Introduction
In this study, we evaluated the effects of bone awl–induced damage to bone surrounding a tooth that was moved.
Methods
A randomized split-mouth design with 7 foxhounds was performed to evaluate protraction of the mandibular third premolars for 56 days with 200 g of orthodontic force. Before initiating tooth movements, a bone awl was used on the experimental side to create 60 buccal and lingual microfracture injuries to the cortical bone without a periosteal flap. Tooth movements were performed on the control and experimental sides. Microcomputed tomography and histology were used to assess bone morphology and modeling. Radiographic and caliper measures were used to assess tooth movements.
Results
The awl-induced injuries produced significant damage and microfractures (95 mm 3 ). Buccal and lingual cortical bone volume fractions and densities were significantly less and cortical modeling was significantly greater on the experimental sides than on the control sides. Bone volume fractions and densities mesial to the third premolars were the same on the experimental and control sides. Experimental side tooth movements (1.40 ± 0.25 mm) were statistically the same as the control side tooth movements (1.57 ± 0.45 mm).
Conclusions
The effects of flapless, bone awl−induced damage were limited to the cortical bone. Because there was no effect on the medullary bone mesial to the tooth being moved, no differences in tooth movements were produced.
Highlights
- •
Flapless, bone awl–induced damage causes cortical bone modeling.
- •
It is associated with significant decreases in buccal and lingual cortical bone volume and density.
- •
Bone awl–induced damage has no significant effects on mesial medullary bone volume and density.
- •
Bone awl–induced damage has no significant effect on mesial tooth movements.
- •
Extensive injuries to the cortical bone alone around a tooth do not accelerate tooth movement.
According to the American Association of Orthodontists, the length of comprehensive orthodontic treatment ranges from approximately 18 to 30 months, depending on the difficulty of the malocclusion and the patients’ characteristics. With prolonged orthodontic treatments, the risks of root resorption, decalcification, dental caries, and periodontal problems significantly increase. To minimize these risks, orthodontists are continually trying to decrease treatment times in a manner that will yield results comparable to or better than accepted traditional modalities.
Currently, corticotomies are perhaps the most popular method used for accelerating orthodontic tooth movement by inducing the regional acceleratory phenomenon, which has experimentally been shown to double the rate of movement. Although traditional corticotomies accelerate tooth movements with minimal long-term side effects, some postoperative swelling and pain are expected for several days. Complications associated with corticotomies range from slight interdental bone loss and loss of attached gingiva to periodontal defects, which can occur with short interdental distances. Subcutaneous hematomas in the neck and face have also been reported after more invasive corticotomies.
In an effort to reduce postsurgical morbidity, alternative surgical procedures have been introduced. Kim et al penetrated the cortical bone with a reinforced surgical blade and mallet, thus eliminating the need for a periosteal flap. They observed accelerated tooth movements and less postsurgical discomfort, but the blade penetrated 10 mm into the bone, which is much deeper than a corticotomy. Traditional corticotomies are limited to the cortical bone, which is 1 to 2 mm thick, depending on the location. Dibart et al also performed corticotomies without a periosteal flap. After accessing the bone with interdental gingival incisions, they used a piezosurgery device for the corticotomies. Claims of accelerated tooth movement and reduced patient morbidity were premature due to the lack of controls. Although eliminating the need for periosteal resection during the procedure can reduce postsurgical morbidity, it remains unknown whether bone damage limited to the cortices will provide a sufficient modeling stimulus to accelerate tooth movement.
Microfracture surgery is a method for minimizing periosteal damage while maximizing cortical bone damage. It is used by orthopedists to repair damaged articular cartilage in the knee. The surgery involves the use of a bone awl to create small perforations (microfractures) in the subchondral bone plate of the defective area. The benefit of using this surgery in lieu of corticotomies is that microfractures cause more bone destruction and osteocyte death than lesions incurred by drilling, and greater amounts of bone damage are related to greater tooth movements. If microfracture surgery causes more damage than drilling, it is more likely to initiate sufficient modeling to accelerate tooth movement. The procedure is also less invasive because there is no incision or flap, and it can be limited to the cortical bone.
