Angle, Tweed, and Moyers classified Class III malocclusions into 3 types: pseudo, dentoalveolar, and skeletal. Clinicians have been trying to identify the best timing to intercept a Class III malocclusion that develops as early as the deciduous dentition. With microimplants as skeletal anchorage, orthopedic growth modification became more effective, and it also increased the scope of camouflage orthodontic treatment for patients who were not eligible for orthognathic surgery. However, orthodontic treatment combined with orthognathic surgery remains the only option for patients with a severe skeletal Class III malocclusion or a craniofacial anomaly. Distraction osteogenesis can now be performed intraorally at an earlier age. The surgery-first approach can minimize the length of time that the malocclusion needs to worsen before orthognathic surgery. Finally, the use of computed tomography scans for 3-dimensional diagnosis and treatment planning together with advances in imaging technology can improve the accuracy of surgical movements and the esthetic outcomes for these patients.
Highlights
- •
We studied the best timing to intercept a developing Class III malocclusion.
- •
Camouflage is possible with microimplants for skeletal anchorage.
- •
Improvements in technology will help in the diagnosis and treatment of Class III patients.


In 1899, Angle was the first to classify malocclusions into Class I, Class II, and Class III based on the relationship of the first molars and the alignment (or lack of it) of the teeth relative to the line of occlusion. Almost immediately, it was recognized that the Angle classification was not complete because it did not include important characteristics of the patient’s problem. Gradually, Angle’s classification numbers were extended to refer to the skeletal jaw relationship and the pattern of growth other than the molar relationship. Thus, a Class III jaw relationship meant that the mandible was positioned mesial to the maxilla. This was usually found in connection with a Class III molar relationship but occasionally could be a Class I molar relationship when the dental compensation overcame the skeletal imbalance. A Class III growth pattern is then defined as one with disproportionate forward mandibular growth or deficient maxillary growth.
In 1966, Tweed classified Class III malocclusions into 2 categories: category A was defined as a pseudo-Class III malocclusion with a conventionally shaped mandible, and category B was defined as a skeletal Class III malocclusion with a large mandible or an underdeveloped maxilla. Moyers further classified malocclusions according to the cause of the problem: osseous, muscular, or dental in origin. Moyers emphasized the need to determine whether the mandible, on closure, is in centric relation or in a convenient “anterior” position for patients with neuromuscular or functional problems. Anterior repositioning generally results from a tooth contact relationship that forces the mandible in a forward position. Moyers suggested that a pseudo-Class III malocclusion is a positional malrelationship with an acquired neuromuscular reflex.
The prevalence of Angle Class III malocclusions varies greatly among and within populations, ranging from 0% to 26%. Pseudo-Class III malocclusions are found primarily in the deciduous and mixed dentitions. Approximately 60% to 70% of anterior crossbites in the 8- to 12-year-old group were classified as pseudo-Class III malocclusions. A study excluding children under 11 years old found that the populations from Southeast Asian countries (Chinese and Malaysian) showed the highest prevalence rate of 15.8%. Middle Eastern nations had a mean prevalence rate of 10.2%. European countries had a lower prevalence rate of 4.9%, and the Indian population showed the lowest prevalence rate of 1.2%. In white children, approximately 57% of the patients with either a normal or a prognathic mandible showed a deficiency in the maxilla. In Asian countries such as Japan, patients were found to have a significantly reduced anterior cranial base, an obtuse gonial angle, and an increased lower anterior face height. Backward rotation of the mandible was necessary to coordinate the occlusion because of the small maxilla.
Evolution of orthopedic treatment
In 1728, Fauchard was first to describe the bandeau, an expansion arch consisting of a horseshoe-shaped strip of precious metal to which the teeth were ligated. It was refined by Bourdet, a dentist to the King of France; he was the first to practice “lingual orthodontics,” expanding the arch from the lingual aspect. In 1771, Hunter took a particular interest in the anatomy of the teeth and jaws. His text, The Natural History of the Human Teeth , presented the first clear statement of orthopedic principles. He established the difference between teeth and bone, and he gave the teeth names such as cuspidati and bicuspidati. He was the first to describe the growth of the jaws, not as a hypothesis but as a sound, scientific investigation.
