Introduction
In this systematic review, we assessed the literature to determine which evidence level supports the association of orthodontic force system and root resorption.
Methods
PubMed, Cochrane, and Embase databases were searched with no restrictions on year, publication status, or language. Selection criteria included human studies conducted with fixed orthodontic appliances or aligners, with at least 10 patients and the force system well described.
Results
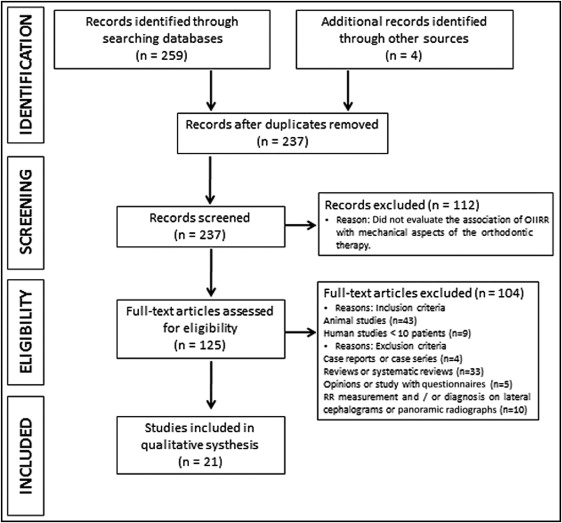
A total of 259 articles were retrieved in the initial search. After the review process, 21 full-text articles met the inclusion criteria. Sample sizes ranged from 10 to 73 patients. Most articles were classified as having high evidence levels and low risks of bias.
Conclusions
Although a meta-analysis was not performed, from the available literature, it seems that positive correlations exist between increased force levels and increased root resorption, as well as between increased treatment time and increased root resorption. Moreover, a pause in tooth movement seems to be beneficial in reducing root resorption because it allows the resorbed cementum to heal. The absence of a control group, selection criteria of patients, and adequate examinations before and after treatment are the most common methodology flaws.
A common goal that permeates the practice of orthodontics has been the determination of the “optimal” force magnitude, which results in the highest rate of tooth movement with minimal iatrogenic side effects. Still, orthodontically induced inflammatory root resorption (OIIRR) is an undesirable risk of orthodontic treatment. OIIRR is a biomechanical phenomenon: an association between OIIRR and biologic effects has been shown. It is known that the biologic factors are intrinsic to the patient and, until now, have not been able to be modified. Thus, it is essential to identify how the biomechanical orthodontic treatment factors influence OIIRR to minimize the risks and the severity of this phenomenon.
Orthodontic tooth movement involves a series of biologic reactions after force application, which makes teeth vulnerable to root resorption. Already in the 1930s, Schwarz proposed that the “optimal” force for tooth movement, characterized by maximal cellular response with maintenance of the vitality of the tissues, should be within the levels of capillary pressure. If the capillary blood pressure is exceeded, this may cause collapse of the capillaries and dysfunction of the blood supply. This phenomenon may result in a degradation of the tooth-protecting outer layers of the precementum and its formative layer of cementoblasts; this activates the resorptive activity of the clastic cells. This process leaves the mineralized tooth tissue denuded, triggering inflammatory events, similar to bone resorption, but on the root surface.
Although the severity of OIIRR is mostly clinically insignificant, the literature shows that 1% to 5% of orthodontically treated teeth have severe OIIRR, which is defined as resorption exceeding 4 mm or a third of the original root length. A significant reduction in the root length can cause an unfavorable crown-root ratio of the affected teeth. This has great clinical significance, especially when it is coincident with alveolar bone loss or combined with orthodontic retreatment. Apical root loss of 3 mm is equivalent to 1 mm of crestal bone loss, which means that periodontal bone loss will reach a critical stage more rapidly if it is accompanied by OIIRR. Regarding orthodontic retreatments, when force is again applied to a tooth with an already traumatized external surface, the onset of resorption will probably be much more rapid and extensive than that occurring during the primary activation.
