The common aspect of all granulomatous diseases is the typical form of chronic inflammatory response with distinct microscopic granulomas that are formed secondary to either definitive etiologic agents, like bacteria, fungal, or parasitic, or due to an unknown etiologic agent, such as trauma, autoimmune, or even neoplastic process. Although they can be histologically distinct, granulomatous diseases demonstrate a variety of clinical features that may not seem to be inflammatory. Two types of granulomas are typically encountered: foreign body granulomas and immune granulomas. The differences between the two types of granulomas lie in the pathogenesis.
Key points
- •
Identification of oral granulomatous lesions clinically and radiographically with histologic confirmation for a definitive diagnosis is the standard strategy.
- •
On occasion, the interventions can be undertaken by clinical and radiographic diagnosis alone to curtail the spread of the infection.
- •
As oral granulomatous lesions are rare, a thorough understanding of the mechanisms involved in the production of clinical symptoms is essential to identify these lesions at an early stage.
Infections
Tuberculosis
Tuberculosis (TB) is an airborne disease caused by the bacterium Mycobacterium tuberculosis . It spreads through air droplets. It mainly affects the respiratory tract and lungs via the nasal passage ( Table 1 ).
| Category/Disease | Etiologic Agent |
|---|---|
| Infections | |
| Bacterial infections | |
| TB | Mycobacterium tuberculosis |
| Leprosy | Mycobacterium leprae |
| Actinomycosis | Actinomyces israelii |
| Rhinoslceroma | Klebsiella rhinoscleromatis |
| Anthrax | Bacillus anthracis |
| Brucellosis | Brucella melitensis |
| Syphilis | Treponema pallidum |
| Fungal infections | |
| Histoplasmosis | Histoplasma capsulatum |
| Blastomycosis | Blastomyces dermatitidis |
| Phycomycosis | Basidiobolus haptosporus |
| Aspergillosis | Aspergillus |
| Cryptococcosis | Cryptococcus neoformans |
| Rhinosporidiosis | Rhinosporidium seeberi |
| Parasitic infection | |
| Leishmaniasis | Leishmania (through sandfly) |
| Myiasis | Chrysomya bezziana |
| Toxoplasmosis | Toxoplasma gondii |
| Traumatic cause | |
| Pyogenic granulomas | Trauma and local factors |
| Reparative granulomas | Trauma or inflammation |
| Foreign body cause | |
| Oral foreign body reaction | Inflammation |
| Cholesterol granulomas | Eustachian tube dysfunction |
| Cocaine-induced midline granulomas | Inflammation and necrosis |
| Gout | Excess uric acid |
| Neoplastic | |
| Langerhans cell histiocytosis (LCH) | Malignancy |
| Necrotizing sialometaplasia | Inflammation, trauma, reactive |
| Polymorphic reticulosis (lethal midline granulomas) | Epstein-Barr virus |
| Unknown cause | |
| Sarcoidosis | Unknown |
| Crohn diseases | Unknown |
| Autoimmune and vascular diseases | |
| Wegener granulomatosis | Autoimmune |
| Systemic lupus erythematosus | Autoimmune |
| Sjögren syndrome | Autoimmune |
| Developmental | |
| Melkersson-Rosenthal syndrome (orofacial granulomatosis) | Developmental |
Clinical features
Primary TB is associated with episodic fever, chills, fatigability, malaise, gradual loss of weight, and a persistent cough, which may be dry or productive. Secondary TB presents with fever, cough, chest pain, and hemoptysis. Military TB shows symptoms of acute febrile illness in children. However, in adults, it is insidious with gradual development of ill health, anorexia, loss of weight, and fever.
Tuberculous lymphadenitis may progress to the formation of an actual abscess or remain as granulomatous infection. They are tender because of inflammation of the overlying skin with perforation and pus discharge. More than 50% of the patients with AIDS have extrapulmonary TB lesions.
Oral manifestations
Direct contact with infected sputum is the most common route. There are other routes of infections, such as lymphatic spread, hematogenous spread, and extension from the involved neighboring tissues. The resulting oral lesions present as ulcers, nodules, tuberculomas, and apical granulomas.
Histopathologic features
Areas of infection demonstrate the formation of granulomas, circumscribed by collections of epithelioid histiocytes, lymphocytes, and multinucleated giant cells with central caseous necrosis. These granulomas are called as tubercles.
Radiographic features
There are 3 patterns of nodal involvement in tuberculous lymphadenitis on CT or MRI.
- •
Nodes are homogeneous in attenuation or signal intensity and enhance homogenously after the injection of contrast material in the early phase of the disease.
- •
A node with a central area of necrosis is seen as the disease progresses.
- •
A fibrocalcified node is usually seen in patients who have been treated for TB.
TB of the nose and paranasal sinuses in CT or MRI demonstrates nasal soft tissue nodules and thickening and involvement of the paranasal sinuses.
