Introduction
Our objectives were to (1) systematically review the literature on the effectiveness of fluoride-containing adhesives in controlling decalcification in fixed orthodontic patients, (2) determine which fluoride-containing adhesives provide protection against decalcification, and (3) make recommendations on the usage of fluoride-containing adhesives in patients with fixed orthodontic appliances.
Methods
In this systematic review, we searched published and unpublished material in any language using general and specialist databases; key orthodontic journals were searched by hand. Predefined inclusion criteria based on objective outcome measures for decalcification, presence of a comparison group, and the study design were applied to select the studies. Included studies were double extracted onto predesigned data extraction sheets.
Results
A qualitative analysis of 5 randomized controlled trials and 5 clinical trials is presented.
Conclusions
It is impossible to make recommendations on the use of fluoride-containing orthodontic adhesives during fixed orthodontic treatment. However, there is evidence to suggest that (1) glass ionomer cement is more effective than composite resin in preventing white spot formation, but the evidence is weak; (2) further research is required to determine the effectiveness of the various fluoride-containing orthodontic adhesives; and (3) common outcome measures and reporting standards would assist future researchers.
Orthodontic treatment is almost always an elective procedure to improve the patient’s dentofacial appearance. A major barrier in achieving this goal is the potential for patients to develop areas of decalcification adjacent to orthodontic brackets and bands. In the context of fixed orthodontic treatment, such lesions could be considered iatrogenic. The effects of decalcification vary from no perceptible change to white spots on the enamel, or even cavitation. They appear as unsightly lesions on previously healthy teeth at the end of orthodontic treatment. They can require further treatment after orthodontic treatment to mask or remove them.
Studies have shown that decalcification is a significant risk during fixed orthodontic treatment, with rates reported between 2% and 96%. Research suggests that topical fluorides might decrease decalcification during orthodontic treatment. One method of applying fluoride is to incorporate it into the adhesive.
The numbers of fluoride-containing adhesives for orthodontic use increase each year, and both fluoride-containing glass ionomer and composite adhesives have been shown to decrease decalcification in patients with fixed appliances. However, the ability to prevent decalcification is not the only attribute of concern to clinicians, and the volume of information makes it difficult to stay up to date and make a valid conclusion about the most appropriate type of bonding agent to use.
One way to overcome this is to carry out a systematic review of the literature. Information from randomized controlled trials and clinical controlled trials can then be collated, summarized, and regularly updated to aid clinicians in their decisions, enabling them to make an evidence-based choice.
The objectives of this review were to determine whether fluoride-containing orthodontic adhesives are effective in preventing decalcification during fixed appliance treatment and, if possible, to make recommendations for their usage during fixed orthodontic treatment.
Material and methods
Our search strategy for identification of studies followed the methodology outlined by the guidelines of the NHS Centre for Research and Dissemination. The search strategies were cross-disciplinary and included internationally published research. Review articles, published bibliographies, relevant citations in articles, and all languages were included.
Initial searches were carried out on Medline, Embase, CINAHL, the Cochrane Library, and Web of Science. The full search was built on a preliminary scoping search and also the strategy used by the Cochrane review on orthodontic adhesives.
Specialist databases such as the Health Technology Assessment were also searched by using appropriately modified terms. Unpublished “gray” literature was identified by searching SIGLE, ISI Conference Proceedings, Current Controlled Trials Register, and the National Research Register ( Table I ).
| 1 | orthodontic brackets |
| 2 | orthodont: |
| 3 | glass ionomer. |
| 4 | 2 and 3 |
| 5 | composite |
| 6 | 2 and 5 |
| 7 | orthodontic adhesive: |
| 8 | 4 or 6 or 7 |
| 9 | remove duplicates from 9 |
| 10 | 1 and 9 |
| 11 | fluorid: |
| 12 | demineral: |
| 13 | decalcif: |
| 14 | 12 or 13 |
| 15 | remove duplicates from 13 |
| 16 | limit 14 to yr=1966-1990 |
| 17 | remove duplicates from 16 |
| 18 | limit 14 to yr=1991-2003 |
| 19 | remove duplicates from 18 |
| 20 | 17 or 19 |
| 21 | 10 and 11 and 20 |
After the electronic literature search, a hand search to identify recent but uncited publications was undertaken. After liaising with the Cochrane Oral Health group, a selection of journals was identified as incompletely hand-searched and therefore not listed in the Cochrane Oral Health Group’s Trials Register. The following relevant journals were searched once: American Journal of Orthodontics and Dentofacial Orthopedics, Journal of Orthodontics (formerly, British Journal of Orthodontics ), Angle Orthodontist, European Journal of Orthodontics, and Journal of Clinical Orthodontics .
The search was expanded by secondarily searching the references of the selected stage 1 articles and the listed references of the Cochrane systematic reviews on fluoride, orthodontic adhesives, and bands.
The complete search was rerun and updated in October 2008.
