Iatrogenic disease

INTRODUCTION
A number of medical and surgical treatments and dental interventions (Table 54.1) can result in iatrogenic (from the Greek iatros = doctor) diseases affecting various orofacial tissues and/or oral healthcare. A surprisingly wide range of infections, materials and drugs can affect the orofacial tissues on occasion and the astute diagnostician will always search the literature for such possibilities.
Table 54.1
| Cause | Specifics | Disorders |
| Cancer treatments | See text | |
| Dental appliances | Dentures/obturators | Denture-related stomatitis Angular stomatitis Denture-induced hyperplasia Traumatic ulceration Caries |
| Orthodontic appliances* | Traumatic ulceration Stomatitis Pain Root resorption Decalcification Caries |
|
| Dental interventions | Cross-infection | Various agents |
| Local analgesic injections | Transient diplopia Transient facial palsy Nerve damage Haematoma Trismus Infection |
|
| Tissue damage | Mainly soft tissue haematomas, lacerations or ulceration | |
| Tissue infection | Various | |
| Inhaled foreign bodies | Respiratory obstruction or infection | |
| Swallowed foreign bodies | Typically pass without consequence | |
| Foreign body in tissues | Granulomatous reaction | |
| Air in tissues | Surgical emphysema | |
| Psychological sequelae | Dental anxiety Dental phobia |
|
| Dental materials | Amalgam | Amalgam tattoo Lichenoid reactions |
| Other materials | Foreign body gingivitis | |
| Corrosives | Burns | |
| Allergens | Angioedema | |
| Drugs | See Tables 54.3–54.31 | Wide range of disorders |
| Immunosuppressive treatments | See text | |
| Restorative dental procedures | Damage to teeth or soft tissues | Fracture or trauma Root perforation |
| Pulp damage | Non-vital teeth Dental abscess Odontogenic infections |
|
| Endodontic material extrusion | Nerve damage Sinus infection Osteochemonecrosis |
|
| Endodontic instrument breakage | Endodontic failure | |
| Surgery | Infection | Localized osteitis (dry socket) Osteomyelitis Bisphosphonate osteonecrosis Osteoradionecrosis |
| Nerve injury | Sensory loss Facial palsy |
|
| Bone fracture | Alveolar bone or jaw fracture |
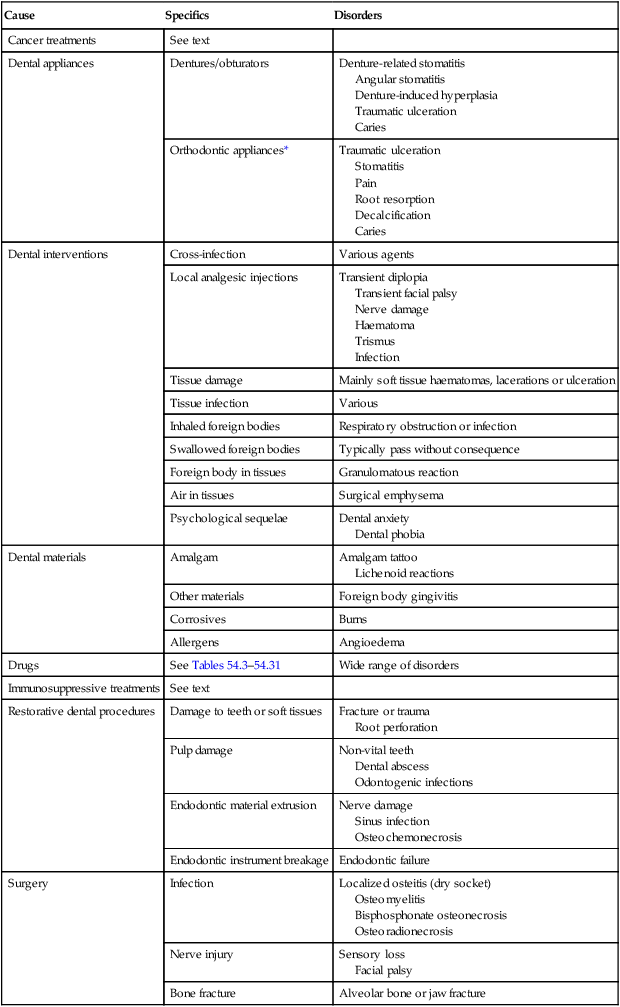
** Suggestedly implicated in Alzheimer disease but no reliable evidence available.
*Although some TMJ pain-dysfunction has been attributed to orthodontic treatment no reliable evidence is available.