Typically tuberculous osteomyelitis with mandibular involvement shows radiographic features that include osteopenia and poorly defined lytic lesions with minimal surrounding sclerosis.
Dental considerations
The following Centers for Disease Control and Prevention recommendations apply to patients who are known or suspected to have active TB and should be adopted by every dentist.
- •
Evaluate patients away from other patients and dental team members. When they are not being evaluated, patients should wear a surgical mask or be instructed to cover their mouth and nose when coughing or sneezing.
- •
Defer elective dental treatment until patients are noninfectious as confirmed by a physician.
- •
Refer patients requiring urgent dental treatment to a previously identified facility (such as a hospital) with TB engineering controls and a respiratory protection program.
Leprosy
Leprosy, also known as Hansen disease, is a chronic infectious disease mainly caused by Mycobacterium leprae . This organism requires a cold host body temperature for endurance.
Clinical features
Clinical presentations of leprosy could be in one of the 2 known forms: (1) tuberculoid leprosy and (2) lepromatous leprosy.
Tuberculoid leprosy develops in patients with high immune reactions. Lepromatous leprosy is seen in patients with reduced cell-mediated immunity.
Paucibacillary leprosy
Small number of well-circumscribed, hypopigmented skin lesions will be noted. Nerve involvement resulting in anesthesia of the affected skin is observed. Oral lesions are rare in this variant.
Multibacillary leprosy
Numerous ill-defined hypopigmented macules or papules may be noted on the skin and becomes thickened with time. Skin enlargements can lead to distorted facial appearance, that is, leonine facies. Nerve involvement leads to loss of sweating and decreased sensations of light, touch, pain, and temperature. Sensory loss begins in the extremities and spreads to most of the body.
Oral manifestations
Oral soft tissue lesions initially present as yellowish to red, sessile, firm, enlarging papules that develop ulceration and necrosis ( Fig. 1 ). Deep infiltration of the soft tissue involvement leads to bone destruction.
- •
Atrophy of the anterior nasal spine
- •
Atrophy of the anterior maxillary alveolar ridge
- •
Endonasal inflammatory changes

Teeth show enamel hypoplasia and short tapering roots with internal resorption. Facial and trigeminal nerves can be involved with the infectious process. Involvement of the tongue is not uncommon with indurated areas ( Fig. 2 ). Oral erosive lesions and ulcerations can also be noted within the oral cavity ( Fig. 3 ).


Histopathological features
There are well-formed granulomas with clusters of epithelioid histiocytes, lymphocytes, and Langhans-type multinucleated giant cells. There is a lepromatous pattern with sheets of lymphocytes intermixed with vacuolated histiocytes known as lepra cells. An abundance of organisms can be demonstrated with acid-fast stains in the lepromatous variant.
Radiographic features
Facies leprosa are better visualized in lateral cephalometric radiographs because of the deficiency of the premaxillary region. Shortening of roots of the maxillary anterior teeth in a panoramic radiograph have also been reported. Gallium 67 citrate scintigraphy may be used to detect active multibacillary forms of leprosy. When gallium is used to estimate skin involvement, it is not uncommon to see a moderate to diffuse uptake of the radiopharmaceutical in the skin producing a skin outlining sign. The uptake is very important for the skin where the lepromas are commonly seen.
Dental management
Although patients with leprosy will first report to the dermatologist and rarely to the dental professional, the dental professional should be well aware of the precautions to be taken while giving any kind of treatment to these patients in a leprosy center. Appropriate treatment of dental infections will help to reduce the recurrence in leprosy reactions, as will improving the general oral hygiene of patients. Further, it is thought that oral lesions, along with nasal lesions, form an important source of bacillary dissemination in the community. Oral health status of individuals treated and healed from leprosy is poor. Better methods of oral hygiene and regular dental monitoring should be adopted in order to improve the quality of life of these patients.
Actinomycosis
Chronic granulomatous and fibrosing disease caused by Actinomyces israelii . It is chiefly characterized by the formation of abscesses that tend to drain by the formation of the sinus tract.
In 1938 Cope classified it into 3 types depending on the location:
- •
Cervicofacial
- •
Abdominal
- •
Pulmonary forms
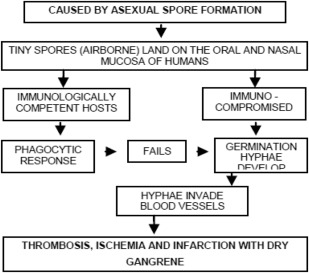
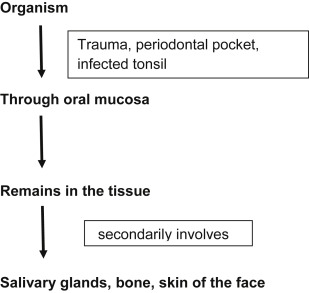
Pathogenesis
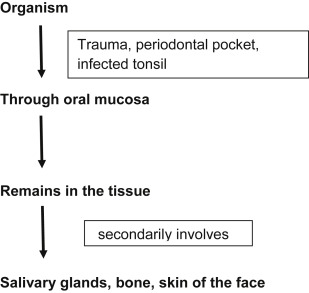
Oral manifestations
Hyperpyrexia is noted, with the presence of regional lymphadenopathy in late stages of the disease. Swelling and indurations of the soft tissue may be noted. Later it may develop into abscesses that tend to discharge pus containing the typical sulfur granules . There are multiple sinus openings. Common sites for multiple sinus openings are mandibular or maxillary bone, which lead to actinomycotic osteomyelitis.