In 1802, Fox was the first to give explicit directions for correcting irregularities of the teeth. He was particularly interested in the use of an expansion arch and a chincup. However, it was Kneisel, a German dentist to Prince Charles of Prussia, who was the first to use a removable chin strap to treat patients with a prognathic mandible.
For maxillary orthopedics, Angell was first to open the median palatal suture with a split plate. Case showed remarkable foresight in differentiating between “dental malpositions” and “dentofacial imperfections,” comparable to today’s terms, dentoalveolar and skeletal. He stressed facial esthetics in contrast to Angle’s reliance on occlusion. He said, “The occlusion or malocclusion of the buccal teeth gives no indication of the real position of the dentures in relation to facial outlines.”
Etiology of Class III malocclusion
Class III malocclusion can be a result of pure mandibular prognathism or maxillary hypoplasia and retrognathism, or a combination of the two. That means that there is possible anatomic heterogeneity of this type of malocclusion, since either jaw or both jaws can be affected in sagittal length or in position relative to the other. Familial aggregation studies also suggest that familial environmental factors or heredity can play a substantial role in the etiology of Class III malocclusion.
Environmental factors that have been thought to influence Class III malocclusion include habits, enlarged tonsils, chronic mouth breathing leading to downward and backward growth of mandible, abnormal tongue and mandibular posture, endocrine disturbances, posture, trauma, and nasal blockage. The role of these factors, however, is based on only a few observations.
The familial nature of mandibular prognathism was first reported by Strohmayer in 1937 as noted by Wolff et al in their analysis of the Hapsburg family. However, it is probable that the mandibular prognathism in the Hapsburg family was heavily influenced by inbreeding, an autosomal recessive pattern, and other multifactorial inheritance possibilities. Analyses of less inbred groups usually indicate an autosomal dominant mode of inheritance with incomplete penetrance and variable expressivity in some families and multifactorial influences in others.
Etiology of Class III malocclusion
Class III malocclusion can be a result of pure mandibular prognathism or maxillary hypoplasia and retrognathism, or a combination of the two. That means that there is possible anatomic heterogeneity of this type of malocclusion, since either jaw or both jaws can be affected in sagittal length or in position relative to the other. Familial aggregation studies also suggest that familial environmental factors or heredity can play a substantial role in the etiology of Class III malocclusion.
Environmental factors that have been thought to influence Class III malocclusion include habits, enlarged tonsils, chronic mouth breathing leading to downward and backward growth of mandible, abnormal tongue and mandibular posture, endocrine disturbances, posture, trauma, and nasal blockage. The role of these factors, however, is based on only a few observations.
The familial nature of mandibular prognathism was first reported by Strohmayer in 1937 as noted by Wolff et al in their analysis of the Hapsburg family. However, it is probable that the mandibular prognathism in the Hapsburg family was heavily influenced by inbreeding, an autosomal recessive pattern, and other multifactorial inheritance possibilities. Analyses of less inbred groups usually indicate an autosomal dominant mode of inheritance with incomplete penetrance and variable expressivity in some families and multifactorial influences in others.
Treatment of pseudo-Class III malocclusion
A pseudo-Class III malocclusion is characterized by an anterior crossbite caused by a forward functional displacement of the mandible. In the mixed dentition, the patient usually has a mesial step that is less than 3 mm. The maxillary incisors are retroclined, and the mandibular incisors are proclined and spaced. When patients are guided into a centric relationship, they often show an end-to-end incisor relationship accompanied by a forward shift of the mandible that we now call a functional Class III malocclusion. In most patients, it is caused by retroclination of the maxillary incisors. Often, there is a Class I molar relationship with a normal mandibular appearance and a straight facial profile, disguising the skeletal discrepancy.