The primary purpose of this study was to determine the effects of cortical bone injuries alone on the bone surrounding teeth that will be moved. Microcomputed tomography and histologic analysis were performed to analyze bone density and the modeling patterns associated with the injuries that were produced. The effect of bone awl–induced damage on tooth movements was a secondary outcome that was evaluated. Unlike previous studies that have cut the periosteum or produced osseous damage well beyond the cortical region, we limited the insults to the buccal and lingual cortical plates.
Material and methods
Seven skeletally mature male foxhounds, 1 to 2 years of age, were used in the experiment. The sample size was based on previous similarly designed studies showing significant surgically induced differences in tooth movements. The dogs had fully erupted dentitions and weighed 25 to 30 kg. The housing, care, and experimental protocol were approved by the Institutional Animal Care and Use Committee at Baylor College of Dentistry, Dallas, Texas. The canine model was selected because it is well established for investigating tooth movements and bony adaptations. After a 10-day quarantine, ultrasonic prophylaxis and initial records were taken; these consisted of alginate impressions, photographs, and radiographs. The dogs were fed soft dog food and water to minimize damage to the experimental orthodontic appliances.
Triad custom tray material (Dentsply, York, Pa) was used to make mandibular alginate impressions. The impressions were poured in die stone, and the resultant models were used to fabricate the appliances. Orthodontic bands were custom made with band material (Dentaurum, Ispringen, Germany) and adapted to the mandibular canines and third premolars. Headgear tubes (diameter, 1.30 mm) were soldered to the orthodontic bands of the third premolars. Orthodontic wires (diameter, 1.14 mm) were soldered to the canine bands and inserted through the headgear tubes on the bands of the third premolars. The third premolars were able to move freely along the wire ( Fig 1 , A ).
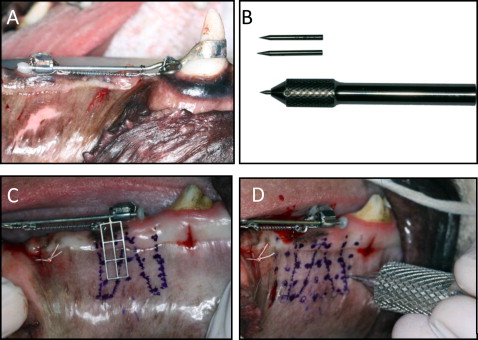
The bone awl handle was custom machined (Custom Scientific, Dallas, Tex) from a surgical stainless steel rod 88 mm long and 9.5 to 12.5 mm in diameter. At one end was a 1.5-mm-diameter hole that was 20 mm deep. The hole allowed individual awl points to be inserted and removed, with a hex lock incorporated into the awl handle to secure the awl points in place. The awl points were fabricated from 1.5-mm-wide high-speed steel rods ( Fig 1 , B ). The overall lengths of the awl points were 25 or 26 mm. The awl points extended 5 or 6 mm from the awl handle, with 3 to 4 mm tapered to a sharp point. Removable points made it possible to change the awl point length depending on the location of the insult. In addition, if a point fractured or became dull, it could also be changed without replacing the instrument.
The second premolars were extracted 4 weeks before the start of the experiment to minimize the potential regional acceleratory phenomenon effects of surgery. The animals were sedated with ketamine (2.2 mg/kg intramuscularly) and xylazine (0.22 mg/kg intramuscularly), followed by intubation and delivery of 1.5% isolflurane in oxygen at 1 L per minute. Vital signs were monitored throughout all procedures and maintained within normal physiologic limits. Local anesthesia (2% lidocaine with 1:100,000 epinephrine) was administered (approximately 1 carpule per side) via regional infiltration and an inferior alveolar block. The second premolars were sectioned, elevated, and extracted bilaterally.
On the day of appliance delivery and microfracture surgery (day 0), the animals were sedated with the same protocol as used for the extractions. The canines and third premolars were prepared for bonding by removing calculus and debris with a 30-fluted football bur. Hemostasis, if needed, was achieved using Viscostat (Ultradent, South Jordan, Utah). Retention grooves were cut around the circumference of the canines and third premolars, close to the gingiva where the band would be cemented. The teeth were etched with 37% phosphoric acid gel for 25 seconds. After irrigation and drying, the premolars were coated with All-Bond 3 (Bisco, Schaumburg, Ill) primer followed by the associated resin. The Ortholux LED curing light (3M Unitek, Monrovia, Calif) was used for 45 seconds to cure at each step. While the teeth were being prepared, the appliance bands were filled with Transbond XT (3M Unitek). The appliances were seated as 1 unit on the canines and third premolars, excess cement was removed, and the cement was cured on each band. Composite was placed on the distal end of the wires to minimize discomfort.
