Key points
- •
The natural evolution of the extraction socket is one of bone loss, most significantly affecting the buccal-lingual dimension.
- •
The healing socket regenerates through intramembranous ossification. The newly developed bone undergoes remodeling and responds to mechanical stress (modeling). The load created by a dental implant leads to long-term modeling of the bone.
- •
Allograft, xenograft, or alloplast grafts are static, inert materials often found unresorbed in graft sites. Residual graft particles that do not resorb can interfere with stress- and strain-induced bone modeling.
- •
Bone morphogenetic protein-2 (BMP-2) is a cytokine member of the transforming growth factor β superfamily that stimulates de novo bone formation. Recombinant human BMP-2 (rhBMP-2) (1.5 mg/mL) delivered via an acellular collagen sponge (ACS) is a versatile graft that can be used alone, in conjunction with mineralized cancellous particles, and with simultaneous implant placement.
- •
Implants placed in extraction sockets act as a construct to enhance bone regeneration. In the author’s experience, implants placed in sockets with wall defects and grafting with rhBMP-2/ACS have shown excellent integration and buccal wall regeneration.
- •
When implant placement is not feasible, socket preservation screws can be used to support gingiva and regenerate alveolar form while maintaining biologic width.
Introduction
The long-term success and health of a dental implant relies on a viable osseous environment. Damage to a socket can occur from infection, trauma, malpositioned teeth, or traumatic extraction, leading to an unsuitable site for implant replacement. The buccal wall is particularly important and its loss can lead to unesthetic gingival discoloration, peri-implantitis, thread exposure, and implant failure. Even in ideal situations, the normal healing process of an extraction socket is one of regressive remodeling. This process occurs from not only remodeling within the socket but also pressure from soft tissue contraction affecting the buccal wall of the alveolus. As a result, bone loss occurs more in the buccal-lingual dimension, and most significantly over the first several months. In a systematic review, Tan and colleagues reported 29% to 63% horizontal bone loss and 11% to 22% vertical bone loss 6 months after tooth extraction.
The process of socket healing has been investigated histologically and consists of a sequence that resembles intramembranous bone formation. A clot composed of erythrocytes trapped in a fibrin network is formed and stabilized immediately after extraction and over the first several days. By the seventh day, granulation tissue, or highly vascularized tissue with inflammatory infiltrate, is formed near the crestal area and the rest of the socket is filled with a provisional matrix consisting of immature mesenchymal cells, various types of leukocytes, and collagen fibers. At the end of first month, the matrix transitions to woven bone, and closure of the socket occurs with a fibrous connective layer containing keratinized epithelium. Finally, the immature bone remodels into mature lamellar bone by 2 months. This remodeling process is characterized by a balanced interplay between osteoclastic resorption and osteoblastic formation. It continues indefinitely and is particularly rigorous in the alveolus, an area of high bony turnover.
Another important adaptive feature of bone is termed modeling , in which bone changes its size and shape in response to the presence and absence of external mechanical forces. A dental implant under load initiates mechanotransduction pathways, specifically at the bone–implant interface. Long-term maintenance of implants involves continuous remodeling of the interface to maintain bone or replace bone that has sustained microfractures or fatigue from cyclic loading. Finite elemental analysis of an osseointegrated dental implant have shown that von Mises forces are focused at the crest for angled implants (such as those in the anterior maxilla) and more evenly distributed around the implant in axially loaded implants (such as those in the posterior maxilla and mandible). Thus, anterior maxillary implants are at risk of bone loss from focused forces, and thin bone if the bone is not capable of remodeling and modeling. Long-term implant survival relies on viable bone that provides a dynamic and adaptive osseous environment.
Socket grafting has become an accepted modality of preserving alveolar ridge dimensions after tooth extraction. Different techniques using various materials have been described. Autogenous grafting requires a second donor site with added morbidity. Bone substitutes (allograft, xenograft, alloplast) act as a scaffold for bone formation, but histomorphometric analysis shows that the grafted site is composed of vital bone intertwined with as much as 40% of unresorbed grafting material.