Histopathologic features
Histological specimen stains with hematoxylin. There is central abscess formation noted with characteristic colonies of microorganisms within it. The colonies seem to be floating in a sea of polymorphonuclear leukocytes, associated with multinucleated giant cells and macrophages at the periphery of the lesion. The eosinophilic club-shaped ends of the A israelii filaments are the basis for the term ray fungus .
Radiographic findings
Computed tomographic (CT) findings include the following:
- •
Cervico-facial actinomycosis is an enhancing soft tissue mass with a low-attenuating center associated with inflammatory change in the adjacent soft tissue. Invasion of the adjacent soft tissue, including the muscles, can occur.
- •
Actinomycotic osteomyelitis of the jaws presents as an irregularly marginated lesion with increased bone marrow attenuation, osteolysis, and involvement of the skin in all patients. Periosteal reaction and intralesional gas can also be seen in patients.
T1- and T2-weighted MRI show intermediate signal intensity associated with moderate contrast enhancement. This characteristic signal intensity may be associated with the histologic feature of abundant granulation and fibrous tissue in actinomycosis. Popcornlike dystrophic calcification can also be seen occasionally.
Extensive soft tissue inflammatory and infiltrative changes in the surrounding soft tissues extending to the skin may be useful in the differentiation of actinomycosis from osteomyelitis due to other causes.
Dental management
Initially, attempts are made to treat actinomycosis, including extensive disease, with aggressive antimicrobial therapy alone. Surgery is indicated to take a biopsy specimen, to drain abscesses, and to extirpate (wide excision) a fibrotic sinus tract. Follow-up should be adequate and meticulous to have a complete cure of the disease.
Klebsiella rhinoscleromatis Infection
It is a chronic, slowly progressive, localized infection caused by Klebsiella rhinoscleromatis . It is commonly seen in the upper respiratory tract, often originating in the nose.
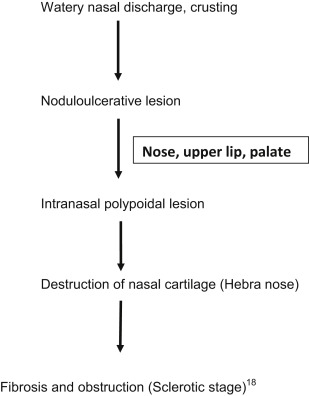
Clinical features
Common sites will be lacrimal glands, orbit, skin, and paranasal sinuses. It shows features, such as exudative, proliferative, and fibrotic (cicatrical).
Exudative phase
Oral manifestations
Impairment of the sensation of taste, anesthesia of the soft palate, and enlargement of the uvula and upper lip are observed.
Histopathologic features
There is a nonspecific inflammatory reaction with polymorph nuclear cells and dense plasma cell infiltration. Also noted are the Mikulicz cells: large foamy histiocytes, that is, macrophages with a size of up to 100 mm that are unable to digest phagocytosed bacteria, which persist in massively enlarged vacuoles. The sclerotic stage is characterized by granulomatous masses that result from scarring of chronically infected upper airways.
Radiographic features
CT scan of the neck shows a big air pocket in the parapharyngeal spaces. These findings are suggestive of a developing abscess. Gas-forming brain abscesses have been reported to result from escape of air into the cranium due to skull fracture or gas-forming organisms.
Anthrax
Anthrax is caused by Bacillus anthracis . In cutaneous anthrax, it clinically appears as coal-like black lesions found on the skin.
Clinical features
The spectrum of disease ranges from asymptomatic to severe, terminating in sepsis, septic shock, and death. Oropharyngeal anthrax lesions are generally localized in the oral cavity, especially on the buccal mucosa, tongue, tonsils, or posterior pharynx wall. The characteristic oral lesion is generally 2 to 3 cm in diameter and covered with a gray pseudomembrane surrounded by extensive edema. The main clinical features are sore throat, dysphagia, and painful regional lymphadenopathy in the involved side of the neck. The illness may progress rapidly, and edema around lymph nodes may result in extensive swelling of the neck and anterior chest wall. The overt infection leads to toxemia, acute respiratory distress, and alteration in mental state.
Histopathologic features
Gram-stained smear from the lesion reveals polymorphonuclear leukocytes and gram-positive bacilli, and the culture may be positive for B anthracis .
