ). The cases exposed the participants to common patient characteristics, especially problems where CBCT has been suggested to be beneficial, but without regard to prevalence. For example, the prevalence of impacted maxillary canines is 1% to 2.5%, but in our study, impacted maxillary canines were present in 2 of the 6 cases.
| Patient case | Age | Sex | Angle class | Unerupted tooth | Root position/resorption | Severe skeletal discrepancy | TMD | Airway problem | Crowding | Case severity |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 13 y 0 mo | M | II | N | N | N | N | N | N | Low |
| 2 | 7 y 3 mo | F | III | Y | N | N | N | N | Y | Low |
| 3 | 15 y 3 mo | M | I | N | N | N | N | Y | Y | Medium |
| 4 | 11 y 6 mo | F | II | Y | Y | N | N | N | Y | High |
| 5 | 20 y 1 mo | F | II | Y | N | Y | Y | Y | N | High |
| 6 | 16 y 1 mo | M | III | N | N | Y | N | Y | Y | Medium |
Letters briefly describing the study and inviting participation were sent via e-mail to 219 members of the Pacific Coast Society of Orthodontists who resided in the Southern California area. A letter was also sent to the program directors of the 3 regional orthodontic programs: University of California, Los Angeles; University of Southern California, Los Angeles; and Loma Linda University, Loma Linda, Calif. Those who responded were contacted and told that participation would consist of 1 interview (estimated to last about 2 hours) during which the participant would be shown orthodontic cases and asked to provide hypothetical diagnoses and treatment plans. The participants were assured that the accuracy of their diagnosis and treatment plan was not being evaluated, but, rather, the investigators wished to determine the information used to formulate their diagnoses and treatment plans. This study was approved by the institutional review board of the University of California at Los Angeles.
A standardized interview was used. Descriptive data were gathered about the participants (sex, orthodontic program and year of graduation, whether they owned a CBCT device, and for what percentage of their patients did they order CBCT scans before treatment). The participants were shown the case records for the 6 patients. One case, selected by the investigators as an easy diagnostic one, was always presented first to familiarize the participants with the process. The order of presentation of the other 5 cases was systematically varied to prevent changes to the outcome variables associated with fatigue.
Each case was presented on a 15.4-in screen (MacBook Pro; Apple, Cupertino, Calif) with software (Dolphin Imaging, Chatsworth, Calif). The participants were given each patient’s medical and dental histories and shown the study models, intraoral and extraoral photographs, and lateral cephalometric, panoramic, and full-mouth series radiographs. The participant was allowed to rotate and manipulate all images (except the CBCT images) during this part of the interview. They were asked to describe their diagnostic problem list. They were also asked to provide their degree of certainty with their diagnosis using a visual analog scale ranging from 0% (complete guess) to 100% (absolutely certain). This process was repeated for the treatment plan.
The participants were then asked whether they would request a CBCT scan for this patient and their rationale. Regardless of whether they requested a CBCT scan, the participants were asked to evaluate the CBCT examination and note any changes, enhancements, or confirmations to their diagnosis and treatment plan, including reasons for these changes. Next, the participants were given preconstructed images of the TMJ, impacted teeth, and teeth with root resorption. They were also encouraged to view the multi-planar reconstructions and to create any other cross-sections from the CBCT scan that would contribute to their diagnosis and treatment plan.
After data collection, the considerations for ordering CBCT scans and associated diagnostic and treatment plan changes were grouped into the following 8 categories: unerupted tooth, root position or resorption (>2 mm), severe skeletal discrepancy (−2° ≥ ANB ≥ 6°, or asymmetry ≥4 mm), TMJ disorder (signs or symptoms of clicking, popping, or pain), airway problems, crowding (>5 mm in either arch), medico-legal reasons, and financial costs. During the analysis, a hierarchy of change, enhancement, and confirmation was established, with a change having the greatest impact. For example, if a participant reported a change and an enhancement to a diagnosis, both were recorded but only the change was used for analysis.
The participants then provided final percentages of certainty for both their diagnoses and treatment plans. At the conclusion of each case, the participants were asked how the CBCT scan was useful in their diagnosis and whether the information from it would have influenced the treatment outcome for that patient. They were allowed to explain any radiographs or other diagnostic aids that they would have ordered if the CBCT scan were unavailable.
Statistical analysis
The P values for comparing binary outcomes (percentages) from the same participants across patient profiles were computed by using the Cochran Q procedure, a generalization of the McNemar test for balanced 2 × k tables, where k is the number of subjects. For comparisons across categories when participant-patient was the unit of analysis, this was expanded to a repeated-measure logistic model with a random participant effect to take into account nonindependence.
The P values for comparing continuous confidence score outcomes across patients from the same participants were computed by using the nonparametric Friedman test for repeated-measure comparisons, a generalization of the Wilcoxon signed rank test for paired continuous data.