Several reviews, systematic reviews, and a meta-analysis have been performed over the years, aiming to elucidate possible treatment-related etiologic factors to guide clinical decisions that will minimize the risks of severe root resorption. Most authors agree that this biomechanical phenomenon depends on both time and force. The direction of tooth movement and the loading regimen (continuous vs intermittent forces) also appear to have considerable impact in its occurrence. Yet, until today, no investigators have conducted a systematic review to evaluate the state of the published scientific research on OIIRR, considering the mechanical aspects, the methodologic quality, and the risk of bias. According to the preferred reporting items for systematic reviews and meta-analyses (PRISMA) 2009 checklist, Table I better outlines the questions that will be addressed with reference to participants, interventions, comparisons, outcomes, and study designs (PICOS) in this study.
| Component | Description |
|---|---|
| Population | Clinical studies that involved patients having orthodontic treatment |
| Intervention | Orthodontic therapy with conventional fixed appliances or aligners |
| Comparison | Mechanical variables of the orthodontic treatment (continuous vs intermittent forces, light vs heavy forces, influence of tooth movement direction, duration of treatment, and types of orthodontic appliances) |
| Outcome | OIIRR |
| Study design | Randomized and nonrandomized controlled trials, and cohort studies |
The aims of this systematic review were to assess the scientific literature that has examined root resorption as an outcome of orthodontic treatment and to determine which level of evidence is available to support the association of root resorption with different orthodontic force systems.
Material and methods
This systematic review was performed according to the Cochrane Oral Health Group’s Handbook for Systematic Reviews of Interventions ( http://ohg.cochrane.org ) and was registered with the number CRD42014008912 in the PROSPERO database ( http://www.crd.york.ac.uk/PROSPERO ). A computerized systematic search was performed in 3 electronic databases: PubMed, Cochrane, and Embase. For the PubMed and Cochrane databases, we selected the following search sequence of medical subject headings (MeSH) terms: [“orthodontics” AND “root resorption” AND (“biomechanics” or “dental stress analysis”)]. For the Embase database, we selected the following search sequence of Emtree terms: [“orthodontics” AND “tooth root” AND (“biomechanics” OR “dental stress analysis”)].
Hand searches were undertaken to find additional relevant published material that might have been missed in the electronic searches. No restrictions were placed on year, publication status, or language of the articles. The search was performed on December 17, 2013.
In the first step of the screening process, titles and abstracts were used to identify full articles concerning the association of root resorption with the mechanical aspects of orthodontic treatment with fixed appliances and aligners. The ones that evaluated the risk of root resorption based on genetic factors were not considered relevant for this systematic review. In the second step of the screening process, these full articles were subjected to inclusion and exclusion criteria. The inclusion criteria required the studies to be performed on humans, evaluating root resorption as an outcome of orthodontic treatment, with at least 10 subjects. The exclusion criteria were case reports, case series, reviews, systematic reviews, opinions, studies with questionnaires, and studies where the diagnosis or measurement of OIIRR was performed only on lateral cephalograms or panoramic radiographs. The lowest level of evidence accepted was cohort studies.
All studies identified by applying the inclusion and exclusion criteria underwent assessment for validity and data extraction by 2 reviewers (M.G.R. and P.M.C.), who independently examined the studies. The studies that were appropriate to be included were randomized and nonrandomized controlled trials, and cohort studies fulfilling the criteria concerning populations, intervention characteristics, comparison groups, and outcomes as stated in Table I . The reviewers extracted data independently, using specifically designed data-extraction forms. For each included study, qualitative and quantitative information was extracted, including year of publication, experimental and control treatments, numbers and ages of patients, treatment and follow-up durations, method of outcome assessment, authors’ conclusions, and all information needed for the methodologic quality evaluation. Any disagreement was discussed to reach a common final decision. If further clarifications were deemed necessary, the authors of the articles were contacted by e-mail.