Radiographic features
- •
Disease manifests as pleural effusions, mediastinal widening, and, rarely, pneumonia. Mediastinal widening with high-attenuation mediastinal and hilar lymph nodes on CT in the absence of trauma, dissection, or bleeding diathesis is suspicious.
Brucellosis
It is a multisystem disorder with a broad spectrum of nonspecific symptoms. Brucellosis manifests as an acute febrile illness that may persist and progress to a chronically incapacitating disease with severe complications. Bone and joint involvement is the most frequent complication of brucellosis, occurring in up to 40% of cases.
Syphilis
Syphilis is caused by Treponema pallidum and is characterized by episodes of active disease interrupted by periods of latency. It can be either acquired or congenital. The acquired form is contracted as a venereal disease and if untreated manifests 3 distinctive stages throughout its course: primary, secondary, and tertiary stages.
Oral manifestations
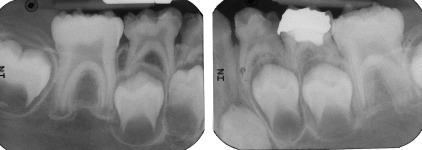
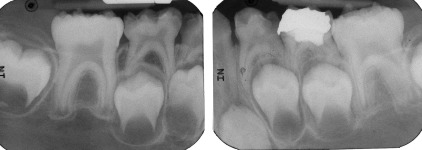
The primary lesion is an elevated, ulcerated nodule that shows indurations and produces regional lymphadenopathy. The intraoral chancre can be appreciated. The secondary stage produces multiple, painless, grayish-white plaques overlying an ulcerated surface and are called mucous patches. Several adjacent mucous patches fuse to form a serpentine or snail-track pattern. Commonly involved sites include the tongue, gingiva, and buccal mucosa. Occasionally papillary lesions resembling viral papillomas may arise called as condylomata lata. Late congenital syphilis is diagnosed by clinical history, distinctive physical signs, and a positive serologic test. The Hutchinson triad of interstitial keratitis, Hutchinson incisors ( Figs. 4 and 5 ), and eighth cranial nerve deafness are diagnostic.

Histopathologic features
The primary lesions show ulcerated surface epithelium with several vascular channels and intense chronic inflammatory infiltrate in the underlying lamina propria. The inflammatory infiltrate is chiefly composed of lymphocytes and plasma cells and demonstrates a perivascular pattern. In the secondary stages, the epithelium demonstrates hyperplasia with significant spongiosis and exocytosis. Tertiary lesions exhibit peripheral pseudoepitheliomatous hyperplasia. The foci of granulomatous inflammation with well-circumscribed collections of histiocytes and multinucleated giant cells can be observed.
Radiographic features
- •
Syphilitic osteomyelitis causes osteolytic changes in the cortex and medullary space, usually with an aggressive pattern of bone destruction compared with other types of osteomyelitis that occur in jaws. Sequestra in syphilis are difficult to visualize radiographically because they are small and usually occur in cancellous bone. It should be stressed that the destructive lesions in early acquired syphilis are those of osteomyelitis and do not represent gummas. MRI demonstrates marrow space involvement, periosteal process, and a degree of intracranial extension more completely than CT.
- •
Proliferative periostitis has been well described in secondary syphilis and is most commonly seen in the tibiae, skull, clavicles, ribs, and sternum. Scintigraphy is a sensitive means of detection in subtle cases and can be useful in the determination of the extent of disease for guiding bone biopsy.
- •
Syphilitic gummas in CT may present as hypodense with no contrast enhancement or mass effect or as densely enhancing masses with surrounding edema. Magnetic resonance (MR) descriptions have included lesions hypointense to isointense on T1-weighted images and hyperintense on T2-weighted images, associated with homogeneous contrast enhancement.
Infections
Tuberculosis
Tuberculosis (TB) is an airborne disease caused by the bacterium Mycobacterium tuberculosis . It spreads through air droplets. It mainly affects the respiratory tract and lungs via the nasal passage ( Table 1 ).
