A girl with an Angle Class III malocclusion, anterior and posterior crossbites, a concave profile, and cleft lip and palate sought orthodontic treatment. She was treated with a multidisciplinary therapeutic protocol including orthodontic and surgical procedures. The proposed objectives of occlusion, normal function, and balanced profile were achieved, and these results remained stable 4 years after the treatment.
Cleft lip and palate (CLP) is the most frequent congenital facial abnormality. Its incidence varies according to studied populations but is usually between 1 and 1.82 for each 1000 births. The etiology is related to genetic heritage or environmental factors. CLP patients might suffer from unfavorable smile esthetics and low self-esteem, leading mainly to difficulties in social interactions. Patients with CLP have typical characteristics, such as deficiency in midface development, orthodontic Class III tendency, significantly smaller ANB angle, oronasal fistulae in some cases, alterations in shape and number of the lateral incisors, and, occasionally, supernumerary teeth.
The multidisciplinary therapeutic protocol frequently extends over many years, starting with primary surgeries up to the end of adolescence. Treatment might start around 3 to 6 months of age with a labial repair or at 10 to 12 months of age with palatoplasty. Secondary alveolar bone grafting is indicated for most patients with an alveolar cleft, and the best stage for the procedure is when the canine adjacent to the cleft has completed half to three quarters of its root formation. Orthodontic treatment before bone grafting might be performed, aiming to improve the maxillary relationship and the facial profile, as well as to aid positioning of cleft alveolar segments, leading to a more favorable graft prognosis. If successful, this surgery enhances the dental alveolus for eruption and periodontal support of the teeth adjacent to the cleft, usually the canine and the lateral incisor. Surgical protocols might use several areas as bone donors, such as the mandibular symphysis and the iliac crest, which are the most used.
The purpose of this report was to show that an interdisciplinary treatment protocol, after adequate diagnosis and planning, significantly improves the alterations resulting from a bilateral CLP deformity. The proposed objectives of occlusion, normal function, and balanced profile were achieved, and these results remained stable 4 years after the treatment.
Diagnosis and etiology
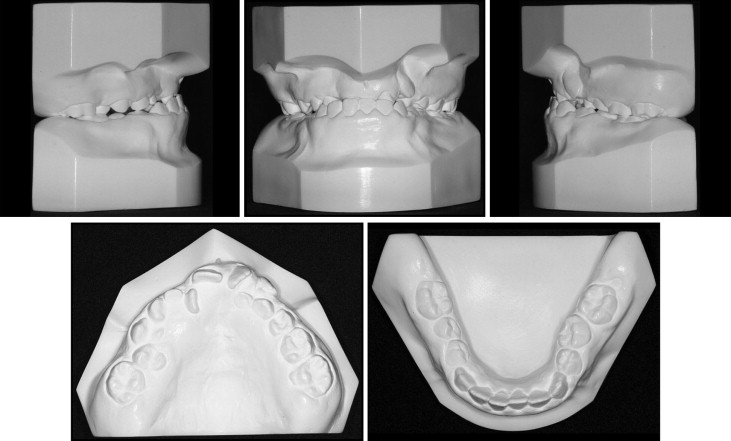
A girl, aged 9 years 8 months, with a complete bilateral CLP, sought care at the Care Facility for Patients with Facial Deformity at the Federal University of Santa Catarina in Brazil. The facial assessment showed a functional mandibular deviation to the right side and vertical balance among the facial thirds. The facial profile was concave with a retrusive upper lip ( Fig 1 ). She was at the end of the mixed dentition and had an anterior crossbite and Class III molar and canine relationships. Her soft and hard palates had been repaired successfully at 1 year of age. She had an atresic maxilla in the premolar and canine areas, overjet of −2 mm, and 50% overbite. The dental cast discrepancies were −5 mm for the maxilla and −0.5 mm for the mandible. The mandibular midline deviated 2 mm to the right and was related to the postural mandibular deviation resulting from the posterior crossbite. The maxillary midline was deviated 2 mm to the left ( Fig 2 ).

