Introduction
The frontal occlusal plane of the maxilla generally inclines toward the ipsilateral side of the mandibular deviation in subjects with facial asymmetry; however, a few patients with facial asymmetry have their frontal occlusal planes inclined toward the contralateral side. We aimed to investigate the morphologic and functional features of such patients.
Methods
The subjects were 40 patients with facial asymmetry divided into 2 groups based on the inclination of the frontal occlusal plane toward the ipsilateral or the contralateral side. We analyzed lateral and posteroanterior cephalometric radiographs and occlusal variables and evaluated temporomandibular joint symptoms. Statistical comparisons were performed between the 2 groups ( P <0.05).
Results
The posteroanterior cephalometry significantly differed between the ipsilateral and contralateral groups. Occlusal force and occlusal contact area were significantly larger, and temporomandibular joint symptoms were more frequently found on the side of the upward-inclined frontal occlusal plane than on the opposite side in both groups.
Conclusions
The features in the contralateral group in terms of occlusal force and temporomandibular disorders were clinically significant. Clinicians should note that the conditions associated with the contralateral group require less presurgical decompensation.
Highlights
- •
Frontal occlusal plane inclination and mandibular deviation were studied.
- •
The maxillary bone was inclined toward the contralateral side.
- •
Dental compensation in the mandibular molars was less.
- •
Occlusal force and contact area were larger contralateral to the deviation.
- •
Clicking was less prevalent ipsilateral to the deviation, more prevalent contralateral.
Orthognathic surgery is an effective method to achieve good occlusion and improve skeletal morphology and facial appearance in subjects with facial deformity and disharmony between the maxilla and the mandible.
Esthetic demands include improvements in the horizontal and vertical dimensions of the maxilla and the mandible that alter the facial profile and the frontal aspect for facial asymmetry (FA); this is an important treatment goal for orthognathic surgery. However, it is difficult to estimate FA accurately before treatment because it requires bilateral evaluations by both the patient and the operator. Many morphologic studies have evaluated skeletal and soft tissue characteristics in the lateral and frontal aspects using cephalometry for diagnosis and treatment planning. Three-dimensional computed tomography is commonly used for diagnosis.
Many studies have shown that subjects with FA have morphologic problems and functional disorders in the oral and facial areas, such as occlusal force and temporomandibular disorders (TMDs). Occlusal force is lower in subjects with FA than in normal subjects. Moreover, the occlusal force and the occlusal contact areas of the ipsilateral side to the mandibular deviation are significantly greater than those of the contralateral side in patients with FA. Furthermore, the prevalence of TMDs is higher in patients with FA and is more frequent in the ipsilateral side. Therefore, we assumed that functional aspects such as occlusal force and TMDs are related to 3-dimensional morphologic disharmonies of the maxilla and the mandible in the sagittal and frontal planes.
Most clinical studies of FA have focused on the mandibular deviation, and some have described a relationship between mandibular lateral deviation and the inclination of the frontal occlusal plane (FOP) of the maxilla. There is a strong correlation between mandibular lateral deviation and canting of the maxillary FOP, which tends to incline toward the ipsilateral side of the mandibular deviation ; however, we have previously reported on patients with FA whose FOPs inclined toward the contralateral side.
The aim of this study was to investigate the morphologic and functional features of subjects with the FOP inclined toward the contralateral side of the mandibular deviation. We tested the null hypothesis that there would be no significant difference in morphologic and functional features between the patients with the FOP inclined toward the ipsilateral and contralateral sides of the mandibular deviation except for the dentoalveolar measurements.
Material and methods
We examined patient records from April 2006 to December 2012 at the orthodontic department of Tokyo Medical and Dental University; 272 (67.2%) of 405 patients with mandibular protrusion (ANB angle ≤0.0°) were found to have prominent FA, defined as a deviation of 2.0 mm or more of menton to the cranial midline on a posteroanterior (PA) cephalometric radiograph. We found that 206 of the 272 patients (75.7%) had the FOP inclined toward the ipsilateral side of the mandibular deviation. Only 20 of the 272 patients (7.4%) had the FOP inclined toward the contralateral side. No inclination of the FOP was seen in the remaining 46 patients (16.9%), since they did not meet our definition of FOP with an absolute value of 1.0° or more. Positive and negative values indicate that the FOP is inclined toward either the ipsilateral or the contralateral side of the mandibular deviation, respectively.
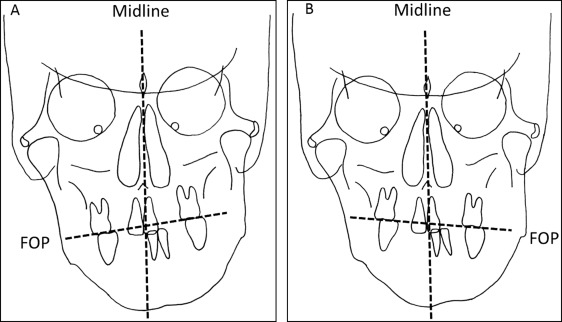
We randomly selected 20 patients (11 men, 9 women), aged 24.7 ± 4.2 years (mean ± SD), from the 206 patients in whom the FOP was inclined toward the ipsilateral side of the mandibular deviation ( Fig 1 , A ). This was called the ipsilateral group. Another 20 patients (11 men, 9 women), aged 25.5 ± 3.8 years, whose FOPs inclined toward the contralateral side of the mandibular deviation ( Fig 1 , B ), were referred to as the contralateral group.
