8 Fine-Needle Aspiration Cytology and Frozen Sections in Salivary Gland Diseases
The Role of Frozen-Section Diagnosis
The Role of Core-Needle Biopsy
Introduction
Fine-needle aspiration cytology (FNAC) is a well-established tool for investigating many head and neck conditions. Its use in patients with major salivary gland swelling continues to be a matter of controversy amongst some head and neck surgeons. Many patients with malignant salivary gland neoplasms present with almost no symptoms suggesting malignancy, and it has therefore been recommended that FNAC should be used as a routine preoperative diagnostic test before surgical excision. The aim of cytological examination is to determine whether the tumor process is inflammatory and/or reactive, benign, or malignant, and if possible to give a specific diagnosis.
It has been argued that even when neoplasms are suspected in salivary gland swellings, the surgical management is not heavily dependent on a specific preoperative diagnosis, as almost all patients with a neoplastic salivary gland lesion undergo surgical excision in any case. However, knowing beforehand whether a lesion is malignant or benign may aid in surgical planning and may expedite or delay the decision in favor of surgery. It may also be helpful for patient counseling and may reduce the number of unexpected pathological findings.1–7
Ultrasound can increase the accuracy of sampling and make it more likely that a representative specimen from the disease process will be obtained, particularly if the lesion being investigated in a deep location or the lump has cystic components. However, adequately trained cytopathologists with the requisite skills, experience, and regular workload are essential for good results to be obtained. A repeat FNAC may provide a cytological diagnosis in cases in which the initial diagnosis is not clear,8 but cytology should be used in conjunction with other investigations, including the patient history, clinical examination, and imaging methods for suspected salivary tumors; image-guided biopsy examinations should also be carried out when appropriate.
 The most important prerequisite for FNAC is to have a cytopathologist with experience in the cytology of salivary gland diseases.
The most important prerequisite for FNAC is to have a cytopathologist with experience in the cytology of salivary gland diseases.
Informed Consent
It is currently essential to explain to the patient the nature and purpose of the procedure, its format, and the risks, benefits, and alternative approaches available. This allows the patient to reach a voluntary and informed decision. The modern approach to informed consent involves a process of mutual communication, rather than simply having the patient place a signature on a standard form. Information leaflets answering patients’ questions in advance are helpful in departments with a high FNAC workload. The member of staff carrying out the aspiration should explain the steps involved in the procedure and also should give a running commentary during the examination in order to reassure the patient.
Equipment Required
Needles of various calibers, no larger than 21 gauge and preferably 23 gauge, are needed. Needles thicker than 18 gauge increase the risk of bleeding. A variety of syringes (20, 10, 5 mL), a syringe holder (e.g., Cameco Syringe Pistol, Precision Dynamics Corporation, California, USA), glass slides (coated and uncoated; preferably with a frosted end), alcohol swabs, universal containers (empty and containing transport medium), gauze swabs, a wound plaster, a pencil, rubber gloves, a protective mask, and an apron are recommended. In most cases, a local anesthetic (2% lidocaine without epinephrine) is not needed. The contents of the FNAC workbox should be clearly listed in a container or case containing the equipment necessary and checked before each clinic session in which FNAC is likely to be performed.
The slides are stained using one of the rapid stains that are available to apply to the specimens obtained. It is useful if a microscope and the relevant expertise are also available, so that the adequacy of the aspirated material can be evaluated while the patient is still present. It has been reported that the average rate of nondiagnostic FNAC without on-site evaluation is 20%, and this figure can be substantially reduced to less than 1% with on-site evaluation.9
If the procedure is being carried out on an outpatient basis, the patient should be placed in a comfortable position. If the procedure is being done on an inpatient basis, it is probably best performed at the bedside. In the outpatient setting, an examination couch is needed. A standard request form should be completed, and all the appropriate and relevant information has to be communicated to the cytopathologist who will be analyzing the specimen and reporting on the FNAC.
 The minimum equipment for FNAC is: 23-gauge needles, glass slides, and a container. A needle holder and access to an ultrasound machine are recommended.
The minimum equipment for FNAC is: 23-gauge needles, glass slides, and a container. A needle holder and access to an ultrasound machine are recommended.
