Introduction
In this study, we aimed to investigate the dental and skeletal changes associated with long-term use of the Silensor appliance (Erkodent, Cologne, Germany) in patients with obstructive sleep apnea and hypopnea syndrome.
Methods
The sample included 42 patients with mild-to-severe obstructive sleep apnea and hypopnea syndrome (mean apnea-hypopnea index, 27; range, 5-74) who had been treated with the Silensor appliance for an average of 4 years (range, 1-11 years). A questionnaire was used to assess of the side effects subjectively; the cephalometric analysis was conducted to identify the dental and skeletal changes of different treatment times objectively.
Results
The Silensor appliance was associated with few subjective side effects. Most subjective side effects decreased after long-term use of the Silensor appliance. Significant changes after long-term use of the Silensor appliance were observed in incisor angulation, overbite, overjet, mandibular plane angle, anterior lower facial height, and anterior facial height. Overbite and skeletal changes at treatment times between 1 year and 3 years were a decrease in overbite and increases in the mandibular plane angle, anterior lower facial height, and anterior facial height. Overjet and other dental changes at treatment times longer than 3 years were a decrease in overjet, retroclination of the maxillary incisors, and proclination of the mandibular incisors.
Conclusions
The Silensor appliance was well tolerated and preferred by most subjects. Common but mild dental and skeletal changes resulted from using the appliance over a long period of time. The changes after 1 to 3 years of use were skeletal changes predominantly. Both dental and skeletal changes were observed simultaneously at treatment times longer than 3 years.
Highlights
- •
The Silensor appliance was well tolerated and preferred by most subjects.
- •
The side effects were relieved with an extension of treatment time.
- •
The Silensor produced maxillary incisor retroclination and mandibular incisor proclination.
- •
Skeletal changes tended to occur in the short term after treatment.
- •
Dental changes tended to occur with an extension of treatment time.
Obstructive sleep apnea and hypopnea syndrome (OSAHS) is a sleep-related breathing disorder characterized by repeated narrowing or collapse of the upper airway during sleep, resulting in hypoxemia, arousal, and fragmentation of sleep. Since the first description of the disease, many treatment methods have been attempted, including weight loss, medication, surgery, and continuous positive airway pressure (CPAP). Mandibular advancement devices (MADs) have also been reported to be an effective treatment option for patients with OSAHS. Therapy with MADs is increasingly popular not only because of its good efficacy, but also because of its simplicity, high acceptance, noninvasiveness, and low cost.
According to the American Academy of Sleep Medicine, MADs are indicated in patients with primary snoring and upper airway resistance syndrome, patients with mild-to-moderate OSAHS who prefer MADs to CPAP, and those with severe OSAHS who refuse CPAP. Many MADs that vary in design are in use, but it is now recognized that the anterior repositioning of the mandible is an essential mechanism of the MAD by which the oropharyngeal space is increased. The Silensor appliance (Erkodent, Cologne, Germany) is a type of custom-made semirigid MAD with a satisfying efficacy and a low frequency of subjective side effects. Furthermore, a recent study suggested that the Silensor appliance is suitable for the first phase of oral appliance treatment for OSAHS.
Dental and skeletal changes associated with long-term use of MADs have been studied with cephalometric analysis. Most authors evaluated the side effects induced by MAD use for an average of 2 to 3 years. In addition, in most studies, only patients with mild-to-moderate OSAHS or snorers were included. Among various authors, Almeida et al reported changes after at least 5 years of oral appliance use. However, the oral appliances in that study were rigid MADs and held the mandible in a fixed forward and slight downward position. MAD design is thought to be one factor that could affect the side effects from use of the appliance. Compared with rigid MADs, the Silensor appliance has an adjustable advancement of the mandible with mouth opening. Any further opening of the mouth increases the anterior displacement of the mandible. Therefore, a better understanding of the possible side effects after long-term treatment with semirigid MADs is meaningful.
The aim of this study was to investigate the possible dental and skeletal changes associated with long-term use (4 years on average) of the Silensor appliance in patients with mild-to-severe OSAHS.