| Category/Disease | Etiologic Agent |
|---|---|
| Infections | |
| Bacterial infections | |
| TB | Mycobacterium tuberculosis |
| Leprosy | Mycobacterium leprae |
| Actinomycosis | Actinomyces israelii |
| Rhinoslceroma | Klebsiella rhinoscleromatis |
| Anthrax | Bacillus anthracis |
| Brucellosis | Brucella melitensis |
| Syphilis | Treponema pallidum |
| Fungal infections | |
| Histoplasmosis | Histoplasma capsulatum |
| Blastomycosis | Blastomyces dermatitidis |
| Phycomycosis | Basidiobolus haptosporus |
| Aspergillosis | Aspergillus |
| Cryptococcosis | Cryptococcus neoformans |
| Rhinosporidiosis | Rhinosporidium seeberi |
| Parasitic infection | |
| Leishmaniasis | Leishmania (through sandfly) |
| Myiasis | Chrysomya bezziana |
| Toxoplasmosis | Toxoplasma gondii |
| Traumatic cause | |
| Pyogenic granulomas | Trauma and local factors |
| Reparative granulomas | Trauma or inflammation |
| Foreign body cause | |
| Oral foreign body reaction | Inflammation |
| Cholesterol granulomas | Eustachian tube dysfunction |
| Cocaine-induced midline granulomas | Inflammation and necrosis |
| Gout | Excess uric acid |
| Neoplastic | |
| Langerhans cell histiocytosis (LCH) | Malignancy |
| Necrotizing sialometaplasia | Inflammation, trauma, reactive |
| Polymorphic reticulosis (lethal midline granulomas) | Epstein-Barr virus |
| Unknown cause | |
| Sarcoidosis | Unknown |
| Crohn diseases | Unknown |
| Autoimmune and vascular diseases | |
| Wegener granulomatosis | Autoimmune |
| Systemic lupus erythematosus | Autoimmune |
| Sjögren syndrome | Autoimmune |
| Developmental | |
| Melkersson-Rosenthal syndrome (orofacial granulomatosis) | Developmental |
Clinical features
Primary TB is associated with episodic fever, chills, fatigability, malaise, gradual loss of weight, and a persistent cough, which may be dry or productive. Secondary TB presents with fever, cough, chest pain, and hemoptysis. Military TB shows symptoms of acute febrile illness in children. However, in adults, it is insidious with gradual development of ill health, anorexia, loss of weight, and fever.
Tuberculous lymphadenitis may progress to the formation of an actual abscess or remain as granulomatous infection. They are tender because of inflammation of the overlying skin with perforation and pus discharge. More than 50% of the patients with AIDS have extrapulmonary TB lesions.
Oral manifestations
Direct contact with infected sputum is the most common route. There are other routes of infections, such as lymphatic spread, hematogenous spread, and extension from the involved neighboring tissues. The resulting oral lesions present as ulcers, nodules, tuberculomas, and apical granulomas.
Histopathologic features
Areas of infection demonstrate the formation of granulomas, circumscribed by collections of epithelioid histiocytes, lymphocytes, and multinucleated giant cells with central caseous necrosis. These granulomas are called as tubercles.
Radiographic features
There are 3 patterns of nodal involvement in tuberculous lymphadenitis on CT or MRI.
- •
Nodes are homogeneous in attenuation or signal intensity and enhance homogenously after the injection of contrast material in the early phase of the disease.
- •
A node with a central area of necrosis is seen as the disease progresses.
- •
A fibrocalcified node is usually seen in patients who have been treated for TB.
TB of the nose and paranasal sinuses in CT or MRI demonstrates nasal soft tissue nodules and thickening and involvement of the paranasal sinuses.
Typically tuberculous osteomyelitis with mandibular involvement shows radiographic features that include osteopenia and poorly defined lytic lesions with minimal surrounding sclerosis.
Dental considerations
The following Centers for Disease Control and Prevention recommendations apply to patients who are known or suspected to have active TB and should be adopted by every dentist.
- •
Evaluate patients away from other patients and dental team members. When they are not being evaluated, patients should wear a surgical mask or be instructed to cover their mouth and nose when coughing or sneezing.
- •
Defer elective dental treatment until patients are noninfectious as confirmed by a physician.
- •
Refer patients requiring urgent dental treatment to a previously identified facility (such as a hospital) with TB engineering controls and a respiratory protection program.
Leprosy
Leprosy, also known as Hansen disease, is a chronic infectious disease mainly caused by Mycobacterium leprae . This organism requires a cold host body temperature for endurance.
Clinical features
Clinical presentations of leprosy could be in one of the 2 known forms: (1) tuberculoid leprosy and (2) lepromatous leprosy.
Tuberculoid leprosy develops in patients with high immune reactions. Lepromatous leprosy is seen in patients with reduced cell-mediated immunity.
Paucibacillary leprosy
Small number of well-circumscribed, hypopigmented skin lesions will be noted. Nerve involvement resulting in anesthesia of the affected skin is observed. Oral lesions are rare in this variant.
Multibacillary leprosy
Numerous ill-defined hypopigmented macules or papules may be noted on the skin and becomes thickened with time. Skin enlargements can lead to distorted facial appearance, that is, leonine facies. Nerve involvement leads to loss of sweating and decreased sensations of light, touch, pain, and temperature. Sensory loss begins in the extremities and spreads to most of the body.
Oral manifestations
Oral soft tissue lesions initially present as yellowish to red, sessile, firm, enlarging papules that develop ulceration and necrosis ( Fig. 1 ). Deep infiltration of the soft tissue involvement leads to bone destruction.
- •
Atrophy of the anterior nasal spine
- •
Atrophy of the anterior maxillary alveolar ridge
- •
Endonasal inflammatory changes

Teeth show enamel hypoplasia and short tapering roots with internal resorption. Facial and trigeminal nerves can be involved with the infectious process. Involvement of the tongue is not uncommon with indurated areas ( Fig. 2 ). Oral erosive lesions and ulcerations can also be noted within the oral cavity ( Fig. 3 ).


Histopathological features
There are well-formed granulomas with clusters of epithelioid histiocytes, lymphocytes, and Langhans-type multinucleated giant cells. There is a lepromatous pattern with sheets of lymphocytes intermixed with vacuolated histiocytes known as lepra cells. An abundance of organisms can be demonstrated with acid-fast stains in the lepromatous variant.
Radiographic features
Facies leprosa are better visualized in lateral cephalometric radiographs because of the deficiency of the premaxillary region. Shortening of roots of the maxillary anterior teeth in a panoramic radiograph have also been reported. Gallium 67 citrate scintigraphy may be used to detect active multibacillary forms of leprosy. When gallium is used to estimate skin involvement, it is not uncommon to see a moderate to diffuse uptake of the radiopharmaceutical in the skin producing a skin outlining sign. The uptake is very important for the skin where the lepromas are commonly seen.
Dental management
Although patients with leprosy will first report to the dermatologist and rarely to the dental professional, the dental professional should be well aware of the precautions to be taken while giving any kind of treatment to these patients in a leprosy center. Appropriate treatment of dental infections will help to reduce the recurrence in leprosy reactions, as will improving the general oral hygiene of patients. Further, it is thought that oral lesions, along with nasal lesions, form an important source of bacillary dissemination in the community. Oral health status of individuals treated and healed from leprosy is poor. Better methods of oral hygiene and regular dental monitoring should be adopted in order to improve the quality of life of these patients.
Actinomycosis
Chronic granulomatous and fibrosing disease caused by Actinomyces israelii . It is chiefly characterized by the formation of abscesses that tend to drain by the formation of the sinus tract.
In 1938 Cope classified it into 3 types depending on the location:
- •
Cervicofacial
- •
Abdominal
- •
Pulmonary forms
Pathogenesis
Oral manifestations
Hyperpyrexia is noted, with the presence of regional lymphadenopathy in late stages of the disease. Swelling and indurations of the soft tissue may be noted. Later it may develop into abscesses that tend to discharge pus containing the typical sulfur granules . There are multiple sinus openings. Common sites for multiple sinus openings are mandibular or maxillary bone, which lead to actinomycotic osteomyelitis.
Histopathologic features
Histological specimen stains with hematoxylin. There is central abscess formation noted with characteristic colonies of microorganisms within it. The colonies seem to be floating in a sea of polymorphonuclear leukocytes, associated with multinucleated giant cells and macrophages at the periphery of the lesion. The eosinophilic club-shaped ends of the A israelii filaments are the basis for the term ray fungus .
Radiographic findings
Computed tomographic (CT) findings include the following:
- •
Cervico-facial actinomycosis is an enhancing soft tissue mass with a low-attenuating center associated with inflammatory change in the adjacent soft tissue. Invasion of the adjacent soft tissue, including the muscles, can occur.
- •
Actinomycotic osteomyelitis of the jaws presents as an irregularly marginated lesion with increased bone marrow attenuation, osteolysis, and involvement of the skin in all patients. Periosteal reaction and intralesional gas can also be seen in patients.
T1- and T2-weighted MRI show intermediate signal intensity associated with moderate contrast enhancement. This characteristic signal intensity may be associated with the histologic feature of abundant granulation and fibrous tissue in actinomycosis. Popcornlike dystrophic calcification can also be seen occasionally.
Extensive soft tissue inflammatory and infiltrative changes in the surrounding soft tissues extending to the skin may be useful in the differentiation of actinomycosis from osteomyelitis due to other causes.
Dental management
Initially, attempts are made to treat actinomycosis, including extensive disease, with aggressive antimicrobial therapy alone. Surgery is indicated to take a biopsy specimen, to drain abscesses, and to extirpate (wide excision) a fibrotic sinus tract. Follow-up should be adequate and meticulous to have a complete cure of the disease.
Klebsiella rhinoscleromatis Infection
It is a chronic, slowly progressive, localized infection caused by Klebsiella rhinoscleromatis . It is commonly seen in the upper respiratory tract, often originating in the nose.
Clinical features
Common sites will be lacrimal glands, orbit, skin, and paranasal sinuses. It shows features, such as exudative, proliferative, and fibrotic (cicatrical).
Exudative phase
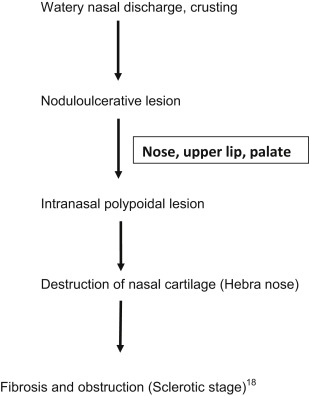
Oral manifestations
Impairment of the sensation of taste, anesthesia of the soft palate, and enlargement of the uvula and upper lip are observed.