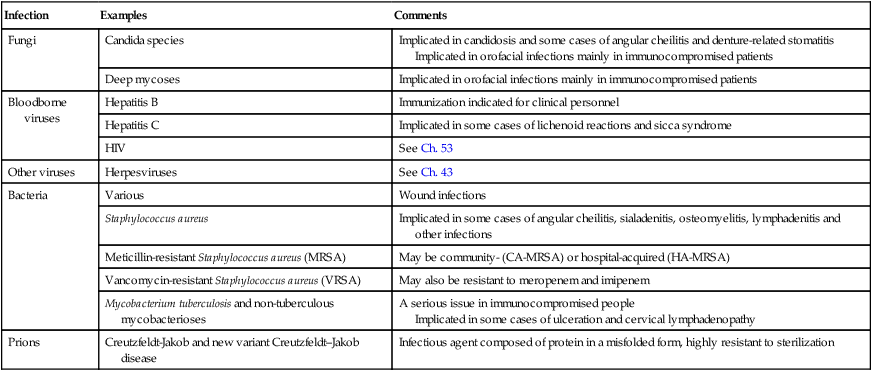
IATROGENIC INFECTIONS
Fortunately, iatrogenic infections apart from opportunistic infections, are uncommon in the practice of oral medicine. Opportunistic infections, such as candidosis and herpesvirus infections, are common in immunocompromised patients, or those treated with some agents causing hyposalivation, antimicrobials, and some topical corticosteroid and other agents. Tuberculosis is an increasing issue in immunocompromised people, and people on immunosuppressive drugs including those treated with biologic agents (Ch. 5). The blood-borne agents such as hepatitis viruses, HIV, syphilis and prions should not be transmitted if standard infection control procedures are implemented. Hospital acquired infections have thus far not been a major issue in oral medicine (Table 54.2).
Table 54.2
Some relevant iatrogenic infections
| Infection | Examples | Comments |
| Fungi | Candida species | Implicated in candidosis and some cases of angular cheilitis and denture-related stomatitis Implicated in orofacial infections mainly in immunocompromised patients |
| Deep mycoses | Implicated in orofacial infections mainly in immunocompromised patients | |
| Bloodborne viruses | Hepatitis B | Immunization indicated for clinical personnel |
| Hepatitis C | Implicated in some cases of lichenoid reactions and sicca syndrome | |
| HIV | See Ch. 53 | |
| Other viruses | Herpesviruses | See Ch. 43 |
| Bacteria | Various | Wound infections |
| Staphylococcus aureus | Implicated in some cases of angular cheilitis, sialadenitis, osteomyelitis, lymphadenitis and other infections | |
| Meticillin-resistant Staphylococcus aureus (MRSA) | May be community- (CA-MRSA) or hospital-acquired (HA-MRSA) | |
| Vancomycin-resistant Staphylococcus aureus (VRSA) | May also be resistant to meropenem and imipenem | |
| Mycobacterium tuberculosis and non-tuberculous mycobacterioses | A serious issue in immunocompromised people Implicated in some cases of ulceration and cervical lymphadenopathy |
|
| Prions | Creutzfeldt-Jakob and new variant Creutzfeldt–Jakob disease | Infectious agent composed of protein in a misfolded form, highly resistant to sterilization |
DRUG ADVERSE REACTIONS
