History
The first case of microvascular bone transfer of a vascularized myo-osseous segment of fibula to treat a post-traumatic tibial defect was reported by . All cases that followed did not include a skin paddle.
Description of the harvesting technique for this composite fibula flap by Gilbert in 1981 via the lateral approach allowed direct visualization of the perforating cutaneous branches of the peroneal artery and provided the basis for safe inclusion of a skin paddle with the bone flap.
Hidalgo in 1989 performed the first mandibular reconstruction with a segment of fibula by using multiple defined osteotomies to reproduce the shape of almost an entire mandible. Since then the fibula free flap has enjoyed much popularity for mandibular reconstruction and has continued to undergo technical developments. Variable skin paddle positions relative to the bone, harvesting of two separate skin paddles for reconstruction of composite through-and-through defects of the face, the use of sensate skin islands, and the “double-barreled” fibula flap to improve restoration of bone height have all been described.
Surgical Anatomy
The fibula is a long thin non–weight-bearing bone of the lower extremity. It has a tubular shape with a thick circumference of cortical bone providing it with significant inherent strength. Approximately 22 to 25 cm of bone may be harvested while preserving 6 to 7 cm of bone proximally and distally to maintain integrity and functional stability of both the knee and ankle joints, respectively. An additional limitation of proximal dissection is the common peroneal nerve, which wraps around the neck of the fibula.
The fibula can be harvested as a free osseous or free osteoseptocutaneous flap. The inclusion of an overlying skin paddle is possible because septocutaneous or musculocutaneous perforators from the peroneal artery and vein provide a viable blood supply to this area of skin.
The peroneal artery and vein represent the dominant blood supply and vascular pedicle for the fibula osteocutaneous flap. Classically, the popliteal artery divides into the anterior and posterior tibial arteries below the knee, with the latter vessel subsequently giving rise to the peroneal artery. The peroneal artery and its paired venae comitantes descend in the lower part of the leg between the flexor hallucis longus and tibialis posterior muscles as they course toward the foot.
The peroneal artery via a nutrient medullary artery, along with multiple periosteal feeding vessels, provides a rich endosteal vascular supply to the fibula. The vascular supply to the skin over the fibula arises from numerous fasciocutaneous perforators running in the posterior crural septum. Their position and course may be highly variable. The amount of skin that can be harvested is usually limited by the ability to primarily close the defect, although skin grafting of the donor site defect is also frequently performed successfully.
The sensory supply to the skin over the lateral aspect of the calf is derived from the lateral sural cutaneous nerve, a branch of the common peroneal nerve, arising within or above the popliteal fossa. When harvested as part of the osteocutaneous fibula flap it can provide variable sensation to the accompanying skin paddle.
Pathologic Anatomy
Hypoplasia or complete absence of the fibula with replacement solely by a fibrous band is a rare phenomenon that is clinically apparent as a shortened leg and abnormally bowed tibia.
Anatomic variations in the vasculature supplying the lower part of the leg and foot are of greater relevance and concern when using the fibula free flap for bony reconstruction. Normally, the peroneal artery contributes minimally to the vascular supply of the foot, with the dominant supply being provided by the anterior and posterior tibial vessels. In 10% of cases, these two normally dominant vessels may be significantly attenuated or individually absent. In such circumstances, the primary vascular supply is derived from the peroneal artery (peroneal arteria magna), and sacrifice of it will result in limb-threatening ischemia of the foot.
Diagnostic Studies
The goal of preoperative arteriography with respect to the free fibula flap is to identify patients in whom harvest of this flap would result in either a non-viable flap or compromised extremity. Though controversial, it is generally thought by most reconstructive surgeons that angiography for imaging of the lower limb vessels is the “gold standard” for preoperative assessment of patients. However, it is still routine practice in many centers to rely solely on preoperative clinical assessment.
Non-invasive clinical assessment begins with a thorough patient history and general physical examination. Claudication with walking should alert the clinician to underlying occlusive arterial disease. A more detailed examination of the perfusion status of the lower part of the leg and foot is performed to look for signs of limb deformity, previous surgery, or trauma. Stigmata of peripheral arterial or venous vascular disease include skin pallor or cyanosis, ulceration, cool skin temperature, sparse hair growth, and thickened nail beds. Palpation of the popliteal, posterior tibial, and dorsalis pedis pulses is mandatory. Questionable or absent pulses should be investigated further with Doppler flow assessment.
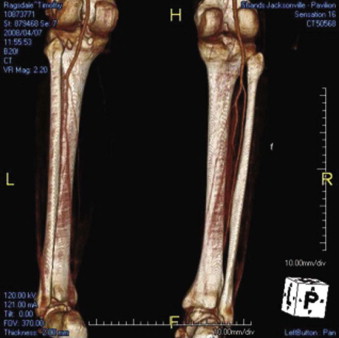
Conventional angiography, computed tomographic angiography, or magnetic resonance angiography, though more invasive, provide superior anatomic detail and functional assessment of the adequacy of limb perfusion and quality of the donor vessels ( Fig. 70-1 ).
Angiographic findings precluding use of the fibula as a reconstructive donor site can be either congenital or acquired. Congenital conditions include peroneal arteria magna. Acquired conditions include a history of lower limb trauma and peripheral vascular disease, both of which can significantly diminish the vascularity of the lower extremity. reviewed a large series of lower extremity angiograms and identified numerous vascular anomalies. In their patients, hypoplasia or absence of the anterior tibial artery was noted in 4%, hypoplasia or absence of the posterior tibial artery was seen in 2%, and a dominant peroneal supply to the lower limb was present in 7%. Congenital absence of the peroneal vessels was estimated to occur in 0.1% of the population by .
Finally, routine use of preoperative angiography must be weighed against the risk for associated complications, including arterial occlusion, aortic dissection, renal failure, nerve injury, intimal damage, hematoma, and anaphylaxis, which occur at an incidence as high as 5%.
Aside from the donor site, equal attention must be given to the recipient site in question. The site and size of the anticipated mandibular defect can often be evaluated clinically and radiologically with a plain panoramic radiograph or computed tomography scan. Knowledge of the nature of the mandibular pathology is important with respect to any concomitant neck surgery required. Knowledge of the extent of neck surgery for malignant disease is paramount to the reconstructive surgeon with regard to adequate availability of recipient vessels for microvascular anastomosis. This issue is even more important in patients with previous neck surgery, specifically previous neck dissection, in which sacrifice of typical recipient vessels was warranted for clearance of disease. In such cases, neck angiography may also be necessary to define the availability, position, and caliber of possible recipient vessels.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