Histopathologic features
There is a nonspecific inflammatory reaction with polymorph nuclear cells and dense plasma cell infiltration. Also noted are the Mikulicz cells: large foamy histiocytes, that is, macrophages with a size of up to 100 mm that are unable to digest phagocytosed bacteria, which persist in massively enlarged vacuoles. The sclerotic stage is characterized by granulomatous masses that result from scarring of chronically infected upper airways.
Radiographic features
CT scan of the neck shows a big air pocket in the parapharyngeal spaces. These findings are suggestive of a developing abscess. Gas-forming brain abscesses have been reported to result from escape of air into the cranium due to skull fracture or gas-forming organisms.
Anthrax
Anthrax is caused by Bacillus anthracis . In cutaneous anthrax, it clinically appears as coal-like black lesions found on the skin.
Clinical features
The spectrum of disease ranges from asymptomatic to severe, terminating in sepsis, septic shock, and death. Oropharyngeal anthrax lesions are generally localized in the oral cavity, especially on the buccal mucosa, tongue, tonsils, or posterior pharynx wall. The characteristic oral lesion is generally 2 to 3 cm in diameter and covered with a gray pseudomembrane surrounded by extensive edema. The main clinical features are sore throat, dysphagia, and painful regional lymphadenopathy in the involved side of the neck. The illness may progress rapidly, and edema around lymph nodes may result in extensive swelling of the neck and anterior chest wall. The overt infection leads to toxemia, acute respiratory distress, and alteration in mental state.
Histopathologic features
Gram-stained smear from the lesion reveals polymorphonuclear leukocytes and gram-positive bacilli, and the culture may be positive for B anthracis .
Radiographic features
- •
Disease manifests as pleural effusions, mediastinal widening, and, rarely, pneumonia. Mediastinal widening with high-attenuation mediastinal and hilar lymph nodes on CT in the absence of trauma, dissection, or bleeding diathesis is suspicious.
Brucellosis
It is a multisystem disorder with a broad spectrum of nonspecific symptoms. Brucellosis manifests as an acute febrile illness that may persist and progress to a chronically incapacitating disease with severe complications. Bone and joint involvement is the most frequent complication of brucellosis, occurring in up to 40% of cases.
Syphilis
Syphilis is caused by Treponema pallidum and is characterized by episodes of active disease interrupted by periods of latency. It can be either acquired or congenital. The acquired form is contracted as a venereal disease and if untreated manifests 3 distinctive stages throughout its course: primary, secondary, and tertiary stages.
Oral manifestations
The primary lesion is an elevated, ulcerated nodule that shows indurations and produces regional lymphadenopathy. The intraoral chancre can be appreciated. The secondary stage produces multiple, painless, grayish-white plaques overlying an ulcerated surface and are called mucous patches. Several adjacent mucous patches fuse to form a serpentine or snail-track pattern. Commonly involved sites include the tongue, gingiva, and buccal mucosa. Occasionally papillary lesions resembling viral papillomas may arise called as condylomata lata. Late congenital syphilis is diagnosed by clinical history, distinctive physical signs, and a positive serologic test. The Hutchinson triad of interstitial keratitis, Hutchinson incisors ( Figs. 4 and 5 ), and eighth cranial nerve deafness are diagnostic.

Histopathologic features
The primary lesions show ulcerated surface epithelium with several vascular channels and intense chronic inflammatory infiltrate in the underlying lamina propria. The inflammatory infiltrate is chiefly composed of lymphocytes and plasma cells and demonstrates a perivascular pattern. In the secondary stages, the epithelium demonstrates hyperplasia with significant spongiosis and exocytosis. Tertiary lesions exhibit peripheral pseudoepitheliomatous hyperplasia. The foci of granulomatous inflammation with well-circumscribed collections of histiocytes and multinucleated giant cells can be observed.
Radiographic features
- •
Syphilitic osteomyelitis causes osteolytic changes in the cortex and medullary space, usually with an aggressive pattern of bone destruction compared with other types of osteomyelitis that occur in jaws. Sequestra in syphilis are difficult to visualize radiographically because they are small and usually occur in cancellous bone. It should be stressed that the destructive lesions in early acquired syphilis are those of osteomyelitis and do not represent gummas. MRI demonstrates marrow space involvement, periosteal process, and a degree of intracranial extension more completely than CT.
- •
Proliferative periostitis has been well described in secondary syphilis and is most commonly seen in the tibiae, skull, clavicles, ribs, and sternum. Scintigraphy is a sensitive means of detection in subtle cases and can be useful in the determination of the extent of disease for guiding bone biopsy.
- •
Syphilitic gummas in CT may present as hypodense with no contrast enhancement or mass effect or as densely enhancing masses with surrounding edema. Magnetic resonance (MR) descriptions have included lesions hypointense to isointense on T1-weighted images and hyperintense on T2-weighted images, associated with homogeneous contrast enhancement.