It is important for the clinician to take a comprehensive drug history and always consider whether a drug may behind the clinical problem in question, since drugs can sometimes give rise to a range of adverse orofacial manifestations (Table 54.3), particularly salivary changes – notably hyposalivation, but also other features. Amongst the most common and important reactions and drugs implicated are:
Table 54.3
Main adverse drug effects in the orofacial region
| Effects | Examples | See Table | |
| Salivary changes | Hyposalivation | Tricyclic antidepressants | 54.4 |
| Salivary gland swelling or pain | Antihypertensives | 54.5 | |
| Sialorrhoea | Anticholinesterases | 54.6 | |
| Halitosis | Halitosis | Disulfiram | 54.7 |
| Taste disturbances | Taste acuity loss (hypogeusia) or distortion (dysgeusia) | Protease inhibitors | 54.8 |
| Mucosal | Burns | Caustics, such as lime Cocaine Aspirin Potassium tablets Pancreatic supplements Trichloracetic acid Hydrogen peroxide Sodium lauryl sulfate, |
|
| Aphthous-like ulceration | Cytotoxic agents Immunosuppressive agents Nicorandil NSAIDS |
54.9 | |
| Mucositis | Cytotoxic drugs especially methotrexate, 5-fluorouracil, doxorubicin, melphalan, mercaptopurine or bleomycin | 54.9 | |
| Candidosis | Corticosteriods Antibiotics |
54.10 | |
| Contact stomatitis or stomatitis venenata Granulomas Cosmetic fillers |
Antibiotics | 54.11 | |
| Lichenoid eruptions | Antimalarials Beta blockers NSAIDs Phenothiazines Sulfonylureas |
54.12 | |
| Erythema multiforme | Allopurinol Carbamazepine Barbiturates NSAIDs Protease inhibitors |
54.15 | |
| Pemphigoid | Furosemide | 54.13 | |
| Pemphigus | Rifampicin | 54.14 | |
| Lupus-like (lupoid) disorders | Hydralazine | 54.16 | |
| Discolouration and pigmentation | Amalgam Betel Chlorhexidine Crack cocaine Heavy metal salts Imatinib Tobacco |
54.17 | |
| Cheilitis | Contact cheilitis | Protease inhibitors Retinoids |
54.18 |
| Swellings | Gingival enlargement | Calcium channel blockers Ciclosporin Phenytoin |
54.19 |
| Angioedema | ACE inhibitors Aspirin Penicillins |
54.20 | |
| Neurological | Neuropathies | Protease inhibitors | 54.21 |
| Abnormal facial movements | Dopa Metoclopramide Phenothiazines |
54.22 | |
| Pain | ACE inhibitors Vinca alkaloids |
54.23 | |
| Burning sensation | ACE inhibitors Protease inhibitors |