The subjects met the following criteria: (1) no previous orthodontic treatment, (2) no clinical history of lateral functional mandibular shifts on closure, and (3) no congenital anomaly. We (1) performed lateral cephalometry, (2) performed PA cephalometry, (3) measured the occlusal force and occlusal area, and (4) evaluated TMDs.
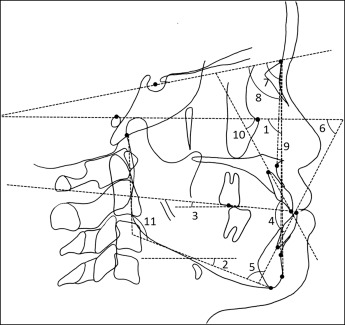
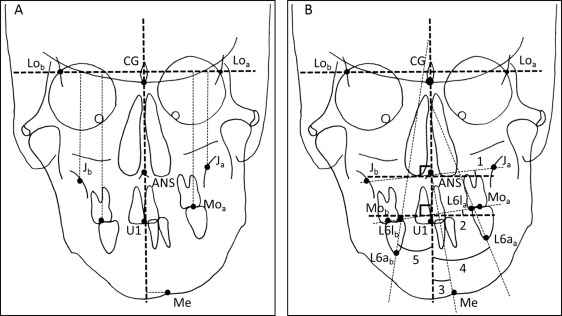
We performed lateral cephalometry with the landmarks and measurements ( Fig 2 ) to delineate the skeletal features of both groups in the sagittal dimensions. Likewise, we performed PA cephalometry with the landmarks and measurements ( Fig 3 ) described previously to investigate the skeletal features in the frontal dimension.
The occlusal force, occlusal contact area, and occlusal average pressure were recorded by pressure-sensitive sheets (Dental prescale 50H R-type; GC, Tokyo, Japan). The sheets included a layer of microcapsules that contain a color-forming material and a layer of a color-developing material. The microcapsules in the sheets are various sizes and strengths, and are broken with pressure. We analyzed the sheets with a computer (Occluzer PD-703; GC).
We calculated the asymmetry index ( Table I ) to investigate the relationship among the FOP, the amount of mandibular deviation, and the balance of the occlusal force between both sides. We also examined the correlation between the asymmetry index and the FOP, and the amount of mandibular deviation.
| Variable | Formula |
|---|---|
| Occlusal force (OF) (N) | |
| OF ipsi | Sum of OF on the ipsilateral side of the mandibular deviation |
| OF contra | Sum of OF on the contralateral side of the mandibular deviation |
| OF total | Sum of OF ipsi and OF contra |
| Occlusal contact area (OCA) (mm 2 ) | |
| OCA ipsi | Sum of OCA on the ipsilateral side of the mandibular deviation |
| OCA contra | Sum of OCA on the contralateral side of the mandibular deviation |
| OCA total | Sum of OCA ipsi and OCA contra |
| Occlusal average pressure (OAP) (MPa) | |
| OAP ipsi | Average OAP on the ipsilateral side of the mandibular deviation |
| OAP contra | Average OAP on the contralateral side of the mandibular deviation |
| OAP total | Average of OAP ipsi and OAP contra |
| Asymmetry index of OF (%) | (OF ipsi -OF contra ) × 100/(OF ips + OF contra ) |
| Asymmetry index of OCA (%) | (OCA ipsi -OCA contra ) × 100/(OCA ipsi + OCA contra ) |
We calculated the ratio of patients with TMDs in each group ( Table II ) to investigate the relationship between the inclination of the FOP and TMD.
| Symptom | Description |
|---|---|
| TMD | Click or tenderness |
| Click ipsi | Clicking on the ipsilateral side of the mandibular deviation |
| Click contra | Clicking on the contralateral side of the mandibular deviation |
| Click bi | Clicking on the bilateral sides |
| Tenderness | Tenderness of the TMJ, temporalis, masseter, and sternocleidomastoid muscles on palpation |
| Pain on motion | Feeling of pain on opening the mouth |
| Restriction | Restriction of mouth opening |
| Tiredness | Tired feeling of the TMJ, temporalis, masseter, and sternocleidomastoid muscles on palpation |
Statistical analysis
The Student t test was used to test for differences in the cephalometric measurements and to compare occlusal force between the ipsilateral and contralateral groups. The paired t test was used to compare bilateral occlusal force, occlusal contact area, and occlusal average pressure between the ipsilateral and contralateral sides of the mandibular deviation in each group. We also explored the correlations between the asymmetry index, the FOP, and the amount of mandibular deviation. The Fisher exact test was used to compare the frequencies of TMDs between the groups. All analyses were performed with the Statistical Package for the Social Sciences (version 10.0; SPSS, Chicago, Ill). Significance was defined as P <0.05.