Radiographic stents were also fabricated from the mandibular models. Triad custom tray material was adapted to the crowns of the mandibular fourth premolars and first molars, with an arm that extended mesially. The arm held an intraoral anterior bite-block film holder that aligned with the third premolar, which was located extraorally. A size 4 film was placed in the film holder, and x-rays were emitted from the contralateral side.
Before we inserted the bone markers, local anesthesia (2% lidocaine with 1:100,000 epinephrine) was administered (approximately 1/4 carpule per bone marker location) via local infiltration. Tantalum bone markers, 0.75 mm long and 0.7 mm in diameter, were placed in the distal crest of the first premolar alveolar ridge and between the roots of the fourth premolars. The markers were placed after making a small (2-3 mm) gingival incision, reflecting the soft tissue, and drilling a 2-mm-deep hole into the cortical bone with a 330 carbide bur. The markers were inserted into the holes, and the gingival tissues were replaced to cover the markers, which served as stable references during treatment.
The surgical side was randomly chosen. A radiographic guide was attached to the buccal tube to locate the roots of the third premolar ( Fig 1 , C ). The locations of the holes to be made with the awl were marked on the soft tissue using a grid of dots 4 mm apart. The grid started at the alveolar ridge and extended approximately 18 mm inferior to the root apices on the buccal side ( Fig 1 , D ). On the lingual side, the grid extended down to the sublingual mucosa, approximately 8 mm from the alveolar ridge. In the mesiodistal direction, the grid began just distal to the distal root outline and extended 5 to 6 mm in front of the mesial root (28 mm total) on both the lingual and buccal surfaces. The dimensions of the grids were approximately 24 × 16 mm and 24 × 8 mm on the buccal and lingual sides, respectively. Markings were also made on the alveolar ridge 4 mm anterior to the mesial root and immediately mesial and distal of the respective roots. On average, there were 35 awl sites marked on the buccal side and 21 sites on the lingual side. Four additional sites were placed on the alveolar ridge mesial and distal to the third premolars.
After marking the surgical sites, the bone awl was used to create the microfractures. The point of the awl was placed on the mark with pressure applied to push through the mucosa and achieve bone contact. A mallet (160 g) was used to drive the awl point into the bone. The awl was struck firmly 2 or 3 times with the mallet to ensure maximum penetration. The 5-mm awl point was used on the buccal bone over the third premolar roots; the 6-mm awl point was used on the remaining buccal locations. Only the 5-mm awl was used on the lingual bone. Minimal bleeding occurred after the surgery, and no postsurgical suturing was required.
After surgery, the appliances were activated by attaching a 9-mm heavy nickel-titanium coil (3M Unitek) from the third premolar to the canine using 0.012-in stainless steel ligatures. The springs were activated to 200 g, which was verified with a force gauge (Correx; Haag-Streit, Bern, Switzerland). Postoperative radiographs and measurements were taken. The management of postoperative pain was accomplished with the administration of buprenorphine, 0.01 to 0.02 mg per kilogram subcutaneously, every 12 hours, as needed. Clindamycin, 5 mg per kilogram intramuscularly, was administered every 12 hours for 5 days for postoperative infection prophylaxis. At the time of surgery, ketoprofen, 2 mg per kilogram intramuscularly, was administered to help reduce inflammation. Premolar protraction continued for 56 days, with periodic force measurements taken to ensure a constant mesial force.
To analyze the initial response to microfracture surgery, 2 dogs received 8 microfracture injuries with only the 5-mm awl 3 days before they were euthanized (day 53). Six injuries were located on the buccal and lingual cortical bone between the first molar roots, approximately 6 mm below the furcation. The additional 2 awl injuries were located between the fourth premolars and first molars approximately 2.5 mm from the alveolar crest on each side. The injuries were made to compare the sizes achieved at different locations on the alveolar bone.
To evaluate the amount and location of subsequent bone modeling, tetracycline (25 mg/kg intravenously) was administered on days 0 and 42, and calcein (10 mg/kg intravenously) was administered on day 21.