54.24 | |
| Bruxism Trismus |
Ecstacy Metoclopramide |
54.25 | |
| Lymph nodes | Swelling | Carbamazepine Phenytoin |
54.26 |
| Tooth | Jaw development | Cytotoxic agents Phenytoin |
54.27 |
| Hypersensitivity | Hydrogen peroxide or carbamide peroxide | 54.28 | |
| Damage | Tetracyclines | 54.29 | |
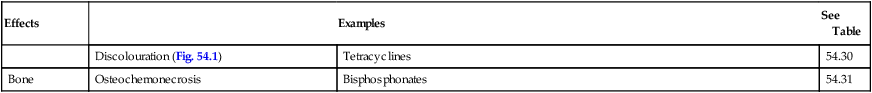
| Discolouration (Fig. 54.1) | Tetracyclines | 54.30 | |
| Bone | Osteochemonecrosis | Bisphosphonates | 54.31 |
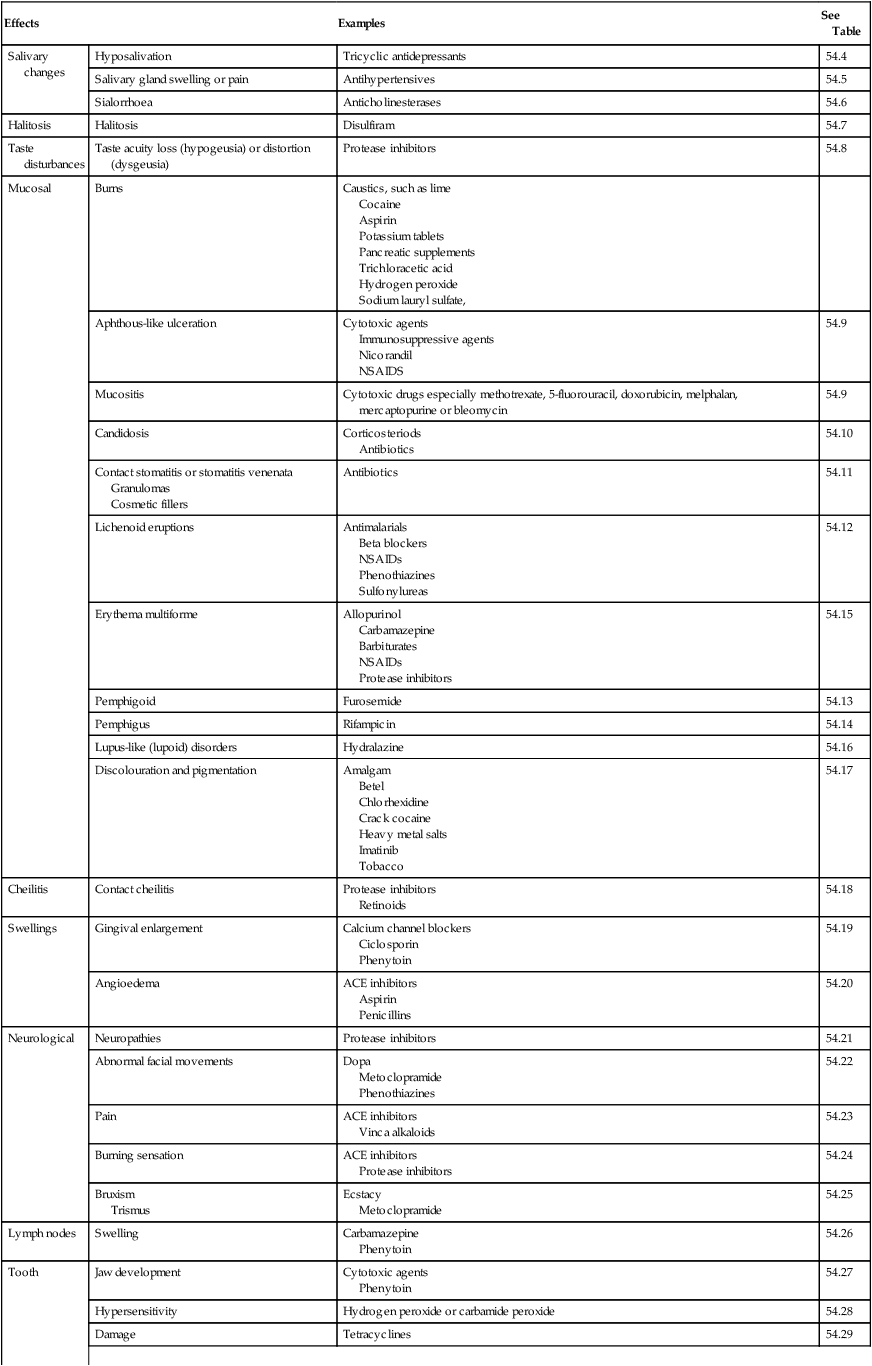
 Hyposalivation: antidepressants, antihypertensives, antihistamines and anticholinergics.
Hyposalivation: antidepressants, antihypertensives, antihistamines and anticholinergics.
 Swelling of gingiva: calcium channel blockers, ciclosporin and phenytoin.
Swelling of gingiva: calcium channel blockers, ciclosporin and phenytoin.
 Swelling of lips/face: ACE inhibitors, aspirin and penicillins.
Swelling of lips/face: ACE inhibitors, aspirin and penicillins.
 Erythema multiforme: allopurinol, barbiturates, NSAIDs and protease inhibitors.
Erythema multiforme: allopurinol, barbiturates, NSAIDs and protease inhibitors.
 Lichenoid lesions: antimalarials, beta-blockers, NSAIDs, phenothiazines and sulfonylureas.
Lichenoid lesions: antimalarials, beta-blockers, NSAIDs, phenothiazines and sulfonylureas.
 Ulceration/mucositis: barbiturates, cytotoxic agents (e.g. 5-fluorouracil, doxorubicin, and methotrexate), nicorandil, nonsteroidal antiinflammatory drugs (NSAIDs), sulfonamides and tetracyclines.
Ulceration/mucositis: barbiturates, cytotoxic agents (e.g. 5-fluorouracil, doxorubicin, and methotrexate), nicorandil, nonsteroidal antiinflammatory drugs (NSAIDs), sulfonamides and tetracyclines.
 Hyperpigmentation: antimalarials, cytotoxic agents, minocycline and zidovudine.
Hyperpigmentation: antimalarials, cytotoxic agents, minocycline and zidovudine.
The osteochemonecrosis resulting from bisphosphonates; adverse effects from recreational drugs; and opportunistic infections secondary to cytotoxic chemotherapy and increased prevalence of dysplastic and malignant lip and oral lesions in immunosuppressed patients and those using photosensitisers such as antihypertensive drugs are discussed below and in Ch. 31. Other possible reactions are shown in Tables 54.4–54.31.