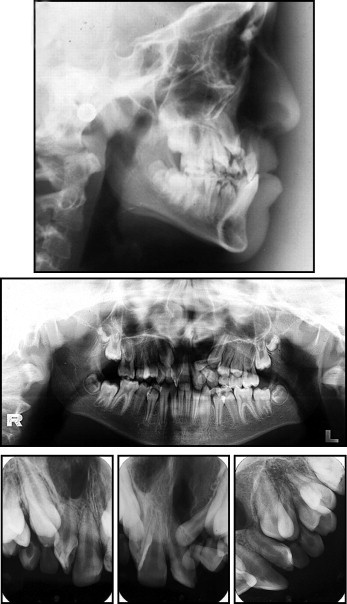
Panoramic and periapical radiographs showed the presence of all permanent teeth, and the maxillary lateral incisors adjacent to the cleft were malpositioned. Four supernumerary teeth (precanine type) were additionally diagnosed as 2 deciduous teeth accompanied by their successors. They were bilaterally positioned at the distal ridge of the alveolar clefts. The lateral cephalometric radiograph showed skeletal maxillomandibular horizontal balance (ANB, 3.5°; NAPog, 5.0°; AO-BO, 1.0 mm) ( Table ). The facial growth vector was predominantly vertical (GoGn.SN, 33°; FMA, 32°; y-axis, 63.5°) ( Fig 3 ). The maxillary incisors had accentuated vertical angulation (1.NA, −4°; 1-NA, 0 mm), whereas the mandibular incisors were well positioned (1.NB, 23°; 1-NB, 5 mm; IMPA, 92°). The maxillary incisor retroclination led to buccally positioned roots, influencing the contour of the anterior maxillary vestibule; this produced an increased ANB angle and masked the retrusive maxillary position. Her hand and wrist radiographs were compatible with a bone age of 10 years. The thumb abductor sesamoid was present, indicating that the pubertal growth spurt had already started ( Fig 4 ).
| Measurements | Normal | Pretreatment | Posttreatment | Difference |
|---|---|---|---|---|
| Skeletal pattern | ||||
| SNA (°) | 82 | 80 | 83 | 3 |
| SNB (°) | 80 | 76.5 | 82 | 5.5 |
| ANB (°) | 2 | 3.5 | 1 | −2.5 |
| Facial convexity (°) | 0 | 5 | 0 | −5 |
| Y-axis (°) | 59 | 63.5 | 65 | 1.5 |
| Facial angle (°) | 87 | 81 | 81 | 0 |
| SN.GoGn (°) | 32 | 33 | 35 | 2 |
| AO-BO (mm) | 0 | 1 | 3.5 | 2.5 |
| FMA (°) | 25 | 32 | 33.5 | 1.5 |
| Dental pattern | ||||
| IMPA (°) | 90 | 92 | 82 | −10 |
| 1.NA (°) | 22 | −4 | 35 | 39 |
| 1-NA (mm) | 4 | 0 | 5 | 5 |
| 1.NB (°) | 25 | 23 | 17 | −6 |
| 1-NB (mm) | 4 | 5 | 4 | −1 |
| 1.1 (°) | 130 | 156 | 133 | −23 |
| Profile | ||||
| Upper lip-S line (mm) | 0 | −1.5 | −1 | 0.5 |
| Lower lip-S line (mm) | 0 | 3 | 3 | 0 |

Treatment objectives
The main goals of the treatment were to correct the anterior and posterior crossbites, perform a bilateral secondary bone graft, and perform dental alignment and leveling to achieve adequate intercuspation. In addition to the occlusal alterations, balancing of the patient’s profile was also desired.
Treatment objectives
The main goals of the treatment were to correct the anterior and posterior crossbites, perform a bilateral secondary bone graft, and perform dental alignment and leveling to achieve adequate intercuspation. In addition to the occlusal alterations, balancing of the patient’s profile was also desired.
Treatment alternatives
Anterior and posterior crossbites are better corrected early in treatment. Thus, maxillary expansion and protraction were planned for the initial stages of orthodontic therapy. Maxillary surgical advancement or mandibular setback in adulthood would be another option, if the mandibular or maxillary growth did not respond favorably.
If the bone graft of the maxillary cleft were successful, the first option would be to move the supernumerary teeth into the lateral incisor positions. The lack of bone and gingival support for the existing lateral incisors favored their extraction. Other options could have been (1) mesial movement of posterior teeth with closure of the space distal to the central incisors, (2) implants when the lateral incisors or supernumerary teeth were lost, (3) surgical mesial positioning of the posterior maxillary segments if the grafts failed, and (4) partial or fixed prostheses between the central incisors and the canines if other alternatives including grafting failed.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