Intraoral measurements and radiographs were taken every 2 weeks by 1 observer (A.S.) starting on the day of surgery and continuing for 8 weeks. To standardize the intraoral measurements, notches were cut into the cusp tip of the third premolar and at the most gingival aspect of the mesiobuccal groove of the first molar. Digital calipers were used to measure the distance between these 2 points. The distance was measured twice at each measurement occasion and averaged. Standardized radiographic measurements were taken at a constant distance and angle using a customized film holder that was made to fit over the fourth premolars and first molars (ie, teeth not involved in the tooth movements). Digital periapical radiographs were analyzed using a custom protocol in Viewbox (version 3.1; DHAL Software, Kifissia, Greece). Two points were digitized including the distal cementoenamel junction of the third premolar and the mesial cementoenamel junction of the fourth premolar. From these 2 points, a horizontal line was drawn, and the distance between them was measured at each time point. On day 56, all animals were again sedated with ketamine (2.2 mg/kg intramuscularly) and xylazine (0.22 mg/kg intramuscularly) and euthanized. The mandibles were sectioned and stored in 70% ethanol. The intraclass correlation of the averaged replicate measures was 0.991; there was no significant systematic difference between the replicates.
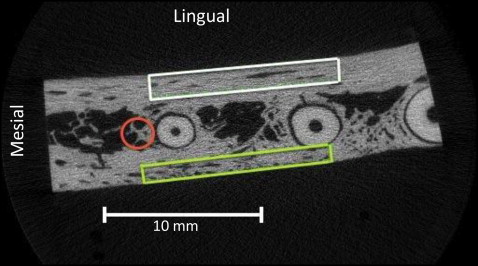
After the dogs were euthanized, all specimens were sectioned to fit in 30-mm tubes and scanned using a SCANCO μCT 35 scanner (SCANCO Medical, Bassersdorf, Switzerland). Each specimen included the section of the mandible just mesial to the fourth premolar and extended mesially 30 mm ( Fig 2 ). This captured the entire surgical site and the third premolar. The specimens were imaged at 30.0-μm resolution, 55 kVp, 145 μA current, and 600 ms integration time. Buccal, lingual, and mesial volumes of bone were segmented and analyzed with the SCANCO software ( Fig 2 ). Bone volume/total volume, apparent bone density, and material bone density were measured on both the control and the experimental sides. The dimensions of the buccal bone volume were approximately 22 × 3 × 1 mm. Its inferior limit was located 3 mm coronal to the apex of the distal root of the third premolar, and the superior limit was 3 mm coronal from the inferior limit. The lingual bone volume was approximately 22 × 4.5 × 1.5 mm. Its superior limit was located 3 mm apical to the furcation of the third premolar and extended apically 4.5 mm. The anterior limit was flush with the anterior border of the mesial root. The mesial segment of bone was determined by drawing a line that bisected the mesial and distal roots and then marking a 2-mm-diameter circle of bone centered on the bisecting line and tangent to the anterior border of the mesial root. This section of bone started 3 mm below the furcation of the third premolar and extended apically 4.5 mm. Only the mesial bone was measured because it was in the direct path of the tooth movement. After defining the volumes of interest, the images were smoothed with a Gaussian filter with sigma equal to 0.9 and support equal to 1. The volumes were segmented at a threshold of 342, which corresponds to a mean linear attenuation coefficient of 563 mg hydroxyapatite per cubic centimeter.
From the 2 dogs that each received 8 microfracture injuries (4 buccal and 4 lingual) 3 days before they were euthanized, the diameter, surface area, and depth of the injuries were estimated using software (μCT version 6.0; SCANCO Medical). The diameter and area of the holes were measured at the first slice showing a complete circumference of bone around the bone awl injury. The volume was estimated using this formula: (area × height)/3.
Five injuries that were inflicted 3 days before the dogs were euthanized were specially prepared to better visualize the location and size of microfractures produced with the awl. The gingival tissues were removed, and the samples were sectioned to separate the buccal and lingual cortices. For microfracture detection, the samples were stained by BaSO 4 precipitation. The specimens were soaked in a solution of equal parts of buffered saline solution, acetone, and 0.5 mol per liter of BaCl 2 (certified ACS crystal; Fisher Scientific, Fair Lawn, NJ) in distilled water for 3 days, followed by a solution of equal parts buffered saline solution, acetone, and 0.5 mol per liter of NaSO 4 (anhydrous powder; Fisher Scientific) in deionized water for 3 days, both under vacuum (about 50 mm Hg). Specimens were rinsed with deionized water after each step to minimize ions or particles on specimen surfaces. The staining mechanism was a precipitation reaction where BaCl 2 (aq) + Na 2 SO 4 (aq) → BaSO 4 (s) + 2NaCl (aq). Barium and sulfate ions diffused into and concentrated within void spaces in the tissues, such as microcracks, damaged tissues, and vasculature.