Physician
The responsibility for the procedure should lie with a physician who has the necessary expertise in performing FNAC. It would seem to be best practice for the head and neck surgeon himself or herself to be trained in taking the specimen. Depending on local circumstances and the local organization, the member of staff carrying out the procedure could also be the radiologist or cytopathologist. Although FNAC is a simple procedure, the ability to locate the lesion, correctly insert the needle, and collect cells for analysis is a sequence that requires operator skills that are sometimes underestimated. It has been estimated that approximately 250 passes are required before consistently good results can be expected when performing FNAC. The effects of various factors on the sensitivity of the technique have been investigated. Small tumor size, certain types of tumor, and lesions that are difficult to palpate all lead to reduced sensitivity.
Fig. 8.1 Fine-needle aspiration with ultrasound guidance. The needle and needle holder are positioned at right angles to the head of the ultrasound device.
If the lump is palpable, it needs to be fixed or stabilized to ensure that it remains in the same position while the needle is passed in several different directions. This is best achieved using the fingers of the nondominant hand, with the lump being held between the index finger and third finger. The physician needs to have a good knowledge of the local anatomy in order to avoid complications such as bleeding in salivary gland swellings.
Imaging methods such as ultrasound or computed tomography help improve the diagnostic accuracy and reduce the complication rate when swellings are in a deeper location, with small and multiple nodules, and when there is a cystic component associated with a mass lesion (Fig. 8.1). In these situations, ultrasound makes it possible to take a first specimen from the capsule (border) of the lesion, with a second, separate aspiration being taken from the cystic contents (Fig. 8.2). If the FNAC is being carried out on an outpatient basis, the procedure should ideally take place in the ultrasound room. This allows easy and fast access whenever ultrasound is considered necessary during the procedure.
 If it is not easy to fix the lump between the fingers and when lesions are in deeper locations, one should not hesitate to request ultrasound guidance in order to improve the accuracy.
If it is not easy to fix the lump between the fingers and when lesions are in deeper locations, one should not hesitate to request ultrasound guidance in order to improve the accuracy.
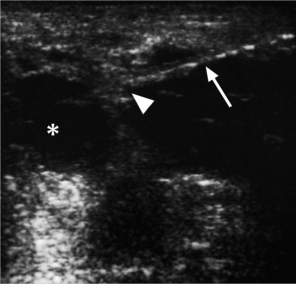
Fig. 8.2 Fine-needle aspiration with ultrasound guidance. There is a hypoechoic lesion in the parotid gland on the left side (*), and the fine needle for aspiration cytology is seen on the right. The needle (arrow) is entering the tissue and puncturing the capsule of the cystic lesion (arrowhead).
Aspiration Techniques
 Suction FNAC
Suction FNAC
Using this method, the needle is passed into the lesion and negative pressure is applied using a syringe, or preferably a syringe holder (see above under “Equipment Required”). This method is particularly useful when draining fluid or liquid from a cyst or a collection. However, it is important to release the negative pressure before the needle is withdrawn from the lesion or lump. If this is not done, then material from the needle may be aspirated into the syringe after it has exited from the lump, and it becomes more difficult to expel the contents. The contents are easier to deliver if a cell solution is made. If the negative pressure is released before the needle is removed from the lump, the cellular material remains contained within the lumen of the needle and its hub.
The needle is then detached from the syringe, and the material is expelled onto a glass slide. If blood has been aspirated, the aspiration and the syringe should be discarded and the whole procedure should be repeated. If the examiner is uncertain whether suitable or sufficient material has been obtained, the procedure should be repeated and additional slides prepared. Additional aspirations improve the accuracy of FNAC procedures.
 Bloody aspirates should be discarded, and FNAC should be repeated whenever there is any uncertainty about the adequacy of the procedure or the specimen obtained, or when a report is received suggesting that the specimen is inadequate or equivocal.
Bloody aspirates should be discarded, and FNAC should be repeated whenever there is any uncertainty about the adequacy of the procedure or the specimen obtained, or when a report is received suggesting that the specimen is inadequate or equivocal.
< div class='tao-gold-member'>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses