Introduction
The aims of this study were to compare lateral cephalograms with other radiologic methods for diagnosing suspected fusions of the cervical spine and to validate the assessment of congenital fusions and osteoarthritic changes against the anatomic truth.
Methods
Four cadaver heads were selected with fusion of vertebrae C2 and C3 seen on a lateral cephalogram. Multidetector computed tomography (MDCT) and cone-beam computed tomography (CBCT) were performed and assessed by 5 general radiologists and 5 oral radiologists, respectively. Vertebrae C2 and C3 were examined for osseous fusions, and the left and right facet joints were diagnosed for osteoarthritis. Subsequently, the C2 and C3 were macerated and appraised by a pathologist. Descriptive analysis was performed, and interrater agreements between and within the groups were computed.
Results
All macerated specimens showed osteoarthritic findings of varying degrees, but no congenital bony fusion. All observers agreed that no fusion was found on MDCT or CBCT. They disagreed on the prevalence of osteoarthritic deformities (general radiologists/MDCT, 100%; oral radiologists/CBCT, 93.3%) and joint space assessment in the facet joints (kappa = 0.452). The agreement within the rater groups differed considerably (general radiologists/MDCT, kappa = 0.612; oral radiologists/CBCT, kappa = 0.240).
Conclusions
Lateral cephalograms do not provide dependable data to assess the cervical spine for fusions and cause false-positive detections. Both MDCT interpreted by general radiologists and CBCT interpreted by oral radiologists are reliable methods to exclude potential fusions. Degenerative osteoarthritic changes are diagnosed more accurately and consistently by general radiologists evaluating MDCT.
In recent years, orthodontists have expressed increasing interest in assessing the cervical spine on a lateral cephalogram. One clinical purpose is the determination of skeletal age based on the association between age-related morphologic changes of the upper cervical vertebrae and the somatic growth curve. A further intent is the evaluation of the craniocervical angulation to characterize head posture, which has been linked to nasorespiratory function and craniofacial morphology. Moreover, the use of lateral cephalograms has also been recommended to study congenital anomalies of the cervical vertebrae, because cervical vertebral anomalies, particularly fusions, could be related to certain craniofacial syndromes and other dentoskeletal malformations. Awareness that the spine is of clinical interest has led to the recommendation to use cephalometric radiographs to routinely screen the cervical vertebrae for anomalies and even to develop a tracing technique of this region.
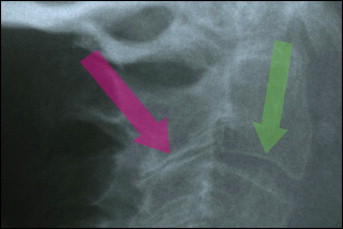
Fusions are most common between the facet joints of the second and third vertebrae (C2 and C3; Fig 1 ). Like all other cervical vertebral anomalies, osseous fusions are usually asymptomatic and considered to be coincidental findings with no clinical relevance. However, in a few patients, cervical vertebral anomalies cause compression of neurologic structures or biomechanical instability, leading to chronic pain. Associations between cervical vertebral anomalies, notably fusion of C2 and C3, and congenital disorders or dentoskeletal malocclusions have been studied extensively. They include syndromic and nonsyndromic anomalies such as fetal alcohol syndrome and cleft lip and palate. In recent research examining cervical vertebral anomalies on lateral cephalograms, a high prevalence of cervical vertebral anomalies, particularly fusions of C2 and C3, was reported in orthodontic surgical patients with severe skeletal malocclusions. The described associations between cephalometric measurements and fusions include skeletal Class III and mandibular overjet with 61.4% fusions, skeletal deepbite with 41.5% fusions, skeletal open bite with 42.1% fusions, and skeletal Class II and maxillary overjet with 28% and 52.9% fusions, respectively. A similarly high prevalence of fusions has been documented in subjects with condylar hypoplasia with 72.7% fusions (45% in C2 and C3) and in patients with obstructive sleep apnea (46%).

These findings have been challenged by some who argued that it was difficult to reliably determine cervical vertebral anomalies on 1 lateral cephalogram. Considerably lower prevalence numbers (<0.9%) have been reported in other studies with normal populations ; this could be because patients with severe malocclusions are significantly different from a normal population, but this dissonance in prevalence certainly raises the question as to whether lateral cephalograms are a reliable tool to assess cervical vertebral anomalies. Koletsis and Halazonetis stated that no study investigating the reliability of cephalometric radiography in the cervical region has been published to date. To validate the assessment of the spine on lateral cephalograms, 3-dimensional radiological data and direct observation (on autopsy material) have been suggested. A cadaver study would allow for direct comparisons of different assessment methods and validate each diagnostic approach against the anatomic truth.