Advances in tissue engineering have enabled the reconstruction of natural form and function of missing tissues and organs. Bone morphogenetic proteins (BMPs) are members of the transforming growth factor β superfamily that are key regulators of cellular growth and differentiation. Specifically, BMP-2 has been shown to be chemotactic, and it upregulates vascular endothelial growth factor α activity and directs mesenchymal stem cells to differentiate into osteoblasts.
The INFUSE bone graft (Medtronic, Memphis Tennessee) consists of genetically engineered human BMP-2, manufactured with recombinant technology. It is delivered via an absorbable collagen sponge that helps initiate clot formation and ultimately resorbs. It has been shown to induce de novo bone formation ( Fig. 1 ) and is approved by the US Food and Drug Administration for alveolar ridge augmentation for defects associated with extraction sockets.
-
Indications
- •
Defects associated with extraction sockets.
-
Contraindications (obtained from INFUSE package insert )
- •
Hypersensitivity to recombinant human BMP-2 (rhBMP-2)/acellular collagen sponge (ACS)
- •
Vicinity of a resected or extant tumor
- •
Presence of any active malignancy or current treatment for a malignancy
- •
Acute, active infection not localized to the operative site
- •
rhBMP-2/ACS has not been studied in an Investigational Device Exemption (IDE) trial for pediatric and pregnant patients
-
Preoperative planning
- •
Bone defects can be visualized with cone beam computed tomography (CT), but it is more often a clinical determination.
- •
An XXS kit of rhBMP-2/ACS is typically sufficient to graft a socket and can be mixed with mineralized cancellous particles for added construct surface area and improved space maintenance.
- •
Implants can be placed immediately with rhBMP-2/ACS with good results.
-
Case reports
-
See Figs. 2–8 .
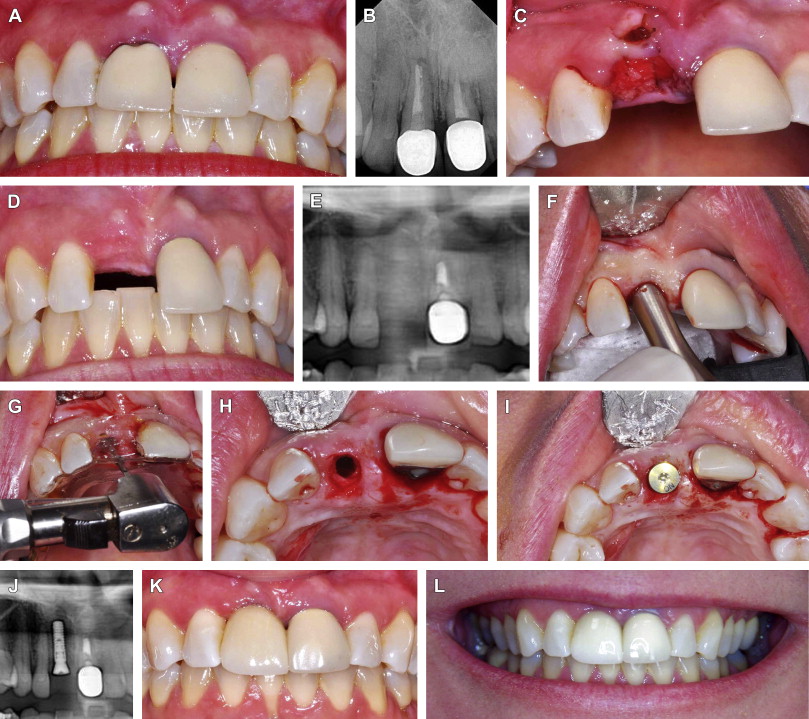