Material and methods
In this study, 56 subjects who fulfilled the following inclusion criteria were initially selected: (1) diagnosed with OSAHS based on polysomnography examination and suitable for Silensor appliance treatment (with mandibular retrognathia, a downward positioned hyoid bone, or a narrow oropharyngeal airway); (2) no mental or psychological illness; (3) enough teeth to retain the appliance without periodontitis; (4) no active temporomandibular dysfunction; (5) answered the pretreatment questionnaire and had cephalometric radiography; and (6) signed written informed consent. The follow-up polysomnography was completed after 4 weeks for the final adjustment of the Silensor appliance to evaluate the efficiency. Then 4 subjects who did not meet the success criteria based on the polysomnography examination (a decrease in the apnea-hypopnea index to <5 for mild OSAHS patients and a reduction in the apnea-hypopnea index by 50% for moderate and severe OSAHS patients ) were excluded. During this study, we recalled them for regular clinical reviews at 1-year intervals. At the end of this study, we recalled the subjects for questionnaires and follow-up cephalometric radiographs. The exclusion criteria included (1) not wearing the Silensor appliance for more than 5 hours per night and 5 days per week for at least 1 year (5 subjects), (2) had CPAP therapy or surgical treatment during the study (2 subjects), (3) had tooth extractions or periodontal surgery during the study (1 subject), or (4) lost to follow-up (2 subjects). Overall, 42 subjects were included in this study. Their clinical characteristics are shown in Table I .
| Parameter | Value |
|---|---|
| Sex | 31 men (74%), 11 women (26%) |
| Age (y) | 47 ± 10 (range, 26-70) |
| Apnea-hypopnea index | 27 ± 19 (range, 5-74) |
| Treatment time (y) | 4 ± 3 (range, 1-11) |
| <3 (22 subjects) | |
| ≥3 (20 subjects) |
All patients received treatment at the Department of Dentistry, Xuanwu Hospital, Capital Medical University, and the Department of Orthodontics, Peking University School and Hospital of Stomatology, in China. This study was approved by the institutional review board of Xuanwu Hospital, Capital Medical University.
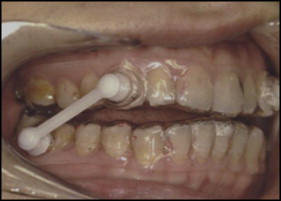
The Silensor appliance is a type of custom-made semirigid MAD, composed of soft methyl methacrylate and 2 separate splints connected by bars with 4 different lengths. Most teeth in both arches are covered by the splints, except for the third molars. The design of the Silensor appliance is shown in Figure 1 . The Silensor appliance induced mandibular advancements of 65% to 75% of maximum protrusion and 4.5 to 5 mm of vertical displacements. The adjustment was performed during the first 2 to 4 weeks of treatment. Then a questionnaire was completed as the baseline after 4 weeks for the final adjustment of the Silensor appliance. The questionnaire included several yes or no questions that addressed the side effects. At the end of this study, we recalled the patients with long-term use of Silensor appliance, and the same questionnaire was repeated to evaluate the long-term subjective side effects.
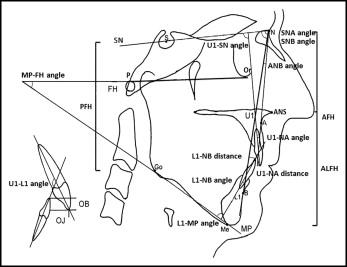
Standardized lateral cephalometric radiographs were routinely obtained at pretreatment as the baseline. At the end of this study, we recalled the patients not only for the questionnaire, but also for the follow-up lateral cephalometric radiograph (without the Silensor appliance). The baseline and the follow-up lateral cephalometric radiographs were measured and compared to evaluate dental and skeletal changes in the patients who received treatment with the Silensor appliance. The patients were asked to bite in intercuspation, breathe slowly, and not swallow during the radiograph procedure. The cephalometric analysis was based on the methods of the Steiner and Wylie, using the professional cephalometric analysis software Dental Studio NX (version 6.0; Nemotec, La Plaine de Saint-Denis, France). The landmarks, reference lines, angles, and distances used in the cephalometric analysis are shown in Figure 2 .
To improve accuracy, all distances and angles were measured twice, on 2 separate occasions 2 weeks apart, by a blinded operator (X.W.). The method error was assessed using Dahlberg’s formula : ME 2 = ∑d 2 /2n, where ∑d 2 is the sum of the squared differences between pairs of recordings, and n is the number of double measurements. The method error in the linear measurements fell within the range of 0.18 to 0.40 mm, and the angular measurements fell within 0.23° to 0.41°. The mean values were used for statistical analysis.
Statistical analysis
The data are presented as the mean values and standard deviations. Dental and skeletal characteristics between the baseline and follow-up were compared using the Student paired t test (version 11.5) with a significance level of 0.05. Further analysis of the data was then undertaken by comparing each treatment time (<3 years and ≥3 years) between the baseline and follow-up.