In addition, a cadaver study would serve another purpose: diagnostic thinking efficacy evaluates whether the information retrieved from radiologic images leads to a change in the clinician’s diagnostic thinking. This efficacy has been evaluated for cone-beam computed tomography (CBCT) in relation to impacted third molars, impacted canines, root resorption of adjacent teeth, and the temporomandibular joint, but it has not been appraised for the cervical spine. Since the cervical spine is a region of interest for the orthodontist, it would be beneficial to assess the diagnostic efficacy of oral radiologists examining CBCT data and to compare it with that of general radiologists analyzing multidetector computed tomography (MDCT) data, and to verify the results against the anatomic findings.
The objectives of this cadaver study were therefore (1) to ascertain whether fusions of C2 and C3 suspected on lateral cephalograms would also be diagnosed by general radiologists on MDCT or oral radiologists on CBCT, and (2) to validate MDCT and CBCT assessments of congenital fusions and osteoarthritic changes against the anatomic truth.
Material and methods
From a larger collection of perfused cadaver heads, 8 specimens were selected for which analog, postmortem lateral cephalograms were available (tube voltage, 67; tube current, 250 mA; exposure time, 0.04 second; tube current time product, 10 mAs; focus to coronal plane distance, 200 cm). The cadaver heads were supplied by the Institute of Anatomy at the University of Zurich in Switzerland in accordance with state and federal regulations (ie, voluntary body donation program on the basis of informed consent), the Convention on Human Rights and Medicine, and the recommendation of the National Academy of Medical Science. The perfusion was carried out within 4 days after death with a fixation liquid consisting of 2 parts alcohol (70%), 1 part glycerine, and 2% almudor (containing 8.1% formaldehyde, 10% glyoxal, and 3.7% glutaraldehyde).
The lateral cephalograms were screened and assessed for potential fusions of cervical vertebrae by an author (D.B.) following the method prescribed in the literature: fusions were identified as an osseous continuity between C2 and C3 without complete separation at the articular facets or intervertebral disc space (see Fig 2 for an excluded specimen with a continuous radiolucent area). Four specimens (3 female, 1 male; age range, 65-87 years; mean age, 78 years) fulfilled the inclusion criterion of a suspected cervical spine fusion at the level of C2 and C3 and were used for the study.
MDCT was performed on a 40-detector row computed tomography system (Brilliance CT 40; Philips Healthcare, Eindhoven, The Netherlands) with the following scan parameters kept identical for all specimens: tube voltage, 120 kV; tube current time product, 70 mAs; slice collimation, 20 × 0.625 mm; pitch, 0.68; reconstruction slice thickness, 0.67 mm; reconstruction increment, 0.33 mm; window level setting, 2000/500 Hounsfield units; voxel sizes, 0.39 mm (x-axis), 0.39 mm (y-axis), and 0.67 mm (z-axis). Sagittal and coronal reformatted images (slice thickness, 1 mm; increment, 0.5 mm) were viewed on a high-resolution diagnostic workstation (dx IDS5; Sectra PACS, Linköping, Sweden).
The CBCT scans were made on a scanner with an amorphous silicon flat panel (KaVo 3D exam; KaVo Dental, Bismarckring, Germany). The following scan parameters were kept identical during all CBCT examinations: tube voltage, 120 kV; tube current time product, 37.07 mAs; reconstruction thickness, 0.25 mm; reconstruction increment, 0.25 mm; voxel size, 0.25 mm (x-axis), 0.25 mm (y-axis), and 0.25 mm (z-axis). Digital imaging and communications in medicine (DICOM) files were reformatted in multiplanar reconstructions by using open-source postprocessing software (Workstation version 2.0 SP1; ClearCanvas, Toronto, Ontario, Canada).
Five general radiologists were asked to evaluate the MDCT data, and 5 dentists with special postgraduate training in oral radiology were asked to evaluate the CBCT data.
Three areas were assessed for a potential congenital fusion: facet joint (C2-C3) of the left and right articular processes and the intervertebral disc space between the 2 bodies, C2 and C3.
Additionally, the raters were requested to perform their radiological appraisals for the left and right facet joints in the following manner: (1) normal joint or (2) osteoarthritis (joint space entirely preserved, partially preserved, or not visible).