Fig. 2 Esthetic case involving extraction of tooth #8, socket grafting with rhBMP-2/ACS with mineralized cancellous particles, and implant placement at second stage. ( A ) Tooth #8 with chronic abscess after trauma with ( B ) periapical radiolucency. ( C ) Tooth #8 extracted and rhBMP-2/ACS with mineralized cancellous particles are placed into socket. ( D ) Alveolar ridge 4 weeks after extraction with homogenous bone fill ( E ) on panoramic radiograph. ( F ) Flapless surgical approach. Note excellent gingival architecture. ( G ) Use of surgical guide assists in appropriate placement. ( H ) Implant osteotomy into bleeding, viable bone. ( I ) Placement of implant with healing abutment. ( J ) Panoramic radiograph confirms implant in good position with surround bone. ( K ) Day of restoration. ( L ) Two years later with good esthetic result. Tooth #9 pending extraction.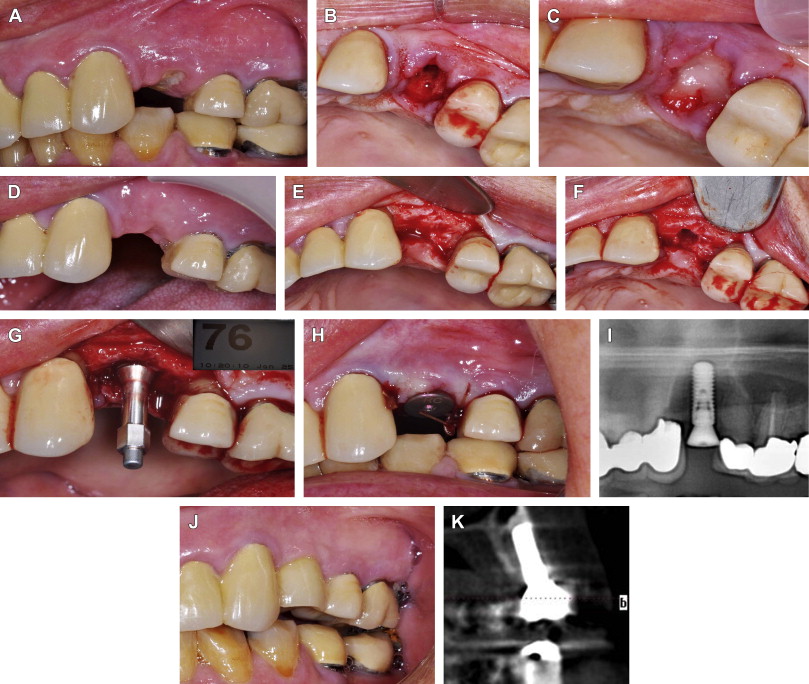
Fig. 3 Extraction of tooth #12, socket grafting and buccal wall regeneration with rhBMP-2/ACS alone, and implant placement at a second stage. ( A ) Fractured and nonrestorable tooth #12. ( B ) Extraction of tooth reveals buccal wall defect. Osteotomy on palatal bone to stimulate bleeding. ( C ) Graft with XXS kit of rhBMP-2/ACS alone. ( D ) Four months later at time of implant placement, site shows healthy soft tissue with preservation of papilla. ( E ) Surgical exposure reveals regeneration of buccal wall and ( F ) vascular bone at osteotomy site. ( G ) Implant is placed with good initial stability (Implant Stability Quotient [ISQ] value 76). ( H ) Healing abutment is placed to optimize gingival contours and papilla preservation. ( I ) Panoramic radiograph shows good position of implant. ( J ) At 8 weeks, final restoration and CT scan ( K ) shows radiographic evidence of implant osseointegration into native, viable bone.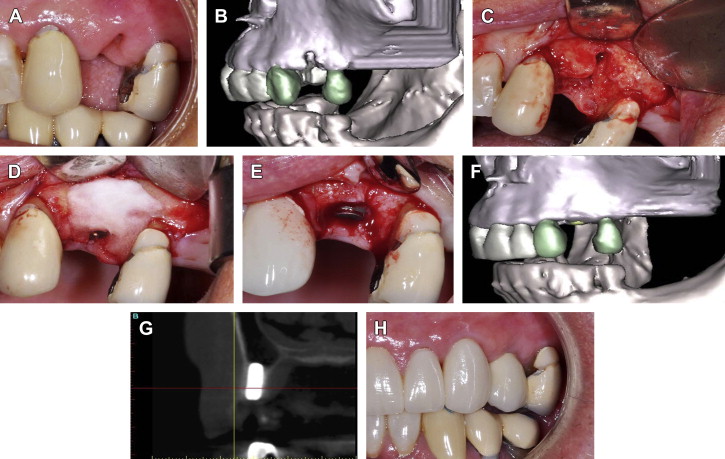