The available literature already includes some scoring systems, which were used as the starting point to develop our methodologic scoring system. Consequently, the remaining articles were scored by the 2 reviewers to analyze study design and conduct, methodologic soundness, and data analysis to answer the research question. This system resulted in the 13 criteria shown in Table II .
| Criteria assessed | Score |
|---|---|
| I. Study design (maximum score, 10 points) | |
| A. Time | Retrospective, 0 point; prospective, 2 points |
| B. Randomization | If stated, 1 point |
| C. Control group | If present, 1 point |
| D. Sample size | Number of evaluated teeth per experimental group: <5, 1 point; 5 to ≤10, 2 points; >10 to ≤20, 3 points; >20, 4 points |
| E. Selection criteria | If clearly described, 1 point |
| F. Objective | If clearly formulated, 1 point |
| II. Methodologic soundness (maximum score, 7 points) | |
| A. Appliance type | If clearly described, 1 point |
| B. Force magnitude | If stated, 1 point; if controlled by a force measurement device, 2 points |
| C. Radiographic examination before treatment | Periapical radiograph or cone-beam computed tomography, 1 point; other method, 0 point |
| D. Measurement method of root resorption | Periapical radiograph or histological analysis, 1 point; SEM, TEM, CLSM, or μCT, 2 points (if 2 methods were combined, the points were summed) |
| III. Data analysis (maximum score, 4 points) | |
| A. Statistical analysis | Appropriate for data, 1 point |
| B. Error of the method | If stated, 1 point |
| C. Data presentation | If P value stated, 1 point |
| If any variability measures (standard deviation, confidence interval, or range) stated, 1 point | |
Concerning study design, time, randomization assignment, control group, sample size, description of the selection criteria for patients, and formulation of the objective of the study were evaluated. Prospective and randomized studies provide the best evidence on the efficacy of health care interventions ; therefore, the time and the randomization process were included in the scoring. The absence of a random assignment could be critical because clinicians with a preconceived notion of what causes root resorption may be biased when obtaining their patient sample. Regarding sample size, the numbers of teeth analyzed in each experimental group were evaluated. Because of the genetic predisposition influence for the onset of OIIRR, large samples were given higher scores to reduce variability. Importance was given to patient-selection criteria because external factors that might predispose root resorption should be excluded during patient selection.
With respect to methodologic soundness, descriptions of appliance types, force magnitudes, radiographic examinations before treatment, and accuracy of the diagnoses and measurement methods of OIIRR were evaluated. Different scores were given if the force magnitude was just stated or controlled by a force measurement device. The radiographic evaluation before the study was also considered in the scoring process because it could detect pretreatment root shortening and eliminate patients who were predisposed to root resorption. The varying degrees of magnification of the radiographs and the limitations of 2-dimensional measurement of a 3-dimensional (3D) phenomenon make light microscopy and plain radiographic methods less accurate than quantitative 3D volumetric evaluations. Therefore, these methods were evaluated with lower scores than scanning electron microscopy (SEM), transmission electron microscopy (TEM), confocal laser scanning microscopy (CLSM), or microcomputed tomography (μCT).
Regarding data analysis, we analyzed whether the statistical analysis was appropriate, whether the error of the method was stated, and whether in the data presentation the P value was associated with any measurement of variability, such as confidence interval, range, or standard deviation.
The methodologic quality scores were reported as percentages of the maximum achievable score (21 points): mean score less than 60% indicates low level of evidence; 60% to 70%, moderate level of evidence; and more than 70%, high level of evidence. To account for flaws in design, conduct, analyses, and reporting that might lead to underestimation or overestimation of the true intervention effect (bias), assessments for risk of bias were performed. The risk of selection, performance, detection, attrition, and reporting bias of each study was evaluated and classified. Studies were categorized as having a low risk of bias if 4 or more domains were considered adequate, as having a moderate risk of bias if 3 domains were considered adequate, and as having a high risk of bias if 2 or fewer domains were considered adequate. The full descriptions of the bias classifications are presented in Table III . The risk of bias across the studies was also assessed. Studies conducted by the same research group were compared to check for similarity between patient characteristics (sex, age, number, and so on). If we detected bias across the studies that might have affected the cumulative evidence, the authors were contacted to clarify or confirm the risk of bias.