An anterior crossbite and a mild skeletal Class III malocclusion in the mixed dentition can be corrected with a variety of treatment approaches, including removable appliances, partial fixed appliances, orthopedic chincup, and facemask for a short duration. Correction of the anterior crossbite should be carried out as soon as it is detected to maximize the orthopedic effects and the stability of early treatment. Correcting an anterior crossbite increases the maxillary arch perimeter, offering more space for the eruption of the canines and the premolars. Anterior crossbites left untreated have been associated with a variety of complications, such as gingival recession of the mandibular incisors, incisal wear, and worsening of the growth pattern.
Removable functional appliances such as Fränkel III regulators and activators to treat Class III malocclusions work by permitting the eruption of the maxillary molars and maintaining the mandibular ones in position, leading to an occlusal plane rotation that helps to shift the molar relationship from Class III to Class I. On the other hand, maxillary protraction using a facemask creates a counterclockwise rotation of the maxilla and a clockwise rotation of the mandible, usually resulting in increased lower face height. Therefore, these appliances are more suitable to be used in functional Class III patients with lower angles.
In young patients with an anterior crossbite, better results can be achieved through the association of maxillary expansion because of orthopedic stability and the movement of the maxilla down and forward. In 84% of patients, self-correction can be expected without the need for any other appliance. The association of maxillary expansion and 2 × 4 fixed appliances improves the arch perimeter, reducing the number of extractions in patients with slight to mild crowding. The increase has been quantified to span up to 6.0 mm in the maxillary arch. Other advantages of fixed appliances include better 3-dimensional (3D) control of tooth movement and the use of light continuous forces.
Treatment of skeletal Class III malocclusion with a chincup
In 1836, Kneisel, a German dentist to Prince Charles of Prussia, was the first to use a removable chin strap to treat patients with a prognathic mandible. This was followed by Westcott, who also reported the use of occipital anchorage to correct mandibular protrusion. After a long period of disuse of the vertical chincup, Oppenheim reintroduced extraoral anchorage in 1944.
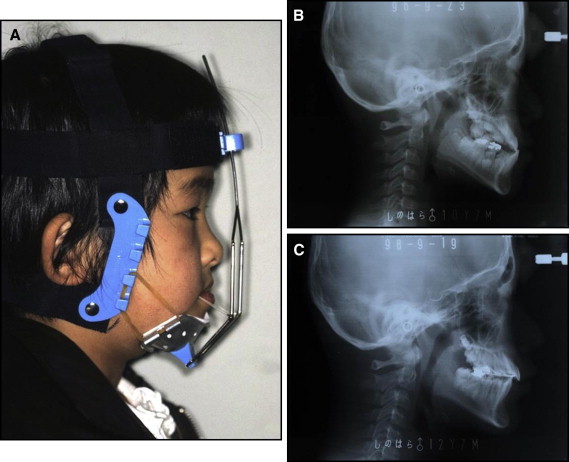
The chincup, or chincap, was widely used in the Southeast Asian countries because of the prevalence of Class III patients with mandibular prognathism and downward and backward growth directions. Sugawara et al and Mitani et al reported that chincap forces can alter the mandibular form and condylar growth. Deguchi et al reported that aggressive application of a chincup or reverse-pull headgear for 2 years resulted in effective orthopedic treatment, and skeletal relapse diminished by 0% to 40% judging by the ramus angle, gonial angle, ANB, and Wits appraisal ( Fig 1 ). However, Sugawara and Mitani also admitted that although the mandibular position could be improved anteroposteriorly during the first 2 or 3 years of chincap therapy, the initial changes were not always maintained when chincap use was discontinued before facial growth was complete. Recovery growth may cause recurrence of the prognathic face and Class III malocclusion after discontinuation of chincap therapy. The author recommended that chincap use must be continued until the completion of facial growth. Chincap therapy is not indicated for patients with a true skeletal Class III malocclusion, a large mandible, a normal anteroposterior maxillary position, a mild anteroposterior skeletal discrepancy, a normal cranial base angle, a normal lower face height, and no temporomandibular joint disorder or indication for surgery.