Fig. 4 Extraction of tooth #12, socket grafting and buccal wall regeneration with rhBMP-2/ACS, and immediate implant placement. This patient participated in a prospective pilot study of 6 patients that followed the same protocol detailed in Fiorellini and colleagues, with the only variable being implant placement in conjunction with rhBMP-2/ACS. ( A ) Extraction socket with radiographic evidence of buccal wall defect on ( B ) 3-dimensional reconstruction of cone beam CT. ( C ) Surgical exposure reveals buccal wall defect. ( D ) Implant placed and rhBMP-2/ACS alone placed on buccal aspect. ( E ) 6 months later at implant uncovering, buccal wall regeneration is evident clinically and ( F , G ) radiographically. ( H ) Final restoration at 6 months as per the study protocol.( Data from Fiorellini JP, Howell TH, Cochran D, et al. Randomized study evaluating recombinant human bone morphogenetic protein-2 for extraction socket augmentation. J Periodontol 2005;76:605.)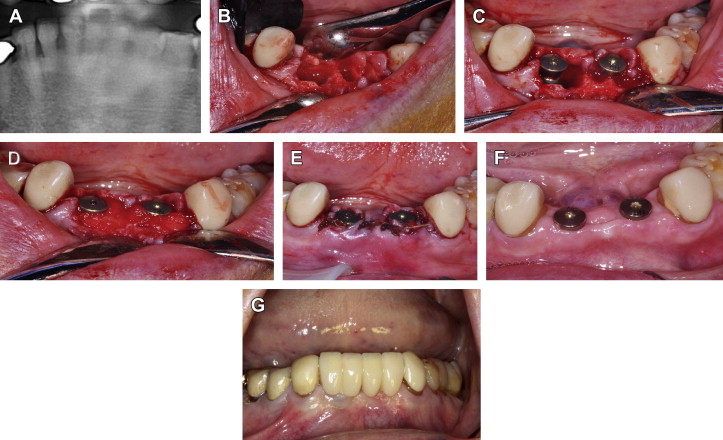
Fig. 5 Extraction of teeth #23, #24, #25, and #26; immediate implant placement; and grafting of socket defects with rhBMP-2/ACS and mineralized cancellous particles. ( A ) Panoramic radiograph reveals periodontal bone loss on lower anterior teeth. ( B ) Surgical exposure and teeth extraction reveal thin buccal bone with vertical loss. ( C ) Immediate implant placement in locations 23 and 26 and ( D ) grafting with rhBMP-2/ACS with mineralized cancellous particles. ( E ) Closure of soft tissue around healing abutments. ( F ) Twelve weeks after surgery excellent soft tissue healing is seen. ( G ) Three-year follow-up.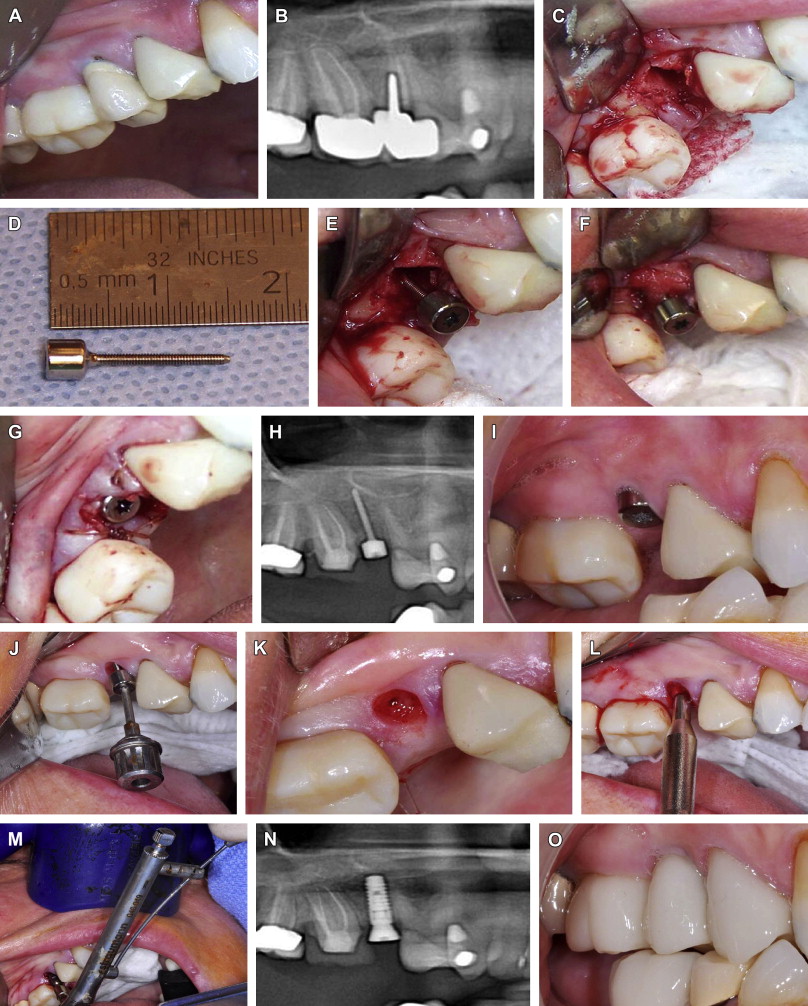
Fig. 6 Extraction of tooth #5, placement of socket preservation screw with rhBMP-2/ACS only and implant placement at a second stage. ( A ) Failing tooth #4 deemed nonrestorable and not a suitable site for immediate implant placement because of ( B ) distal angulation of tooth #5 seen on panoramic radiograph. ( C ) Extraction socket. ( D ) Socket preservation screw with 1.2-mm threaded body and 3 × 3–mm polished head. ( E ) Screw partially placed into extraction socket after