| Type of bias | Description | Relevant domains |
|---|---|---|
| Selection | Systematic differences between baseline characteristics of the groups that were compared |
|
| Performance | Systematic differences between groups in the care that was provided or in exposure to factors other than the interventions of interest |
|
| Detection | Systematic differences between groups in how outcomes were determined |
|
| Attrition | Systematic differences between groups in withdrawals from a study |
|
| Reporting | Systematic differences between reported and unreported findings |
|
Results
The database search showed 128 articles listed in PubMed, 115 articles in Embase, and 16 articles in Cochrane. Four articles were added after hand searches of the bibliographies of the selected articles and relevant reviews. By using the PRISMA flow diagram, an overview of the article selection process is illustrated ( Fig ). After exclusion of 26 duplicate articles, 237 articles remained. In the first step of the screening process, a further 112 articles were excluded because they were determined to be irrelevant based on the titles and abstracts. In the second step of the screening process, the remaining 125 full-text articles were assessed: 52 articles were excluded because they did not meet the inclusion criteria, and 52 articles were excluded after the application of the exclusion criteria ( Fig ). Thus, the selection process resulted in 21 full-text articles. A summary of the main findings and the data regarding participants, interventions, comparisons, outcomes, study designs (PICOS), and follow-up periods of each study in this systematic review is presented in Table IV . The assessment of the risk of bias across the studies showed that 2 articles were conducted on the same sample of patients (confirmed by e-mail communication from their authors); therefore, these 2 studies were treated as one, and the results were combined.
| Study | Participants | Interventions | Comparisons | Outcomes | Study design | Follow-up | Main findings |
|---|---|---|---|---|---|---|---|
| Harris et al (2006) | 54 maxillary first PM from 27 patients (12 M, 15 F); ages, 11.9-19.3 y; mean, 15.6 y | Orthodontic therapy with fixed appliances (segmented technique) | Force levels: low (25 g) vs heavy (225 g) vs control (0 g) |
|
RCT, SMD | 4 wk | The 3 force level groups were significantly different. Mean volumes of RR in the light and heavy force groups were about 2 and 4 times greater than in the control group. Mesial-apical and distal-apical surfaces had more RR than the other regions, with no statistically significant difference between them. |
| Chan and Darendeliler (2005, 2006) | 36 maxillary and mandibular PM from 16 patients (10 M, 6 F); ages, 11.7-16.1 y; mean, 13.9 y | Orthodontic therapy with fixed appliances (segmented technique) | Force levels: low (25 g) vs heavy (225 g) vs control (0 g) |
|
RCT, SMD | 4 wk | More RR in the heavy force group compared with the light and control groups. Although more RR was recorded in the light force group, no statistically significant difference was found between the light and control groups. Buccocervical and lingual-apical surfaces had more RR than the other regions. |
| Barbagallo et al (2008) | 54 maxillary first PM from 27 patients (12 M, 15 F); ages, 12.5-20 y; mean, 15.3 y | Orthodontic therapy with fixed appliances (segmented technique) and aligners | Force levels and systems: conventional low (25 g) vs conventional heavy (225 g) vs aligner vs control (0 g) |
|
RCT, SMD | 8 wk | More RR in the heavy force group compared with the aligner, light, and control groups. The aligner group had similar effects on root cementum as did the light group. More RR was observed was at the buccocervical and lingual-apical regions in all treated teeth. |
| Weiland (2003) | 90 maxillary and mandibular PM from 27 patients (10 M, 17 F); ages, 10.2-14.5 y; mean, 12.5 y | Orthodontic therapy with fixed appliances (segmented technique) | Loading regimen: continuous vs intermittent vs control |
|