Studies that included comparison groups were considered. Thus, randomized controlled trials, clinical trials, and prospective observational studies with concurrent or historic comparison groups were included in the review.
To be of clinical benefit, the fluoride-containing adhesive must be able to prevent decalcification throughout treatment; therefore, this review was restricted to clinical studies of patients who had completed a full course of fixed orthodontic treatment. No reports were excluded on the basis of population or study setting.
From the titles and abstracts derived from the searches, articles were excluded on the basis of nonhuman subjects, laboratory based, nonrelevant (ie, not fixed orthodontic appliances or not using fluoride-containing adhesives), or the entire period of fixed orthodontic treatment was not covered.
From the titles and abstracts derived from the searches, articles were included on the basis of human studies, clinical studies, fluoride-containing adhesives, and fixed orthodontic treatment.
The outcome measure was decalcification at the baseline and the end point of the study. When possible, the total numbers of white spots, decalcifications, and decayed, missing, or filled teeth were recorded for the start and finish of the trial for both subjects and teeth.
Effect modifiers were other factors that might increase or decrease a patient’s likelihood of developing decalcification during orthodontic treatment. The following were identified and, when reported, recorded: level of water fluoridation, caries status of subjects, general health of subjects, oral hygiene of subjects, oral hygiene reinforcement program, socioeconomic status of subjects, use of topical fluoride (other than toothpaste), compliance with topical fluoride regimen, and debonds.
Ten articles were used as a pilot test for the 2 reviewers (S.R., B.C.) to clarify the inclusion and exclusion criteria and to train the reviewers to ensure that the criteria were consistently applied. This phase was also used to refine the data extraction sheet.
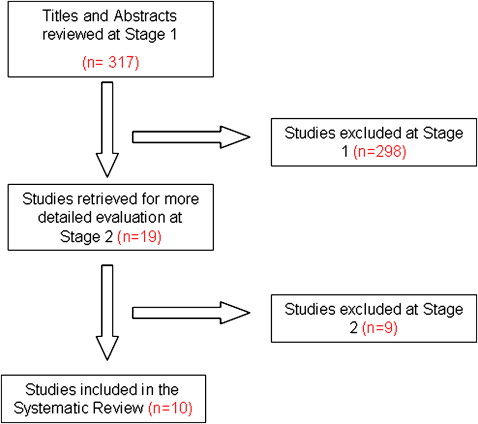
In stage 1, all titles and abstracts were reviewed by 1 reviewer (S.R.) to determine whether each article met the predetermined inclusion and exclusion criteria. If, with the information available, it was determined that an article definitely did not meet the inclusion criteria, it was excluded. If there was any doubt, then the full article was retrieved, and the opinion of the second reviewer was sought (B.C.).
In stage 2, all selected articles were examined by 2 independent reviewers (S.R., B.C.) to determine whether the eligibility criteria were met. At this stage, articles with inappropriate study designs or no outcome measures at both baseline and end point were excluded. For all included studies, a note was made of any flaws in the study design.
In stage 3, all included articles were read, data were extracted, and methodologic quality was assessed by 2 reviewers independently, in duplicate, using specially designed data extraction forms, in accordance with the guidelines of the NHS Centre for Research and Dissemination. Any disagreement was discussed, and a third reviewer was consulted when necessary (E.T.). Five authors were contacted for more information, and 2 responses were received.
Results
Nine studies were excluded at stage 2. Eight studies were bonding studies, reporting on comparative bond strengths, with no assessment of decalcification, and the other study was not relevant ( Fig ).
The 10 included studies used different methodologies, reporting strategies, and various orthodontic adhesives, making a meta-analysis impossible. A qualitative analysis was therefore undertaken. Details of the included studies are given in Table II .
