There are both odontogenic and nonodontogenic benign lesions in the maxilla and mandible. These lesions may have similar imaging features, and the key radiographic features are presented to help the clinician narrow the differential diagnosis and plan patient treatment. Both intraoral and panoramic radiographs and advanced imaging features are useful in assessing the benign lesions of the jaws. The location, margins, internal contents, and effects of the lesions on adjacent structures are important features in diagnosing the lesions.
Key points
- •
Benign lesions of the jaws can be either odontogenic or nonodontogenic and have a variety of cystic and solid appearances.
- •
The radiographic features of plain films in conjunction with advanced imaging can help the clinician in the differential diagnosis, presurgical planning, and management of the lesion.
- •
Both intraoral and panoramic radiographs and advanced imaging features are useful in assessing the benign lesions of the jaws.
- •
The location, margins, internal contents, and effects of the lesions on adjacent structures are important features in diagnosing the lesions.
Introduction
Benign lesions can develop from both odontogenic and nonodontogenic tissues in the maxilla and mandible. Odontogenic lesions can arise from tooth-forming epithelium, mesenchymal tissue, or both. In the mandible, odontogenic lesions originate superior to the mandibular canal. Neural and vascular lesions often originate within the mandibular canal, whereas lesions with epicenter inferior to the inferior alveolar canal are usually nonodontogenic in origin.
Benign odontogenic lesions are characterized by well-defined margins with regular borders causing expansion, displacement of adjacent structures, and directional root resorption. Intraoral and panoramic radiographs can show the superior-inferior and antero-posterior extent of the lesion. However, additional imaging, including cone beam computed tomography (CBCT), multidetector-row CT (MDCT), and MRI, is needed to effectively diagnose the extent of the lesion in all 3 planes. CBCT and MDCT imaging are highly useful for showing the extent of the lesion, expansion, and any ossifications/calcifications. MDCT has a better soft tissue resolution compared with CBCT. MRI is effective in differentiating cysts and tumors, evaluating the infiltration in the jawbone and surrounding soft tissue and detecting bone marrow changes of the jaw. Combining radiography with advanced imaging techniques, including CT and MRI, can improve the accuracy of diagnosing the benign lesions in the jaws.
Introduction
Benign lesions can develop from both odontogenic and nonodontogenic tissues in the maxilla and mandible. Odontogenic lesions can arise from tooth-forming epithelium, mesenchymal tissue, or both. In the mandible, odontogenic lesions originate superior to the mandibular canal. Neural and vascular lesions often originate within the mandibular canal, whereas lesions with epicenter inferior to the inferior alveolar canal are usually nonodontogenic in origin.
Benign odontogenic lesions are characterized by well-defined margins with regular borders causing expansion, displacement of adjacent structures, and directional root resorption. Intraoral and panoramic radiographs can show the superior-inferior and antero-posterior extent of the lesion. However, additional imaging, including cone beam computed tomography (CBCT), multidetector-row CT (MDCT), and MRI, is needed to effectively diagnose the extent of the lesion in all 3 planes. CBCT and MDCT imaging are highly useful for showing the extent of the lesion, expansion, and any ossifications/calcifications. MDCT has a better soft tissue resolution compared with CBCT. MRI is effective in differentiating cysts and tumors, evaluating the infiltration in the jawbone and surrounding soft tissue and detecting bone marrow changes of the jaw. Combining radiography with advanced imaging techniques, including CT and MRI, can improve the accuracy of diagnosing the benign lesions in the jaws.
Odontogenic cysts
A cyst contains fluid and is lined by an epithelium and is surrounded by a connective tissue. The fluid in the cyst is secreted by the lining cells or is derived from surrounding tissues. The fluid in the cyst exerts equal pressure in all directions so the cysts appear round or oval on radiographs. Cysts are broadly classified as odontogenic cysts and nonodontogenic cysts.
Odontogenic cysts are 2.25 times more frequently seen than odontogenic tumors. Radiographically, they appear as lytic round or hydraulic-shaped lesions, with well-defined corticated margins ( Table 1 ). Long-standing cysts may have dystrophic calcifications within them.
| Cysts | Radiographic Findings | CBCT/MDCT Findings | MRI Findings |
|---|---|---|---|
| Radicular cyst | Round radiolucent lesions with sclerotic borders at the apices of nonvital teeth. | Better demonstrate the extent of the cyst, expansion in all dimensions. | High T2 (high fluid content) and variable T1 signal intensity. Contrast-enhanced MR images show rim enhancement consistent with inflammation. |
| Residual cyst | Well-defined radiolucency with sclerotic borders apical to an extraction site. | Better demonstrate the extent of the cyst, expansion in bucco-lingual direction. | High T2 (high fluid content) and variable T1 signal intensity. Contrast-enhanced MR images show rim enhancement consistent with inflammation. |
| Dentigerous cyst | Well-defined pericoronal radiolucency with corticated borders causing substantial displacement. Expansion and root resorption may be present. Cortical boundaries are usually preserved. |
Better demonstrate the extent of the cyst, expansion in bucco-lingual direction. | Low-to-intermediate signal T1 and high signal on T2-weighted mages with signal void representing the crown. Can help recognize mural ameloblastomas forming within the cyst lining. |
| Nasopalatine cysts | Well-defined radiolucency in the anterior maxillary region in midline. Can displace roots of adjacent teeth. The lesion is usually palatal to the teeth. |
Better demonstrate the extent of the cyst, expansion in all 3 dimensions. | Water density/signal, may have increased density or T1 signal due to high protein concentration. |
| Simple bone cyst | Usually seen in the posterior mandible as a radiolucency scalloping between the roots of the teeth. Well-defined superiorly, but the inferior borders may not be well defined. |
Better demonstrate the extent of the cyst, expansion in all 3 dimensions. | Variable signal depending on protein concentration within the cyst. |
Radicular (Periapical) Cysts
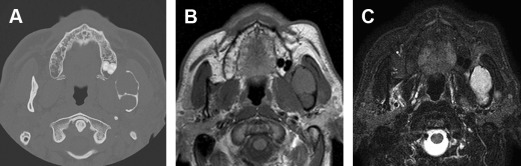
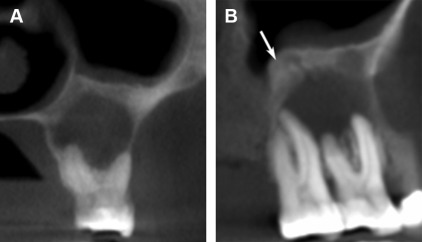
Radicular (periapical) cysts are the most common odontogenic cysts found at the apices of a nonvital tooth resulting from inflammation of the periapical tissues secondary to caries or trauma. These lesions appear radiolucent with well-defined and corticated margins. Large periapical cyst may cause root resorption, displacement of adjacent structures, and expansion ( Fig. 1 ). CBCT images may be superior compared with periapical radiographs in detecting a periapical lesion. There are 25% to 60% more periapical lesions detected by CBCT compared with intraoral periapical radiographs. A radicular cyst remaining after the extraction of the tooth is a residual cyst.
Dentigerous Cysts
Dentigerous cysts appear as a pericoronal radiolucency associated with an unerupted or impacted tooth ( Fig. 2 ). These cysts are caused by expansion of dental follicles resulting from accumulation of fluid between the tooth crown and epithelial components often affecting the maxillary canine and mandibular third molar. Dentigerous cysts are known to cause considerable displacement of the teeth with which it is associated. Maxillary teeth may be pushed into the antrum, and mandibular third molars may be displaced into the ramus or inferior border of the mandible.
Lateral Periodontal Cysts
Lateral periodontal cysts arise from the epithelial rests lateral to the tooth root. It appears as a well-defined, lytic lesion with a corticated boundary. The botryoid variety may appear multilocular.
Nonodontogenic cysts
Nasopalatine Duct/Incisive Canal Cysts
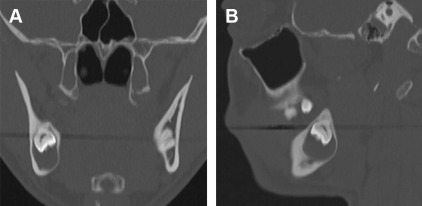
Nasopalatine duct/incisive canal cysts are the most common nonodontogenic cysts in the maxilla. These cysts are thought to arise from proliferation of epithelial remnants of the embryologic nasopalatine duct. Most of the cysts are found in the incisive foramen or the canal in the anterior maxilla. The cysts may appear as a periapical radiolucency in association with the maxillary anterior teeth, but the associated teeth are vital ( Fig. 3 ). On CBCT scan, the average diameter of these cysts was reported to be around 14 mm with a tendency to be larger in men.
Simple Bone Cyst
Simple bone cyst is not a true cyst but a cavity within the jaws lined by connective tissue. Mainly seen in the mandibular posterior region, usually in the second decade of life, these lesions appear to scallop between the roots of the teeth giving it a multilocular appearance ( Fig. 4 ). Theses cysts are usually asymptomatic and rarely cause expansion.