Fungal infections
Histoplasmosis
It is a granulomatous fungal infection caused by a dimorphic fungus Histoplasma capsulatum , first described by Samuel Darling in 1905 (see Table 1 ).
Clinical features
It is acquired by the inhalation of dust containing the spores of fungus or contamination occurring from excreta of birds, such as pigeons, starlings, and black birds. It is clinically classified into the following:
- •
Acute primary pulmonary histoplasmosis
- •
Chronic pulmonary histoplasmosis
- •
Disseminated histoplasmosis
It is characterized by chronic low-grade fever, productive cough, splenomegaly, hepatomegaly, and lymphadenopathy. The infection may be mild and manifests only as local lesions, such as subcutaneous nodules or supportive arthritis. Oral lesions appear as nodular, ulcerative, or vegetative lesions on the buccal mucosa, gingiva, tongue, palate, or lips. Ulcerated areas are covered by a gray membrane that is indurated with raised and rolled-out borders resembling carcinoma. It is solitary and very painful.
Histopathologic features
The classic feature of histoplasmosis is granuloma formation, a collection of macrophages organized into granulomas. Granulomatous inflammation is associated with multinucleated giant cells. Special stains, such as periodic acid-Schiff and Grocott–Gomori methenamine silver methods, can be used. They demonstrate characteristic 2- to 4-μm oval, narrow-based budding yeasts of H capsulatum . Yeasts are found within the macrophages and can also be seen free in the tissues.
Radiographic features
In chronic pulmonary histoplasmosis, chest radiographs often reveal emphysematous lungs with apical bullae surrounded by segmental airspace disease. Progressive thickening of cavity walls and retraction of adjacent lung tissue occur over time, but lymphadenopathy is typically absent. In disseminated histoplasmosis, chest radiographs may be normal but usually display small, diffuse, nodular opacities.
Treatment of histoplasmosis depends on the severity of the clinical syndrome. Mild cases may require only symptomatic measures, but antifungal therapy is indicated in all cases of chronic or disseminated disease and in severe or prolonged acute pulmonary infection.
Blastomycosis
It is also called as Gilchrist disease. It is caused by Blastomyces dermatitidis , which is a dimorphic fungus. It is endemic in South, South Central, and the Great Lakes regions of the United States as well as parts of Canada.
Clinical features
The source of infection in humans is unknown. Most commonly affected individuals are those who work in the outdoors for longer time periods. It occurs in the middle-aged population, and men are more commonly affected than women. It manifests on the skin as small red papules that gradually increase in size and form tiny miliary abscess or pustules that tend to ulcerate and discharge pus. It presents as crateriform lesions with induration and elevated borders. It is associated with fever, sudden weight loss, and productive cough. Oral manifestations are either primary or secondary to lesions present on the body. It is characterized by tiny ulcers. These lesions may bear resemblance to epidermoid carcinoma.
Histopathologic features
It is characterized by acute inflammatory cell infiltrate followed by histiocytic response and granuloma formation. Inflamed connective tissue shows multinucleated giant cells, and microabscesses are found frequently. The granulomas are noted with central necrotic neutrophils surrounded by epithelioid histiocytes. The yeasts are present within the purulent centers of the granulomas and within the histiocytes measuring between 5 μm and 15 μm in diameter. They are round and have a double refractive capsule. Nonulcerated lesions present pseudoepitheliomatous hyperplasia.
Radiological features
There are reported cases of radiolucent bone lesions in the jaws in blastomycosis. Chest radiographs show concomitant pulmonary involvement in all cases. The major radiologic features of pulmonary involvement fall into the following categories: airspace consolidation, masses, intermediate sized nodules, interstitial disease, miliary disease, and cavitary lesions. Unlike histoplasmosis, blastomycotic infections rarely have parenchymal or lymph node calcifications.
Treatment
Ketoconazole, fluconazole, or itraconazole is used for the management of mild to moderate disease and amphotericin B for severe disease.
Phycomycosis
It is also called mucormycosis and zygomycosis. It was first described by Paultauf in 1885. It is caused by numerous Phycomycetes organisms of the Eumycetes class, such as Rhizopus , Mucor , Absidia , and, rarely, Saksenaea and Cunninghamella .
Clinical features
- •
There are 5 forms of the disease:
- ○
Rhinocerebral
- ○
Pulmonary
- ○
Gastrointestinal (GI) tract
- ○
Cutaneous
- ○
Disseminated
- ○
- •
It occurs in 2 main forms:
- ○
Superficial
- ○
Visceral
- ○
- •
It is an opportunistic infection manifesting in those with malignant lymphomas, patients having renal failure, organ transplant, AIDS, and cirrhosis. It is more common in patients with uncontrolled diabetes mellitus who are ketoacidotic. Ketoacidosis inhibits the binding of iron to transferrin and raises the levels of iron, which in turn enhances the growth of these fungi.