Results
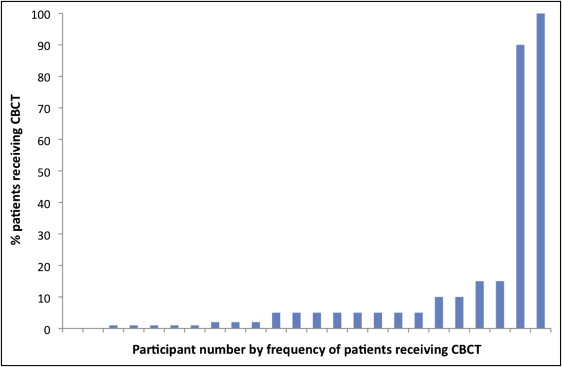
Twenty-four participants began the interview process, and 23 finished all 6 patient cases; 1 participant finished 5. The participants were mostly men (n = 21), trained at 10 orthodontic programs, and had an average of 24 years of experience (range, 1-44 years). The participants reported using CBCT examinations for 0% to 100% of their patients in their practices (mean, 12.1%; median, 5%) ( Fig 1 ).
There were 64 CBCT scans ordered (45% of opportunities) during the interview process ( Table II ). The number of CBCT requests for each case ranged from 2 to 22, and 64% of the CBCT scans requested were for cases 4 and 5. For case 1, only 2 CBCT scans were requested. Two participants never requested a CBCT during their review of the 6 cases, 16 participants ordered 2 to 4 CBCT scans, and 2 participants requested a CBCT scan for all 6 cases ( Table III ).
| Patient case | CBCT scans ordered | Differences | ||
|---|---|---|---|---|
| n | % | SE | ||
| 1 | 2 ∗ | 8 | ±6 | 2, 3, 4, 5, 6 |
| 2 | 6 | 25 | ±9 | 1, 4, 5 |
| 3 | 7 | 29 | ±10 | 1, 4, 5 |
| 4 | 22 † | 92 | ±6 | 1, 2, 3, 6 |
| 5 | 19 † | 79 | ±9 | 1, 2, 3, 6 |
| 6 | 8 | 35 | ±10 | 1, 4, 5 |
| Total | 64 | 45 | ±2.8 | |
| CBCT scans requested (n) | Participants (n) |
|---|---|
| 0 | 2 |
| 1 | 3 |
| 2 | 8 |
| 3 | 4 |
| 4 | 4 |
| 5 | 1 |
| 6 | 2 |
There were 26 changes to the participants’ diagnoses after viewing the CBCT scans (18% of opportunities) and 28 changes to the treatment plans (20% of opportunities) ( Table IV ). The number of changes varied widely by patient case, ranging from 1 to 11, with cases 4 and 5 together comprising over 67% of the changes to the diagnoses (18 of 26 changes) and treatment plans (19 of 28 changes).
| Patient case | Diagnosis changes | Treatment plan changes | ||||
|---|---|---|---|---|---|---|
| n | % | SE | n | % | SE | |
| 1 | 1 | 4 | ±4 | 2 | 8 | ±6 |
| 2 | 2 | 8 | ±6 | 2 | 8 | ±6 |
| 3 | 1 | 4 | ±4 | 1 | 4 | ±4 |
| 4 | 9 ∗ | 38 | ±10 | 8 ∗ | 33 | ±10 |
| 5 | 9 ∗ | 38 | ±10 | 11 † | 46 | ±10 |
| 6 | 4 | 17 | ±8 | 4 | 17 | ±8 |
| Total | 26 | 18 | 28 | 20 | ||
∗ Significantly different from cases 1, 2, and 3 ( P <0.05).
† significantly different from cases 1, 2, 3, and 6 ( P <0.05).
The number of CBCT scans ordered and the number of resulting changes to the diagnoses and treatment plans varied by patient characteristics ( Table V ). Multiple characteristics were present in each case; thus, participants gave multiple reasons for ordering a CBCT scan and for a change to a diagnosis or treatment plan.
| Patient characteristic | n | Characteristic present | CBCT scan ordered | Diagnosis change | Treatment plan change | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| n | % | SE (%) | n | % | SE (%) | n | % | SE (%) | |||
| Unerupted tooth | 71 | N | 2 | 3 | 2 | 0 | 0 | 0 | 0 | 0 | 0 |
| 72 | Y | 39 ∗ | 54 | 6 | 15 ∗ | 21 | 5 | 16 ∗ | 22 | 5 | |
| Root position/resorption | 119 | N | 8 | 7 | 2 | 2 | 2 | 1 | 0 | 0 | 0 |
| 24 | Y | 13 ∗ | 54 | 10 | 3 ∗ | 13 | 7 | 6 ∗ | 25 | 9 | |
| Severe skeletal discrepancy | 96 | N | 3 | 3 | 2 | 0 | 0 | 0 | 1 | 1 | 1 |
| 47 | Y | 6 ∗ | 13 | 5 | 5 ∗ | 11 | 5 | 6 ∗ | 13 | 5 | |
| TMD | 119 | N | 9 | 8 | 2 | 6 | 5 | 2 | 1 | 1 | 1 |
| 24 | Y | 4 ∗ | 17 | 8 | 3 | 13 | 7 | 2 | 8 | 6 | |
| Airway problem | 72 | N | 3 | 4 | 2 | 3 | 4 | 2 | 3 | 4 | 2 |
| 71 | Y | 11 ∗ | 15 | 4 | 3 | 4 | 2 | 3 | 4 | 2 | |
| Crowding | 48 | N | 2 | 4 | 3 | 1 | 2 | 2 | 0 | 0 | 0 |
| 95 | Y | 8 | 8 | 3 | 2 | 2 | 1 | 4 | 4 | 2 | |
For 5 of the 6 patient characteristics, participants ordered CBCT scans more frequently ( P <0.05) when the characteristic was present. An unerupted tooth was the most frequently cited reason for ordering a CBCT scan (64% of orders), followed by root resorption (33% of orders). Of the 72 observations on patients with unerupted teeth, a CBCT scan was ordered 39 times when the characteristic was present (54%) and only twice when the characteristic was not present. Root resorption was cited as the rationale for ordering the CBCT scan 13 times when the characteristic was present (54%) and 8 times (7%) when the characteristic was not present. Severe skeletal discrepancy, TMJ disorders, and airway problems were cited less frequently, yet still significantly more frequently when the characteristic was present. Crowding was offered as a reason for ordering a scan but was not statistically significant.
For 3 of the 6 patient characteristics—unerupted tooth, root resorption, and severe skeletal discrepancy—the participants reported changes to the diagnosis and treatment plan significantly more frequently when the characteristic was present. An unerupted tooth was the most frequently cited reason for changes to the diagnosis (15 instances, or 21% of the cases with the characteristic present) and treatment plan (16 instances, or 22%). It was never mentioned in cases without the characteristic present. Root position or resorption was present in fewer cases, and CBCT scans were ordered for diagnostic reasons both when the characteristic was present (3 times) and when it was not (2 times). In proportion, it was the most common reason for treatment plan changes (6 times, or 25%). Severe skeletal discrepancy was reported as a reason for a change to the diagnosis 5 times (11%). For the treatment plan, 6 changes occurred when there was a severe skeletal discrepancy and once when it was not present. There was no significant difference in the reasons cited for ordering by the presence or absence of the characteristics for TMJ disorder, airway problem, and crowding.
Treatment outcome was defined as the expected result of treatment as reported by the participants. We evaluated the association between treatment plan changes and expected effect on treatment outcome as reported by the participants ( Table VI ). The presence of unerupted teeth resulted in 16 treatment changes, and the participants expected that 7 (44%) of these would affect patient outcome. For the other patient characteristics, the participants reported that the changes would affect patient outcome for between 67% and 100% of the treatment plans.
| Patient characteristic | Treatment plan changes | Treatment plan change and outcome affected | Proportion (%) | SE (%) |
|---|---|---|---|---|
| Unerupted tooth | 16 | 7 | 44 | 12 |
| Root position/resorption | 6 | 5 | 83 | 15 |
| Severe skeletal discrepancy | 7 | 7 | 100 | 0 |
| TMD | 3 | 2 | 67 | 27 |
| Airway problem | 6 | 5 | 83 | 15 |
| Crowding | 4 | 4 | 100 | 0 |
| Total | 42 | 30 | 71 |
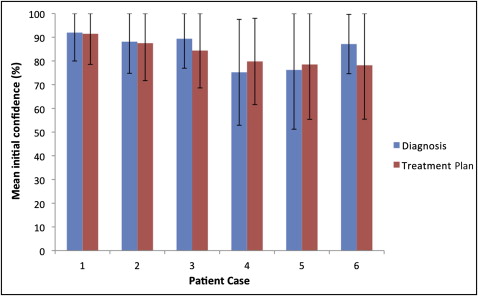
The participants’ initial confidence ranged from 75% to 97% for diagnoses, and from 83% to 95% for treatment plans ( Fig 2 ). Patient cases 4 and 5 had the lowest mean initial diagnosis confidence values; case 1 had the highest value. Significant increases in the mean percentages of confidence in the diagnoses and treatment plans were demonstrated for patient cases 2 to 6 after the participants viewed the CBCT scans ( Fig 3 ).

Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