| Country Reference Study design |
Follow-up (mo) | Clinicians Evaluators (n) |
Decalcification assessment Teeth assessed (FDI numbers) | Test adhesive | Control adhesive | Tests (n) | Controls (n) | Decalcification at baseline, test/control | Decalcification at end point, test/control | Debonds number→ %, study (control) | Additional fluoride |
|---|---|---|---|---|---|---|---|---|---|---|---|
| United Kingdom 14 CT |
Debond, 12 | NS 3 |
Photos 13-23 |
Ketac- Cem (GI) | Right-on (composite) | 120 (t) | 120 (t) | 46/45 (t) | 55/53(t) | 20/120 → 16.6 (5/120→4.2) ∗ |
TP |
| United States 8 CT |
Debond | NS NS |
Photos 15-25 35-45 |
FluorEver (LC composite) | Aurafill (LC composite) | 206 (t) | 206 (t) | 0/0(t) | 0/26(t) | 5/206 →2.4 (7/206→3.3) |
NS |
| United Kingdom 27 RCT |
Debond, 3 | NS 1 |
Photos 13-23 |
Direct (composite) | Right-on (composite) | 62 (t) | 62 (t) | 0/0(t) | 11/12 (t) | 4/62 →6.4 (9/62→14.5) † |
NS |
| Belgium 28 CT |
1 week postdebond | NS NS |
Photos 15-25 35-45 |
Orthon LC (composite) | Lee-Insta Bond (composite) | 383 (t) | 379 (t) | 0/0 (t) | 17/26 (t) | NS ∗ | NS |
| Sweden 9 RCT |
Debond, 12, 24 | NS 3 |
Photos 12-22 33-43 |
Aquachem (GI) | Unite (composite) | 111 (t) | 111 (t) | 9/7 (t) | 27/45 (t) | NS | NS |
| United States 15 CT |
Debond | NS 7 |
Photos 13-23 |
Fuji Ortho LC (GI) | Reliance light bond-fluoride releasing (composite) | 48 (t) | 48 (t) | NS | 37/36 (t) | 37/149→24.8 (11/149 →7.4) ∗ |
NS |
| United Kingdom 16 RCT |
Debond | 4 4 |
Clinical NS |
DeTrey Densply (composite) | Concise (composite) | 203 (t) | 203 (t) | 12/10 (t) | 31/41 (t) | 3/203→ 1.5 (6/203→ 2.9) |
MW |
| United Kingdom 17 RCT |
Debond | NS 1 |
Clinical 15-25 35-45 |
Fluoride-releasing Rely-a-bond (composite) | Nonfluoride- releasing Rely-a-bond (composite) | 366 (t) | 371 (t) | 0/0 (t) | 45/54 (t) | 13/366 → 3.6 (10/371 →2.7) |
MW |
| United Kingdom 29 CT |
Debond | 1 2 |
Photos 13-23 |
Dyract (compomer) | Right-On (composite) | 213 (t) | 213 (t) | 9/9 (t) | 23/34 (t) | 37/ 213 →17 (43/ 213 →20) ∗ |
MW |
| United Kingdom 30 RCT |
Debond | NS NS |
Clinical buccal and lingual surfaces of molars | Band-Lok (compomer) | Ketac-Cem (GI) | NS | NS | 19/90 (s) 20/90 (s) |
27/90 (s) 26/90/(s) |
7/140 →5 (4/140 →2.8) (no. bands) |
MW |
∗ Debonds were not included in the decalcification analysis
† Debonded teeth were rebonded with the same material and included in the decalcification analysis.
The single feature common to all included studies was the use of a split-mouth technique.
Five compared fluoride releasing with conventional composite, 3 studies compared glass ionomer cement with composite, and 1 study compared compomer with composite. The final study compared compomer with composite for orthodontic bands.
Only four studies assessed the full mouth for decalcification.
There were 7 indexes used to quantify decalcification. The most commonly used index was a 0-to-3 score. It is an ordinal scale, with 0, indicating no white spots, to 3, indicating cavitation, based on either the index of Gorelick et al or Geiger et al, or the system used by Mizrahi.
Three studies assessed decalcification by direct vision, and the rest used photography.
Most studies assessed decalcification at debond, with only 1 study scoring at 1 week after debond.
Two studies reviewed decalcification over longer times: from debond to a 12-month review and from debond to a review 1 and 2 years later. Both studies reported an overall reduction in decalcification for both groups. However, it was still greater than before treatment.
Only 3 studies reported statistically significant differences in decalcification between the control and the experimental adhesives.
Most studies based the assessment of decalcification on the number of teeth and not on the number of patients. Only 3 studies reported patient numbers.
Millett et al reported the mean numbers of teeth affected by decalcification per patient. They also reported an increase by about 30% during the treatment time: from 2.1 to 2.8 for the experimental adhesive, and 2.1 to 2.7 for the control group. This amounted to an additional tooth affected in both groups.
Trimpeneers and Dermaut assessed remineralization, not decalcification, with their patient numbers, and reported no significant difference between both types of adhesive. In the experimental adhesive group, remineralization was noted in 5 of 19 patients with initial white spots, whereas, in the control adhesive group, this was the case in 14 of 23 patients ( P >0.05).
Gillgrass et al reported the mean enamel white spot lesion scores per patient and the number of patients with decalcification ( Table II ).
The only effect modifier reported in any detail was debonded brackets, which was included by all but 2 studies. In the 4 studies comparing fluoride-releasing and conventional composites, bracket failure rates were similar between the control and the experimental groups ( Table II ). The 1 study comparing compomer with conventional composite also found similar debond rates with both materials. In contrast, the 2 studies comparing glass ionomer with composite reported substantially more failures in the glass ionomer group: 11 of 149 and 5 of 120 debonded brackets in the composite groups compared with 37 of 149 and 20 of 120 in the glass ionomer groups.
The final study compared the band failure rates of a compomer with a conventional glass ionomer and found no significant difference between the failure patterns of the 2 cement groups.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