NR-CT, SMD | 12 wk | The teeth with the superelastic wire moved significantly more and tipped buccally to a greater degree than those moved with the stainless steel wire. The teeth moved with the superelastic wire showed significantly more RR, more resorptive damage regarding perimeter, area, and volume of the lacunae than those moved with a stainless steel wire. The cervical resorptions were mainly located on the buccal side, and the apical resorptions on the palatal or lingual side. |
| Owman-Moll et al (1995) | 32 maxillary first PM, from 16 patients (8 F, 8 M); ages 11.8-15.8 y; mean, 13.9 y | Orthodontic therapy with fixed appliances (segmented technique) | Loading regimen and treatment times: continuous vs interrupted forces, applied for 4 or 7 weeks |
|
NR-CT, SMD | 4 or 7 wk | Areas of RR were found on all experimental teeth. No significant difference of resorption was found between the 2 force systems. |
| Bartley et al (2011) | 30 maxillary first PM from 15 patients (7 M, 8 F); ages, 12.75-16.83 y; mean, 14.3 y | Orthodontic therapy with fixed appliances (segmented technique) | Force system: 2.5° vs 15° of buccal root torque |
|
RCT, SMD | 4 wk | No statistically significant differences in RR after the application of either 2.5° or 15° of buccal root torque. More RR at the apical region than at the middle and cervical regions. |
| Wu et al (2011) | 30 maxillary first PM from 15 patients (5 M, 10 F); ages, 11.9-16.9 y; mean, 14.15 y | Orthodontic therapy with fixed appliances (segmented technique) | Force levels: low (25 g) vs heavy (225 g) |
|
RCT, SMD | 4 wk | More RR in the heavy force group than in the light force group. Greater RR in the compression areas (buccodistal and lingual-mesial surfaces) than in other areas at all levels of the root. |
| King et al (2011) | 30 maxillary first PM from 15 patients (4 M, 11 F); ages, 12.8-16.11 y; mean, 14.2 y | Orthodontic therapy with fixed appliances (segmented technique) | Force system: 2.5° vs 15° of distal root tipping |
|
RCT, SMD | 4 wk | Greater RR in teeth that had undergone greater distal root tip bends. Compression of the periodontal ligament caused more RR than tension, which was more pronounced in the apical and cervical thirds of the teeth. |
| Montenegro et al (2012) | 20 maxillary first PM from 10 patients (3 M, 7 F); ages, 12-18 y; mean not mentioned | Orthodontic therapy with fixed appliances (segmented technique) | Force levels: low (25 g) vs heavy (225 g) |
|
RCT, SMD | 4 wk | Greater RR after heavy forces when compared with light forces. The distal surfaces were more affected than other root surfaces. No significant difference between the cervical, middle, and apical thirds in relation to RR. |
| Chan et al (2004) | 20 maxillary first PM from 10 patients | Orthodontic therapy with fixed appliances (segmented technique) | Force levels: low (25 g) vs heavy (225 g) vs control (0 g) |
|
RCT, SMD | 4 wk | More RR in the heavy force group than in the light and control groups. |
| Kurol et al (1996) | 112 maxillary PM from 56 patients (18 M, 38 F); ages, 10.5-17.5 y; mean, 13.8 y | Orthodontic therapy with fixed appliances (segmented technique) | Force levels and treatment times: 50 g applied for 1 to 7 wk vs 0 g (control) |
|
NR-CT, SMD | 1-7 wk | More than 6 times the RR in all test groups compared with the control group. The RR was mainly located in the apical third of the root. The number of teeth with RR increased with time of force application. The PR failed to show any RR occurrence. |
| Casa et al (2006) | 28 maxillary first PM from 14 patients; ages, 13-16 y | Orthodontic therapy with fixed appliances (segmented technique) | Treatment times: 1, 2, 3, or 4 wk vs control |
|
NR-CT, SMD | 1-4 wk | Resorption lacunae and clastic cells increased in extent and number with the duration of the force and were found on the cementum surface at the pressure areas. Some signs of cementum repair were also noticed, even with maintenance of the force level. |
| Paetyangkul et al (2011) | 54 maxillary first PM from 36 patients (21 F, 15 M); mean age, 14.9 y | Orthodontic therapy with fixed appliances (segmented technique) | Force levels and treatment times: low (25 g) vs heavy (225 g), applied for 4, 8, or 12 wk |
|
NR-CT, SMD | 4, 8, or 12 wk | Less RR in the light force group than in the heavy force group. Increased RR from 8-12 weeks of force application with either light or heavy orthodontic forces. |