Treatment of a skeletal Class III malocclusion with a protraction facemask
Until 1970, a Class III malocclusion was synonymous with mandibular prognathism. Many studies since then have found that in most patients, the hypoplastic maxilla is often the primary etiology of a Class III malocclusion. Dietrich reported maxillary retrusion in 40% of white children. Mandibular prognathism was due in part to positional deviation of the mandible relative to the cranial base. Maxillary retrusion was due primarily to inadequate length of the maxillary base. Guyer et al reported that 57% of white children with either a normal or a prognathic mandible showed a deficiency in the maxilla. On the other hand, Masaki found that patients with Asian origin have a significantly reduced anterior cranial base, an obtuse gonial angle, and an increased lower anterior face height. A backward rotation of the mandible was necessary to coordinate the occlusion because of a small maxilla.
In 1944, Oppenheim, a native of Moravia (now the Czech Republic), published the records of 3 Class III patients treated with a chincup and spurs, attached via elastics to a soldered maxillary lingual arch. Kettle and Burnapp from Guy’s Hospital in London, United Kingdom, also used a chincup with spurs to protract the maxilla in patients with cleft lip and palate. Most of us are familiar with the facemask of Delaire, which was a modification of the chincup that also incorporated a forehead support and an interlabial bow with spurs for attachment of elastics.
Haas reported that maxillary expansion alone often causes the maxilla to advance and drop vertically, rotating the mandible down and back. Using Class III elastics with palatal expansion, Haas demonstrated the correction of mild Class III malocclusions with this approach. In the 1970s, several primate studies contributed to our understanding of the anatomic effects of continuous protraction forces to the maxilla. These studies demonstrated not only significant maxillary skeletal and dental movements, but also orthopedic changes distant from the maxilla such as in the zygomaticotemporal articulation and the spheno-occipital synchondrosis.
In 1987, McNamara presented a case report and used a bonded expansion appliance in conjunction with a facemask to treat Class III patients with maxillary deficiency. This was followed by Turley, who presented a young patient with a Class III malocclusion corrected using palatal expansion and custom protraction headgear. Maxillary protraction has also been used in conjunction with an active chincup to produce a more efficient orthopedic treatment for Asian patients with combined maxillary deficiency and mandibular prognathism.
In the 1990s, several scientific studies clarified the effects of maxillary protraction on the correction of Class III malocclusions with maxillary deficiency. This involves forward movement of the maxilla, downward and backward rotation of the mandible, proclination of the maxillary incisors, and retroclination of the mandibular incisors. These studies also found that the amount of forward movement of the maxilla was limited to 2 to 4 mm, and this effect diminished in older patients. Liou proposed the use of an expansion-constriction protocol to achieve greater forward movement of the maxilla by distraction of the maxillary sutures. A recent study showed that maxillary expansion using the expansion-constriction protocol resulted in forward movement of the maxilla and a significant increase in upper airway volume.
Another shortcoming of using a tooth-borne appliance such as a rapid palatal expander for expansion and protraction is the loss of anchorage of the posterior molars and proclination of the maxillary incisors. Cevidanes et al introduced bone-anchored maxillary protraction, which induced a significantly greater maxillary advancement than did rapid palatal expansion in conjunction with facemask therapy. Mandibular sagittal changes are similar, whereas vertical changes are better controlled by bone-anchored maxillary protraction. Another favorable aspect of bone-anchored maxillary protraction is the lack of clockwise rotation of the mandible and retroclination of the mandibular incisors. Wilmes et al proposed the use of a hybrid hyrax expansion appliance with the expansion-constriction protocol to reduce the side effects of a conventional expansion appliance.