These specimens were imaged with the scanner at 10.0-μm resolution, 70 kVp, and 114 μA current, and 600 ms integration time. Gray-scale images were smoothed by a Gaussian filter with sigma equal to 3 and support equal to 5. The volume was segmented at a threshold of 861 (mean linear attenuation coefficient of 1664.5 mg hydroxyapatite/cm 3 ). Microfracture damage was measured by comparing the amount of bone affected by microfractures to the initial size of the awl injury. Measurements were taken at the computed tomography slice that was closest to the cortical bone surface and had at least 1 mm of visible bone surrounding the awl injury. After segmentation, the microfractures appeared white, and the area of affected bone was measured. The volume of microfractured bone was also calculated using the same parameters.
Histologic analyses were performed on samples from 3 dogs. Two were cross-sectioned along the long axis of the third premolar. One was cross-sectioned parallel to the buccal surface, where the initial microfracture surgery was performed. Tetracycline and calcein staining were visualized and photographed under an Eclipse 80i microscope (Nikon, Tokyo, Japan). Modeling adjacent to the bone awl injuries was described.
Statistical analysis
The data were described with means and standard deviations. The experimental and control sides were compared using Wilcoxon signed rank tests. A significance level of P ≤ 0.05 was used for all statistical comparisons. To determine the possible effects that damaged appliances might have had, the rates of tooth movement were calculated after eliminating time points that could have been affected by broken appliances or severely bent wires.
Results
Immediately after surgery, no dogs showed significant signs of swelling or severe damage to the periodontal tissues. Tissues on the experimental side appeared similar to those on the control side within 7 days after surgery. During the experiment, all but 1 dog had damaged appliances ( Table I ). All appliances were repaired within 1 day after detection; the maximum amount of time that tooth movements could have been stopped was 1 week.
| Broken appliances | Severely bent wire | Total | |||
|---|---|---|---|---|---|
| Control | Experimental | Control | Experimental | ||
| Dog A | 0 | 3 | 0 | 0 | 3 |
| Dog B | 2 | 3 | 0 | 1 | 6 |
| Dog C | 2 | 1 | 0 | 2 | 5 |
| Dog D | 0 | 0 | 0 | 1 | 1 |
| Dog E | 1 | 1 | 0 | 0 | 2 |
| Dog F | 0 | 0 | 0 | 0 | 0 |
| Dog G | 0 | 1 | 3 | 2 | 6 |
| Total | 5 | 8 | 3 | 7 | 23 |
Tooth movements
Neither the intraoral nor the radiographic measurements showed statistically significant differences in tooth movements between the experimental and control sides ( Table II , Fig 3 ). For the intraoral measurements, the cumulative movements were 1.56 and 1.40 mm for the control and experimental sides, respectively. The average rates of tooth movement were 0.78 mm per month on the control side and 0.70 mm per month on the experimental side. Radiographically, the cumulative movements for the control and experimental sides were 1.14 and 0.91 mm, respectively. The average rates of tooth movement were 0.57 mm per month on the control side and 0.46 mm per month on the experimental side.
| 0 days | 14 days | 28 days | 42 days | 56 days | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | |
| Intraoral measurements | ||||||||||
| Control | 0 | 0 | 0.36 | 0.17 | 0.63 | 0.57 | 1.07 | 0.72 | 1.57 | 1.2 |
| Experimental | 0 | 0 | 0.30 | 0.21 | 0.46 | 0.30 | 1.06 | 0.60 | 1.40 | 0.65 |
| Radiographic measurements | ||||||||||
| Control | 0 | 0 | 0.21 | 0.04 | 0.57 | 0.32 | 0.86 | 0.61 | 1.14 | 0.81 |
| Experimental | 0 | 0 | 0.20 | 0.13 | 0.34 | 0.33 | 0.61 | 0.35 | 0.91 | 0.43 |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