| Aras et al (2012) | 64 maxillary PM from 32 patients (25 F, 7 M); ages, 12-18 y; mean age, 14.4 y | Orthodontic therapy with fixed appliances (segmented technique) | Force system: continuous vs intermittent force, 2 or 3 weekly reactivations |
|
RCT, SMD | 12 wk | Group of continuous force produced faster TM than intermittent force group. Statistically significant differences regarding the amount of RR between the 2 groups were only observed in the 3 weekly reactivation group. RR decreased when a pause was given, irrespective of the timing of reactivation. Two weekly reactivations of continuous orthodontic force can lead to less RR than 3 weekly reactivations. |
| Harry and Sims (1982) | 36 maxillary and mandibular first PM from 10 patients; ages, 11-18 y | Orthodontic therapy with fixed appliances (segmented technique) | Force levels and time intervals: 50 g vs 100 g vs 200 g. Intervals of 14, 35, and 70 d. |
|
NR-CT, SMD | 14, 35, and 70 d | Surface defects identified with the SEM or macroscopically were not identified on PR. Intrusive forces produced an increase in RR compared with the control teeth. The amount of RR increased with the duration of the force, and to a lesser extent with the magnitude of the activation. More RR was observed at the buccocervical root surfaces and apical thirds of the roots. |
| Paetyangkul et al (2009) | 40 maxillary and mandibular first PM from 10 patients (6 F, 4 M); ages, 12.7-18.2 y; mean age, 14.3 y | Orthodontic therapy with fixed appliances (segmented technique) | Force levels: low (25 g) vs heavy (225 g) |
|
RCT, SMD | 12 wk | Less RR in the light force group than in the heavy force group in both maxillary and mandibular PM. RR greater toward the cervical region on the buccal surfaces and the apical regions on the lingual surfaces. |
| Ramanathan and Hofman (2009) | 49 patients (20 M, 29 F); ages, 9-30.1 y; mean 14.5 y | Orthodontic therapy with fixed appliances (segmented technique and SWA) | Appliance types: basal arch vs 3-component arch vs leveling with SWA. |
|
NR-CT | 6 mo | No statistically significant difference in RR among the 3 groups. |
| Baumrind et al (1996) | Radiographic records of 73 patients (16 M, 57 F); age, at least 20 y, diagnosed with Class I or II malocclusion | Orthodontic therapy with fixed appliances (edgewise appliance). | Maxillary central apical incisor displacement vs ARR |
|
Historic cohort | Variable (1-7 y) | Association of orthodontic intervention with maxillary incisor RR, even when the position of the tooth was the same on the cephalograms. More RR for retraction displacement than displacements in other directions. |
| McFadden et al (1989) | Radiographic records from 38 patients; mean age, 13.1 ± 1.4 y | Orthodontic therapy with fixed appliances (bioprogressive technique). | Intrusion vs root shortening |
|
Historic cohort | 28.8 ± 7.4 mo | Degree of root shortening greater in the maxilla (1.84 mm) than in the mandible (0.61 mm). The most significant factor for occurrence of root shortening was the treatment time. |
| Deguchi et al (2008) | 18 patients (2 M, 16 F); mean ages, 20.7 ± 2.5 y (J-hook headgear group) and 21.5 ± 3.7 y (implant group) | Orthodontic therapy with fixed appliances (edgewise appliance) | Appliance types: implant vs J-hook headgear |
|
NR-CT | 7 mo | Significantly more RR in the J-hook headgear group than in the implant group after intrusion of the maxillary incisors. |
∗ Directions: retraction, advancement, intrusion, and extrusion.
Most studies (90%) were clinical trials, except for 2 historic cohorts. All articles were published in English between 1982 and 2012. Detailed assessments of the methodologic quality and the risk of bias are shown in Tables V through VIII . Methodologic quality scores ranged from 48% to 86% of the maximum achievable score, with a mean score of 72%. Thirteen studies were classified as high (62%), 5 as moderate (24%), and 3 as low (14%) levels of evidence. Eleven studies were considered to have a low risk of bias (52%), 2 had a moderate risk of bias (10%), and 8 were classified as having a high risk of bias (38%). It was not possible to perform a meta-analysis because of the heterogeneous methodologies of these studies.