Table 54.4
| Drugs most commonly implicated | Drugs occasionally implicated |
| Alpha receptor antagonists for treatment of urinary retention Anticholinergics Antidepressants (serotonin agonists, or noradrenaline and/or serotonin re-uptake blockers) Antipsychotics such as phenothiazines Atropinics Diuretics Muscarinic receptor antagonists for treatment of overactive bladder Protease inhibitors Radioiodine |
Amphetamines Antihistamines Antihypertensive agents Antimigraine agents Appetite suppressants Benzhexol Benzodiazepines, hypnotics, opioids and drugs of abuse Benztropine Biperiden Bronchodilators Bupropion Clonidine Cyclobenzaprine Cytokines Cytotoxics Decongestants and ‘cold cures’ Dideoxyinosine Diuretics Fenfluramine Fluoxetine Ganglion-blocking agents Histamine 2 antagonists and proton pump inhibitors Interleukin-2 Ipratropium Isotretinoin Leva-dopa Lithium Monoamine oxidase Omeprazole Opiates Orphenadrine Phenothiazines Propantheline Retinoids Selegiline Skeletal muscle relaxants Thiabendazole |
Table 54.5
Drug-related salivary gland swelling or pain
| Drugs most commonly implicated | Drugs occasionally implicated |
| Antihypertensives Chlorhexidine Cytotoxics Iodides |
Antithyroid agents Bretylium Cimetidine Clonidine Clozapine Deoxycycline Famotidine Ganglion-blocking agents Insulin Interferon Isoprenaline Methyldopa Naproxen Nifedipine Nitrofurantoin Oxyphenbutazone Phenothiazines Phenylbutazone Phenytoin Ranitidine Ritodrine Sulfonamides Trimepramine |
Table 54.6
Drug-related sialorrhoea/hypersalivation
| Drugs most commonly implicated | Drugs occasionally implicated |
| Anticholinesterases Clozapine |
Alprazolam Amiodarone Buprenorphine Buspirone Clonazepam Diazoxide Ethionamide Gentamicin Guanethidine Haloperidol Imipenem/cilastatin Iodides Kanamycin Ketamine Lamotrigine Leva-Dopa Mefenamic acid Mercurials Nicardipine Niridazole Nitrazepam Pentoxifylline Remoxipride Risperidone Rivastigmine Tacrine Tobramycin Triptorelin Venlafaxine Zaleplon |
Table 54.7
| Drugs most commonly implicated | Drugs occasionally implicated |
| Drugs causing hyposalivation | Dimethyl sulfoxide (DMSO) Disulfiram Isorbide dinitrate |
Table 54.8
Drug-related taste abnormalities
| Drugs most commonly implicated | Drugs occasionally implicated |
| Antithyroids Aurothiomalate Aztreonam Baclofen Biguanides Calcitonin Captopril Cilazapril Metronidazole Penicillamine Protease inhibitors |
Acarbose Acetazolamide Amitryptiline Aspirin Atrovastatin Ceftirizine Cisplatin Clidinium Clomipramine Cocaine Diazoxide Dicyclomine Enalapril Etidronate Fluoxetine Fluvoxamine Histone deacetylase inhibitors Imatinib Indometacin Isotretinoin Leva-dopa Losartan Pentamidine Phenytoin Propantheline Rifabutin Rivastigmine Sorafenib Spironolactone Topiramate Venlafaxine |
Table 54.9
| Drugs most commonly implicated | Drugs occasionally implicated |
| Cytotoxics Immunosuppressive agents Nicorandil NSAIDs, e.g. Indometacin |
Alendronate Aurothiomalate Aztreonam Captopril Clarithromycin Cocaine Dapsone Emepromium Everolimus Gold Interferons Isoprenaline Losartan Mycophenolate mofetil Naproxen Olanzapine Pancreatin Penicillamine Phenindione Phenylbutazone Phenytoin Potassium chloride Proguanil Protease inhibitors Sertraline Sirolimus Spironolactone Sulfonamides Tetracyclines |
Table 54.10
| Drugs most commonly implicated | Drugs occasionally implicated |
| Broad-spectrum antimicrobials Corticosteroids Cytotoxics Drugs causing hyposalivation Immunosuppressives |
– |
Table 54.11
Drug-related contact stomatitis (stomatitis venenata)
| Drugs most commonly implicated | Drugs occasionally implicated |
| Anaesthetics Antibiotics Antiseptics Barbiturates Dentifrices Mouthwashes Phenacetin Sulfonamides Tetracyclines |
Chewing gum Cosmetics Dental materials |
Table 54.12
Drug-related lichenoid reactions