Results
The same operator (S.U.) analyzed all lateral and PA cephalometric radiographs. We randomly chose a cephalometric radiograph and performed duplicate measures of each parameter. We then evaluated intraoperator error using the Dahlberg formula and found no significant ( P <0.05) intraoperator error (linear measurements, 0.12-0.18 mm; angular measurements, 0.10°-0.25°).
There were no significant differences in lateral cephalometry between the ipsilateral and contralateral groups ( Table III ). The PA cephalometry showed significant differences in several variables between the groups ( Table IV ). The values of midline-U1, ∠J, ∠Ocl, and incL6 a were significantly smaller, and the values of Lo line-J diff, Lo line-Mo diff, and incL6 b were significantly greater in the contralateral than in the ipsilateral group (see Fig 3 for definitions). There were no other significant differences between the groups.
| Measurement (°) | Ipsilateral group | Contralateral group | P value | ||
|---|---|---|---|---|---|
| Mean | SD | Mean | SD | ||
| Facial angle | 90.86 | 4.08 | 91.34 | 4.43 | 0.75 |
| Mandibular plane | 26.69 | 7.08 | 27.62 | 6.71 | 0.71 |
| Occlusal plane | 9.05 | 4.58 | 8.51 | 5.71 | 0.77 |
| Interincisal | 129.62 | 12.02 | 127.73 | 10.79 | 0.64 |
| L1-mandibular | 86.94 | 7.59 | 85.89 | 6.92 | 0.69 |
| FMIA | 67.18 | 7.66 | 66.45 | 8.92 | 0.80 |
| SNA | 80.55 | 3.32 | 79.57 | 3.07 | 0.39 |
| SNB | 84.71 | 5.32 | 82.98 | 4.46 | 0.32 |
| ANB | −3.56 | 2.73 | −3.39 | 2.88 | 0.87 |
| U1-FH plane | 118.42 | 6.37 | 117.22 | 6.25 | 0.59 |
| Gonial angle | 125.11 | 6.02 | 127.11 | 7.81 | 0.41 |
| Ipsilateral group | Contralateral group | P value | Significance | |||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | |||
| Lo line-J a (mm) | 60.89 | 2.40 | 60.94 | 4.39 | 0.97 | |
| Lo line-J b (mm) | 61.74 | 2.62 | 60.31 | 4.31 | 0.26 | |
| Lo line-J diff (mm) | −0.84 | 0.83 | 0.63 | 1.82 | 0.02 | ∗ |
| Lo line-Mo a (mm) | 83.68 | 4.00 | 87.38 | 5.26 | 0.12 | |
| Lo line-Mo b (mm) | 85.79 | 4.05 | 85.31 | 5.33 | 0.77 | |
| Lo line-Mo diff (mm) | −2.11 | 1.45 | 2.06 | 0.68 | 0.00 | ∗ |
| Midline-U1 (mm) | 0.38 | 0.77 | −0.53 | 1.12 | 0.01 | ∗ |
| Midline-Me (mm) | 5.71 | 3.08 | 3.88 | 1.86 | 0.08 | |
| ∠MeA (°) | 2.97 | 1.42 | 1.88 | 0.83 | 0.12 | |
| ∠Fmp (°) | 1.68 | 3.15 | 1.23 | 2.24 | 0.45 | |
| ∠J (°) | 1.20 | 1.44 | −1.12 | 1.71 | 0.00 | ∗ |
| ∠Ocl (°) | 2.45 | 1.24 | −2.05 | 0.98 | 0.00 | ∗ |
| incL6 a (°) | 31.25 | 5.95 | 26.86 | 6.29 | 0.03 | ∗ |
| incL6 b (°) | 20.92 | 4.85 | 25.50 | 6.61 | 0.02 | ∗ |
In the ipsilateral group, occlusal force and occlusal contact area were significantly larger on the ipsilateral side of the mandibular deviation than on the contralateral side ( Table V ). No significant difference was found in occlusal average pressure between sides. In contrast, occlusal force and occlusal contact area were significantly larger on the contralateral side of the mandibular deviation than on the ipsilateral side in the contralateral group ( Table VI ). No significant difference in occlusal average pressure was found between sides in the ipsilateral group.
| Ipsilateral | Contralateral | P value | Significance | |||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | |||
| OF (N) | 299.97 | 22.91 | 231.43 | 15.23 | 0.00 | ∗ |
| OCA (mm 2 ) | 6.86 | 0.77 | 4.92 | 0.45 | 0.02 | ∗ |
| OAP (MPa) | 48.03 | 13.89 | 49.57 | 10.69 | 0.52 | NS |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