| Article | Time | Randomization | Control group | Sample size | Selection criteria | Objective | Score |
|---|---|---|---|---|---|---|---|
| Harris et al (2006) | 2 | 1 | 1 | 3 | 1 | 1 | 9 |
| Chan and Darendeliler (2005, 2006) | 2 | 1 | 1 | 2 | 1 | 1 | 8 |
| Barbagallo et al (2008) | 2 | 1 | 1 | 2 | 1 | 1 | 8 |
| Weiland (2003) | 2 | 0 | 1 | 4 | 0 | 1 | 8 |
| Owman-Moll et al (1995) | 2 | 0 | 0 | 2 | 0 | 1 | 5 |
| Bartley et al (2011) | 2 | 1 | 0 | 3 | 1 | 1 | 8 |
| Wu et al (2011) | 2 | 1 | 0 | 3 | 1 | 1 | 8 |
| King et al (2011) | 2 | 1 | 0 | 3 | 1 | 1 | 8 |
| Montenegro et al (2012) | 2 | 1 | 0 | 2 | 1 | 1 | 7 |
| Chan et al (2004) | 2 | 1 | 1 | 2 | 0 | 1 | 7 |
| Kurol et al (1996) | 2 | 0 | 1 | 2 | 0 | 1 | 6 |
| Casa et al (2006) | 2 | 0 | 1 | 1 | 0 | 1 | 5 |
| Paetyangkul et al (2011) | 2 | 0 | 0 | 2 | 1 | 1 | 6 |
| Aras et al (2012) | 2 | 1 | 0 | 3 | 1 | 1 | 8 |
| Harry and Sims (1982) | 2 | 0 | 1 | 1 | 0 | 1 | 5 |
| Paetyangkul et al (2009) | 2 | 1 | 0 | 3 | 1 | 1 | 8 |
| Ramanathan and Hofman (2009) | 2 | 0 | 0 | 3 | 1 | 1 | 7 |
| Baumrind et al (1996) | 0 | 0 | 0 | 4 | 1 | 1 | 6 |
| McFadden et al (1989) | 0 | 0 | 0 | 4 | 1 | 1 | 6 |
| Deguchi et al (2008) | 2 | 0 | 0 | 2 | 0 | 1 | 5 |
| Article | Appliance type | Force magnitude | Radiographic exam BT | Measurement method of RR | Score |
|---|---|---|---|---|---|
| Harris et al (2006) | 1 | 2 | 0 | 2 | 5 |
| Chan and Darendeliler (2005, 2006) | 1 | 2 | 1 | 2 | 6 |
| Barbagallo et al (2008) | 1 | 1 | 0 | 2 | 4 |
| Weiland (2003) | 1 | 1 | 0 | 2 | 4 |
| Owman-Moll et al (1995) | 1 | 2 | 1 | 2 | 6 |
| Bartley et al (2011) | 1 | 1 | 0 | 2 | 4 |
| Wu et al (2011) | 1 | 2 | 1 | 2 | 6 |
| King et al (2011) | 1 | 1 | 0 | 2 | 4 |
| Montenegro et al (2012) | 1 | 2 | 1 | 2 | 6 |
| Chan et al (2004) | 1 | 1 | 1 | 2 | 5 |
| Kurol et al (1996) | 1 | 2 | 1 | 2 | 6 |
| Casa et al (2006) | 1 | 1 | 0 | 3 | 5 |
| Paetyangkul et al (2011) | 1 | 2 | 0 | 2 | 5 |
| Aras et al (2012) | 1 | 2 | 0 | 2 | 5 |
| Harry and Sims (1982) | 1 | 2 | 1 | 3 | 7 |
| Paetyangkul et al (2009) | 1 | 2 | 0 | 2 | 5 |
| Ramanathan and Hofman (2009) | 1 | 1 | 1 | 1 | 4 |
| Baumrind et al (1996) | 1 | 0 | 1 | 1 | 3 |
| McFadden et al (1989) | 1 | 0 | 1 | 1 | 3 |
| Deguchi et al (2008) | 1 | 2 | 1 | 1 | 5 |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