| Drugs most commonly implicated | Drugs occasionally implicated |
| Antihypertensives Antimalarials NSAIDs |
ACE inhibitors Amiphenazole Beta blockers Captopril Carbamazepine Carbimazole Chloroquine Chlorpropamide Cimetidine Clofibrate Daclizumab Dapsone Dipyridamole Ethionamide Gaunoclor Gold Griseofulvin Labetalol Lincomycin Lithium Mepacrine Mercury (amalgam) Metformin Methyldopa Metronidazole Niridazole Oxprenolol Para-aminosalicylate Penicillamine Phenindione Phenothiazines Practolol Propranolol Prothionamide Quinidine Quinine Streptomycin Sulfonamides Tetracycline Thiazides Tolbutamide Triprolidine |
Table 54.13
Drug-related pemphigoid-like reactions
| Drugs most commonly implicated | Drugs occasionally implicated |
| Furosemide Penicillamine NSAIDs |
Captopril Clonidine Sulfonamides |
Table 54.14
Drug-related pemphigus-like reactions
| Drugs most commonly implicated | Drugs occasionally implicated |
| Diclofenac Penicillamine Rifampicin |
Captopril Cephalexin Ethambutol Glibenclamide Ibuprofen Penicillamine Practolol |
Table 54.15
Drug-related erythema multiforme (and Stevens–Johnson syndrome and toxic epidermal necrolysis)
| Drugs most commonly implicated | Drugs occasionally implicated |
| Allopurinol Anticonvulsants Barbiturates Carbamazepine Co-trimoxazole Hydantoins NSAIDs Penicillin Phenytoin Sulfonamides |
Adalimumab Bupropion Candesartan Busulphan Cephalosporins Chlorpropamide Clindamycin Codeine Ethambutol Furosemide Gold Metformin Minoxidil Oestrogens Phenothiazines Phenylbutazone Progestogens Protease inhibitors Quinolones Rifampicin Tetracyclines Tolbutamide Vancomycin Verapamil |
Table 54.16
| Drugs most commonly implicated | Drugs occasionally implicated |
| Hydralazine Procainamide |
Ethosuximide Gold Griseofulvin Isoniazid Methyldopa Para-aminosalicylate Penicillin Phenothiazines Phenytoin Streptomycin Sulfonamides Tetracyclines |
Table 54.17
Drug-related oral mucosal pigmentation
| Drugs most commonly implicated | Drugs occasionally implicated |
| Amalgam Chlorhexidine Smoking/tobacco |
ACTH Amiodarone Amodiaquine Anticonvulsants Arsenic Betel Bismuth Bromine Busulphan Chlorhexidine Chloroquine Clofazimine Coal Copper Cyclophosphamide Doxorubicin Gold Heroin Hydroxycarbamide Hydroxychloroquine Imatinib mesylate Iron Ketoconazole Lead Manganese Menthol Mepacrine Methyldopa Minocycline Oral contraceptives Palifermin Phenolphthalein Phenothiazines Quinacrine Quinidine Silver Thallium Tin Vanadium Zidovudine |
Table 54.18
| Drugs most commonly implicated | Drugs occasionally implicated |
| Etretinate Indinavir Isotretinoin Protease inhibitors Vitamin A |
Atrovastatin Busulphan Clofazimine Clomipramine Cyancobalamin Gold Methyldopa Psoralens Streptomycin Sulfasalazine Tetracycline |
Table 54.19
Drug induced gingival overgrowth (DIGO)
| Drugs most commonly implicated | Drugs occasionally implicated |
| Amlodipine Ciclosporin Diltiazem Felodipine Lacidipine Nifedipine Oral contraceptives Phenytoin Verapamil |
Amphetamines Cotrimoxazole Erythromycin Ethosuximide Ketoconazole Lamotrigine Lithium Phenobarbitone Primidone Sertraline Topiramate Valproate Vigabatrin |
Table 54.20
| Drugs most commonly implicated | Drugs occasionally implicated |
| ACE inhibitors Aspirin Penicillin Sulfonamides |
Angiotensin II antagonists Antidepressants Bupropion Clindamycin COX-II inhibitors Droperidol Mianserin NSAIDs Proton pump inhibitors Statins SSRIs Vaccines |
Table 54.21
Drug-related trigeminal paraesthesia or hypoaesthesia
| Drugs most commonly implicated | Drugs occasionally implicated |
| Acetazolamide Articaine Labetalol Protease inhibitors Vincristine |