All radiologists assessed the images independently, in blinded fashion, and without knowledge of the anatomic findings.
After image acquisition, the cervical spines were isolated en bloc from the cadaver heads. Lipids were dissolved in a Supralan UF solution (Bauer Handels, Fehraltorf, Switzerland) with sodium chloride. Enzymatic maceration was performed with papain (Bauer Handels) at pH 6 to 7 in Supralan UF and a solution containing sodium chloride for up to 14 days.
The macerated spines were subsequently analyzed for fusions and osteoarthritis by a board-certified pathologist.
Statistical analysis
A standard statistical software package (version 11.4.1.0; MedCalc Software, Mariakerke, Belgium) was used for the descriptive data analysis. An unweighted Cohen kappa test was computed to evaluate the agreement between the CBCT and MDCT methods. To determine interobserver agreement between the 5 CBCT radiologists and the 5 MDCT radiologists, a Fleiss kappa test for multiple raters was calculated with StatTools.
Results
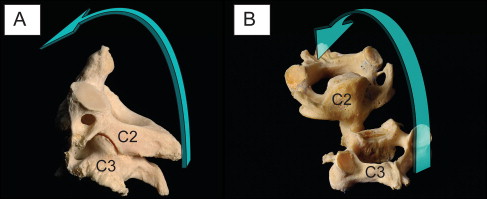
After the enzymatic maceration, the vertebral bodies C2 and C3 could be completely mobilized, proving the absence of congenital bony fusions in these vertebral segments ( Figs 3-5 ). All facet joints showed degenerative osteoarthritic changes including osteophytes, peripheral eburnation, and gross irregularities of the subchondral joint surfaces of varying degrees. The facets of 2 specimens were more severely affected, exhibiting extensive osteophytes and ragged bony joint surfaces ( Fig 5 ).
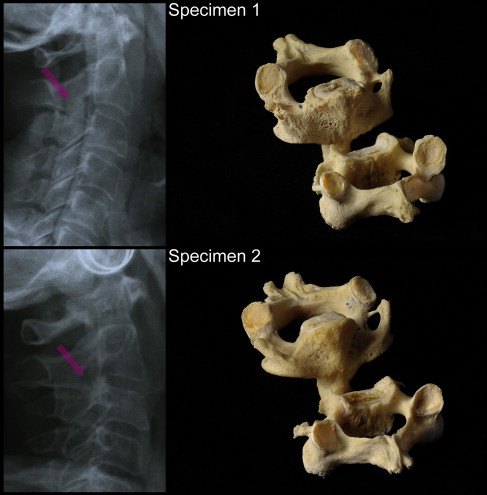
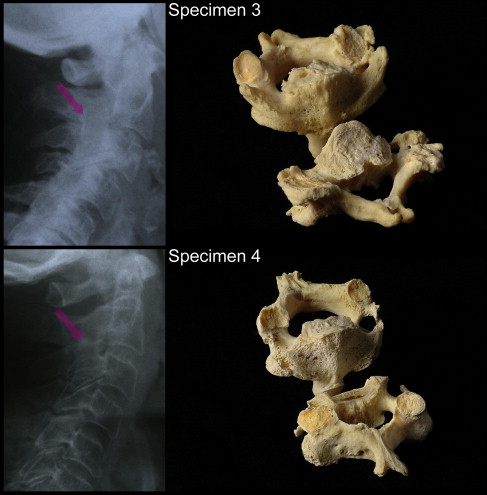
All raters agreed that no congenital fusion was found by MDCT or CBCT, but there was disagreement concerning the prevalence of the osteoarthritic deformities. General radiologists assessing the MDCT recognized osteoarthritic changes in 100% (40/40) of the joint assessments, and oral radiologists evaluating the CBCT found osteoarthritic changes in 93.3% (38/40). Moreover, when evaluating the narrowing of the joint space in the affected osteoarthritic joints, the 2 rater groups differed substantially ( Table I ). The concordance between the 2 rater groups was rather modest (70%) with a kappa value of 0.452 (SE, 0.132; 95% confidence interval [CI], 0.193-0.711), indicating moderate agreement.
| Osteoarthritic joint assessment | General radiologists/MDCT | Oral radiologists/CBCT |
|---|---|---|
| Osteoarthritic joint, joint space entirely preserved | 80.0% | 51.8% |
| Osteoarthritic joint, joint space partially preserved | 20.0% | 48.2% |
| Osteoarthritic joint, joint space not visible | 0% | 0% |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