implant osteotomy with twist drill. ( F ) Placement of rhBMP-2/ACS alone around screw and into socket. Head is then screwed to final depth, with base of screw placed at crestal bone height. ( G ) Closure of soft tissues around screw head, which acts like a healing abutment. ( H ) Panoramic radiograph shows good position of screw. ( I ) Five months later, gingival architecture and papilla are preserved. ( J ) Screw is removed. ( K ) Development of gingival biologic width in conjunction with socket bone regeneration. ( L ) Implant osteotome placed into screw hole. ( M ) Implant placement with torque greater than 25 Newton centimeters. ( N ) Panoramic radiograph shows implant placement in regenerated socket. ( O ) Final restoration at 2-year follow-up.Fig. 7 Extraction of teeth #3, #4, #5, #6, #7, and #8; socket grafting and reconstruction of multiple bony defects with a trilayer graft, including rhBMP-2/ACS, mineralized cancellous particles, and C-graft; and simultaneous implant placement. C-graft is derived from red sea algae and processed to develop a hydroxyapatite/tricalcium phosphate resorbable material. ( A , B ) Multiple failing crowns from recurrent caries and periodontal disease. ( C ) Surgical exposure and extractions reveal multiple bony defects. Site #3 not suitable for implant placement. ( D ) Implants placed in sites 4, 6, 8 with rhBMP-2/ACS alone placed on implant surface. The space is filled with rhBMP-2/ACS and mineralized cancellous particles, and the outer wall is created by C-graft. ( E ) Strips of rhBMP-2/ACS laid on buccal aspect of graft. ( F ) Tension-free closure is obtained with chromic gut in a horizontal mattress fashion followed by oversewing with MONOCRYL in a running fashion. ( G ) Panoramic radiograph shows implant placement. ( H , I ) At 4 months, another implant is placed in site #3, and stage 2 uncovering of other implants is performed. ( J ) Final restoration at 6 months.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