Amitryptiline Chlorpropamide Colistin Ergotamine Gonadotropin-releasing hormone analogues Hydralazine Interferon alpha Isoniazid Mefloquine Methotrexate Methysergide Monoamine oxidase inhibitors Nalidixic acid Nicotinic acid Nitrofurantoin Pentamidine Phenytoin Prilocaine Propofol Propranolol Stilbamidine Streptomycin Sulfonylureas Sulthiame Tolbutamide Tricyclics Trilostane |
Table 54.22
Drug-related involuntary facial movements
| Drugs most commonly implicated | Drugs occasionally implicated |
| L-dopa Metoclopramide Phenothiazines |
Butyrophenones Carbamazepine Ecstacy Lithium Methamphetamine Methyldopa Metirosine Phenytoin Tricyclic antidepressants Trifluoroperazine |
Table 54.23
| Drugs most commonly implicated | Drugs occasionally implicated |
| ACE inhibitors Nitrites Vinca alkaloids |
Benztropine Biperidin Griseofulvin Lithium Penicillins Phenothiazines Stilbamidine Ticarcillin Vitamin A |
Table 54.24
| Drugs most commonly implicated | Drugs occasionally implicated |
| Cytotoxic drugs ACE inhibitors HRTProtease inhibitors Proton pump inhibitors |
Antidepressants Clonazepam |
Table 54.25
Drug-related bruxism or trismus
| Drugs most commonly implicated | Drugs occasionally implicated |
| Ecstacy | Duloxetin Fluoxetine Metoclopramide Phenothiazines Pregabalin Propofol Suxamethonium Tricyclic antidepressants |
Table 54.26
Drug induced gingival hypersensitivity
| Drugs most commonly implicated | Drugs occasionally implicated |
| Allopurinol Carbamazepine Lamotrogine Phenobarbitone Phenytoin Sulfasalazine Sulfonamides |
Abacavir Atenolol Azathioprine Captopril Dapsone Diltiazem Gold salts Isoniazid Mexiletine Minocycline Nevirapine Oxicam Trimethoprim |
Table 54.27
Drugs used in pregnancy that may induce cleft palate
| Drugs most commonly implicated | Drugs occasionally implicated |
| Alcohol Anticonvulsants Cocaine Fluconazole Heroin Phenytoin Retinoids Tobacco Topiramate |
Antihypertensives Corticosteroids Cytotoxic agents Thalidomide |
Table 54.28
Drugs that may induce tooth hypersenstitivity
| Drug | Examples |
| Tooth whiteners | Carbamide peroxide Hydrogen peroxide |
Table 54.29
Drugs that may lead to tooth structure damage
| Drug | Examples | Possible damage to tooth structure |
| Sugar-containing oral (liquid) medication | Various | Caries |
| Drugs that result in decreased salivary secretion (hyposalivation) | See Table 54.4 | Caries |
| Drugs with a low pH | Aspirin, antiasthmatic drugs | Erosion |
| Drugs causing gastro-oesophageal reflux | Theophylline, anticholinergics, progesterone, calcium channel blockers, antiasthmatics | Erosion |
| Drugs inducing bruxism | Dopamine agonists, dopamine antagonists, tricyclic antidepressants, selective serotonin reuptake inhibitors, alcohol, cocaine, amphetamines | Attrition |
| Drugs used for internal tooth bleaching | Hydrogen peroxide and sodium perborate | Cervical root resorption |
| Drugs used for treatment of childhood cancers | Cytotoxic agents | Abnormal dental development |
| Anticonvulsants | Phenytoin | Abnormal dental development |
| Fluorides | Any | Fluorosis |
Table 54.30
Drug-related extrinsic tooth discolouration
| Drugs most commonly implicated | Drugs occasionally implicated |
| Chlorhexidine Ciprofloxacin Fluorides Iron Tetracyclines |
Antibiotics Clarithromycin Enalapril Essential oil Etidronate Fosinopril Imipenem Lisinopril Metronidazole Penicillin Pentamidine Perindopril Propafenone Quinapril Ramipril Terbinafine Trandolopril Zopiclone |
Table 54.31
| Drugs most commonly implicated | Drugs occasionally implicated |
| Bisphosphonates | Denosumab Bevacizumab Sunitinib |
OSTEOCHEMONECROSIS
Aetiology and pathogenesis
BPs act especially by blocking the osteoclast HMG-CoA reductase (mevalonate) path, inhibiting the cell activities, as well as directly inhibiting osteogenesis in bone-healing. BPs remain in bone and exert these effects for many years or even decades. Risk factors for BRONJ include systemic and local factors (Table 54.32), especially tooth extraction.