Results
All 42 patients completed the questionnaire and underwent a clinical examination. The Silensor appliance was associated with a low rate of side effects. Most subjective side effects were decreased after long-term use of the Silensor appliance. Only 1 patient reported an occlusal change at the follow-up, but positive overjet and overbite and multiple occlusal contacts were maintained. The questionnaire data at baseline and at follow-up are shown in Table II .
| Subjective side effects ∗ | Baseline | Follow-up |
|---|---|---|
| Excessive salivation | 15 (36%) | 9 (21%) |
| Dry mouth | 7 (17%) | 4 (10%) |
| Dental discomfort | 18 (43%) | 7 (17%) |
| Occlusal change | 0 (0%) | 1 (2%) |
| Loosening of tooth | 0 (0%) | 0 (0%) |
| Tongue discomfort | 0 (0%) | 0 (0%) |
| Gingival discomfort | 0 (0%) | 0 (0%) |
| Maxillofacial discomfort | 15 (36%) | 2 (5%) |
∗ Subjects were asked to mark “yes” when the side effect occurred subjectively.
After 4 years on average of treatment with the Silensor appliance, the maxillary incisors showed significant retroclinations, with decreases in the U1-SN angle, U1-NA angle, and U1-NA distance. There were significant proclinations of the mandibular incisors, with increases in the L1-MP and L1-NB angles. Furthermore, the relationship between the maxillary and mandibular incisors significantly changed, with decreases in overbite and overjet. Dental changes after long-term use of the Silensor appliance are shown in Table III .
| Baseline | Follow-up without Silensor appliance | Difference | P value | |
|---|---|---|---|---|
| U1-SN angle (°) | 100.51 ± 6.37 | 99.02 ± 6.86 | −1.49 ± 1.55 | <0.001 ∗ |
| U1-NA angle (°) | 20.16 ± 5.69 | 18.75 ± 6.28 | −1.41 ± 1.85 | <0.001 ∗ |
| U1-NA distance (mm) | 4.75 ± 2.64 | 4.07 ± 2.68 | −0.68 ± 0.87 | <0.001 ∗ |
| L1-MP angle (°) | 99.16 ± 7.26 | 100.10 ± 7.24 | 0.94 ± 1.31 | <0.001 ∗ |
| L1-NB angle (°) | 30.78 ± 6.24 | 31.80 ± 6.29 | 1.02 ± 1.09 | <0.001 ∗ |
| L1-NB distance (mm) | 8.84 ± 2.96 | 8.91 ± 2.93 | 0.07 ± 0.70 | 0.495 |
| U1-L1 angle (°) | 122.37 ± 9.38 | 122.57 ± 9.20 | 0.20 ± 0.81 | 0.115 |
| Overbite (mm) | 3.28 ± 1.40 | 2.27 ± 1.46 | −1.01 ± 0.81 | <0.001 ∗ |
| Overjet (mm) | 4.32 ± 1.73 | 3.29 ± 1.75 | −1.03 ± 0.90 | <0.001 ∗ |
No significant changes were observed in the SNA and SNB angles. Regarding the intermaxillary relationships, the ANB angle did not change significantly. A downward rotation of the mandible was observed, with an increase in the MP-FH angle. There were increases in anterior lower facial height and anterior facial height. No significant changes were observed in posterior facial heights. Skeletal changes after long-term use of the Silensor appliance are shown in Table IV .
| Baseline | Follow-up without Silensor appliance | Difference | P value | |
|---|---|---|---|---|
| SNA angle (°) | 80.80 ± 4.10 | 80.64 ± 3.84 | −0.16 ± 1.32 | 0.426 |
| SNB angle (°) | 75.53 ± 3.93 | 75.69 ± 3.93 | 0.16 ± 0.82 | 0.217 |
| ANB angle (°) | 5.27 ± 1.94 | 4.94 ± 2.13 | −0.32 ± 1.90 | 0.277 |
| MP-FH angle (°) | 27.20 ± 5.86 | 28.68 ± 6.10 | 1.48 ± 1.77 | <0.001 ∗ |
| ALFH (mm) | 72.14 ± 6.20 | 73.66 ± 6.23 | 1.52 ± 1.02 | <0.001 ∗ |
| AFH (mm) | 127.44 ± 8.56 | 129.01 ± 8.72 | 1.56 ± 1.20 | <0.001 ∗ |
| PFH (mm) | 86.17 ± 9.08 | 86.17 ± 8.74 | 0.00 ± 1.25 | 0.990 |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