Benign odontogenic tumors
Benign odontogenic tumors grow slowly and appear well defined with smooth and sometimes corticated borders. Unlike the cysts, these lesions may be radiolucent, mixed density, or radiopaque depending on the tissue of origin. They do exert pressure on surrounding tissues and can cause displacement, expansion, and root resorption ( Table 2 ).
| Benign Odontogenic Tumor | Radiographic Findings | CBCT/MDCT Findings | MRI Findings |
|---|---|---|---|
| KOT | Unilocular/multilocular lesions with scalloped margins. May appear as a pericoronal radiolucency. Expansion more prominent in the ramus. Root resorption and displacement to a lesser extent. If multiple, consider the possibility of basal cell nevus syndrome. |
Better demonstrate the extent of the cyst, presence of daughter cyst especially with MDCT. | Higher signal on T1-weighted and lower signal on T2-weighted images compared with ameloblastoma Slight contrast enhancement Malignant transformation into squamous cell carcinoma may occur |
| Ameloblastoma | Well-defined unilocular/multilocular radiolucency. May appear as a pericoronal radiolucency. Extensive root resorption. |
Better demonstrate the extent of the lesion and osseous destruction. Better able to delineate the cortical destruction. |
Heterogeneous intermediate signal on T1-weighted images with heterogeneous enhancement after intravenous contrast administration. |
| Calcifying epithelial odontogenic tumor | Well-defined radiolucency with calcifications. May appear as pericoronal radiolucency with calcifications close to the crown. |
Better demonstrate the extent of the lesion, expansion in bucco-lingual direction, and calcifications. | Predominantly hypointense on T1-weighted and mixed hyperintensity on T2-weighted images with heterogeneous enhancement. |
| Odontoma | Well-defined mixed density (teethlike) with a thin radiolucent capsule. Compound odontoma have toothlike structures, whereas complex odontoma appears as an irregular mass of calcified tissue. May interfere with the eruption if associated with a tooth. |
Can demonstrate the extent of the lesion, expansion in all 3 dimensions. | Signal void, possibly with rim of fluid signal. |
| Ameloblastic Fibro-Odontoma | Well-defined radiolucent/mixed density lesion occlusal to a developing teeth. | Can demonstrate the extent of the lesion, expansion in all 3 dimensions. Can better depict areas of calcifications. |
Signal void, possibly with rim of fluid signal. |
| Adenomatoid Odontogenic Tumor | Well-defined radiolucent/mixed density lesion usually in the anterior maxillary region. If associated with an impacted tooth, the lesions are found more apically on the root than are dentigerous cysts. |
Better demonstrate the extent of the lesion, expansion in all 3 dimensions. Better depict areas of calcifications |
Intermediate to low signal on T1 and high signal on T2-weighted images. |
| Odontogenic myxoma | Well-defined to poorly defined, unilocular or multilocular radiolucent lesion. Scalloped margins with fine straight septa may be noted. Expansion, root resorption, and tooth displacement also seen. |
Better demonstrate the extent of the lesion, expansion. Better reveal the extension of the lesion into adjacent soft tissue. |
Mixed signal on T1 and heterogeneous hyperintense signal on T2-weighted images with varying patterns of enhancement, often with lobulated appearance. |
| Cementoblastoma | Well-defined mixed density lesion at the apices of mandibular posterior teeth. Radiolucent rim surrounding the lesion. Can cause root resorption and expansion. |
Better demonstrate the extent of the lesion, expansion. | Signal void. |
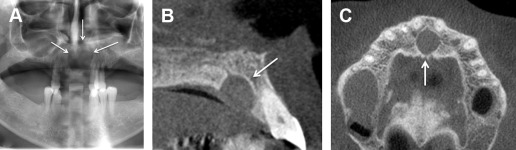
Keratocystic Odontogenic Tumors
Keratocystic odontogenic tumors (KOT) are most commonly located in the posterior mandible, with a male predilection, often in association with an impacted tooth. KOTs may have scalloped borders with mainly unilocular interior, and are sometimes multilocular. In the body of the mandible, KOTs are noted to grow with minimal expansion, and significant expansion may occur in the ramus. KOTs can resorb roots of teeth and displace adjacent structures but at a lesser frequency than dentigerous cysts ( Fig. 5 ). There may be daughter cysts that extend into the surrounding bone and, thus, there is a high recurrence rate—as much as 28%. Multiple KOTS in a young patient should raise the possibility of basal cell nevus syndrome ( Fig. 6 ). Gorlin & Goltz described the syndrome with multiple basal cell carcinoma, keratocystic odontogenic tumors, and bifid ribs. Additionally, calcification of the falx cerebri, palmar and plantar epidermal pits, spine and rib anomalies, relative macrocephaly, frontal bossing, medulloblastomas, cleft lip or palate, and developmental malformations may also be present. Multiple KOTs may be the first manifestation of this syndrome, occurring as early as the first decade of life.