Table 54.32
Risk factors for osteochemonecrosis
| Systemic risk factors | Local risk factors |
| Duration of BP exposure i.v. administration Potent nitrogen-containing BPs (i.e. zoledronate, pamidronate and ibandronate) Smoking Diabetes mellitus Rheumatoid arthritis CYP2C8 gene diversity or reduced interleukin-17 Possibly chemotherapeutic agents, thalidomide, or bortezomib Denosumab (monoclonal antibody for treating osteoporosis) |
Dental extractions: increase risk at least 16-fold and up to 44-fold Denture wearing: an almost 5-fold increased risk for patients taking zoledronate and also wearing dentures Periodontal disease: as a risk factor remains controversial |
Prevention
Prevention of BRONJ is fundamental, since no cure is known, and should include:
 Patient counselling about risks.
Patient counselling about risks.
 Avoiding elective oral surgery: including extractions or endosseous implant placement, or carrying out the treatment well before commencing BPs, or after a 6-month drug holiday.
Avoiding elective oral surgery: including extractions or endosseous implant placement, or carrying out the treatment well before commencing BPs, or after a 6-month drug holiday.
 Preventive measures (dental screening, all dental work done at least 6 weeks before starting BPs) can produce a three-fold reduction of BRONJ related to zoledronate in myeloma patients. One protocol suggested to prevent BRONJ includes the raising of a flap before tooth extraction associated with a broad-spectrum antibiotic started three days before, and advancing the flap for primary closure.
Preventive measures (dental screening, all dental work done at least 6 weeks before starting BPs) can produce a three-fold reduction of BRONJ related to zoledronate in myeloma patients. One protocol suggested to prevent BRONJ includes the raising of a flap before tooth extraction associated with a broad-spectrum antibiotic started three days before, and advancing the flap for primary closure.
 Serum collagen telopeptide (CTX) levels: a reliable index of bone turnover rates might predict BRONJ risk but this is controversial. Perhaps CTX monitoring could help determine the best timing for a ‘drug holiday’.
Serum collagen telopeptide (CTX) levels: a reliable index of bone turnover rates might predict BRONJ risk but this is controversial. Perhaps CTX monitoring could help determine the best timing for a ‘drug holiday’.
RECREATIONAL DRUGS
Although not causing iatrogenic disease, a range of recreational drugs can damage the orofacial region (Table 54.33)
Table 54.33
Maxillofacial consequences of use of specific recreational drugs
| Drug | Possible complications |
| Alcohol | Leukoplakia, carcinoma, tooth erosion, glossitis/oral ulcers/angular stomatitis from malnutrition, sialosis, foetal alcohol syndrome |
| Amphetamine | Picking at the face, bruxism, hyposalivation and increased caries incidence ‘Meth mouth’ is the term given to the neglect and poor oral hygiene seen in methamphetamine users |
| Barbiturates | Facial pain, bullous reactions |
| Betel | Submucous fibrosis, leukoplakia, carcinoma |
| Cannabis | White lesions (burns), hyposalivation, possible leukoplakia, carcinoma |
| Cocaine | Temporarily numbness of lips and tongue, gingival erosions, dry mouth, bruxism dental erosion Caries and periodontal disease, especially acute necrotizing gingivitis, are more frequent Cocaine may precipitate cluster headaches Oronasal fistulae |
| Ecstasy | Tooth clenching, bruxism, TMJ dysfunction, dry mouth, attrition, dental erosion, mucosal burns or ulceration, circumoral paraesthesiae and periodontitis |
| Khat | Leukoplakia, carcinoma |
| Nicotine | Due to tobacco: leukoplakia, carcinoma, dry socket, necrotizing gingivitis, periodontitis, impaired wound healing and implant success |
| Opiates | Hyposalivation |
| Solvents | Perioral dermatitis, foetal gasoline/petrol syndrome |
CANCER THERAPY AND COMPLICATIONS
See Ch. 31 and Table 54.34.
Table 54.34
Orofacial complications of cancer therapy
| Therapy | Oral complications |
| Radiotherapy | Pain, mucositis, hyposalivation, candidosis, caries, sialadenitis, osteoradionecrosis, fibrosis |
| Chemotherapy | Pain, mucositis, hyposalivation, candidosis, herpesviruses, neuropathy |
| Surgery | Pain, neuropathy, disfigurement, impaired speech and swallowing Scarring Carotid blow-out (haemorrhage), chyle leakage, salivary leakage |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


