Several studies investigated the long-term effects in patients who underwent early Class III treatment. Westwood et al followed a sample of Italian children who underwent rapid palatal expansion with facemask treatment before the pubertal growth spurt (mean age, 8 years 3 months). At the final observation period (mean age, 14 years 10 months), there was a slightly greater increase in midfacial length (1.6 mm) in the treatment group than in the controls. The overall increase in mandibular length was 2.4 mm less in the rapid palatal expansion with a facemask group than in the controls, and mandibular projection relative to nasion perpendicular was 3.0 mm less in the treated group. The change in the Wits appraisal was 3.4 mm compared with −2.7 mm in the untreated controls. It appears that the favorable skeletal change observed over the long term is due almost entirely to the orthopedic correction achieved during the rapid palatal expansion with a facemask protocol. During the posttreatment period that includes the pubertal growth spurt, craniofacial growth in the patients in the rapid palatal expansion with a facemask group is similar to that of the untreated Class III controls. The authors recommended aggressive overcorrection of the Class III skeletal malocclusion, even toward a Class II occlusal relationship; this appears to be advisable, with the establishment of positive overbite and overjet relationships essential to the long-term stability of the treatment outcome.
Another study was carried out in a prospective clinical trial of 30 Chinese patients with Class III malocclusion and maxillary retrusion; they were treated with rapid palatal expansion with a facemask in the mixed dentition. Four years after removal of the appliances, 70% of these patients maintained a positive overjet. In an 8-year follow-up study, there were 9 dropouts from the original subjects. When the remaining subjects were divided into a stable group and a relapse group, 2 of 3 patients maintained a positive overjet 8 years after active treatment. The immediate treatment outcome in the sagittal plane was the same for both groups, but the lower face height increased and the mandibular plane opened more in the relapse group. Eight years after active treatment, dental compensation was similar in both groups, but the mandible outgrew the maxilla by 4 times in the relapse group, compared with 2 times in the stable group. These results indicate that in a Chinese population, of young patients diagnosed with a maxillary deficiency and treated with a facemask, there is a potential risk that a third of these patients may be candidates for orthognathic surgery later in life because of an unfavorable growth pattern.
For white children with Class III malocclusions, a retrospective study conducted at West Virginia University included 46 patients of North American origin who received early orthopedic-orthodontic treatment and comprehensive fixed appliance therapy. Lateral cephalograms were taken at the start of phase 1 of treatment (mean age, 8.6 ± 1.3 years) and at the end of fixed appliance therapy followed by a period of retention (mean age, 16.6 ± 2.8 years). The sample was divided into a stable group (26 patients) with positive overjet and an unstable group (20 patients) with end-to-end or negative overjet. No significant differences were found in the pretreatment craniofacial morphologies between the 2 starting groups. At the end of the observation period, the subjects in the unstable group had smaller Wits appraisal values and saddle angles (N-S-Ar), larger effective mandibular lengths (Co-Pg) and gonial angles (Ar-Go-Me), longer lower anterior facial heights, more anteriorly positioned mandibular molars relative to the maxillary molars, and more retroclined mandibular incisors. The results indicated that despite the lack of differences in craniofacial morphology at an early age, several craniofacial variables can be used over time to determine whether a white Class III patient will have a favorable or an unfavorable treatment outcome.
Where do we go from here?
A new breed of rapid palatal expanders incorporating microimplants—microimplant-assisted rapid palatal expanders—was born as implant orthodontics became popular. Numerous microimplant-assisted rapid palatal expanders were developed independently by investigators, varying in their designs and activation protocols. Carlson et al reported the expansion of surrounding structures including the zygoma when a particular type of microimplant-assisted rapid palatal expander, a maxillary skeletal expander, was used. When using a maxillary skeletal expander, disarticulation of the perimaxillary sutures was noted ( Fig 2 ). Combining maxillary protraction with maxillary skeletal expander was attempted by Moon, and the findings were reported in numerous international scientific meetings since 2008. When a maxillary skeletal expander was combined with maxillary protraction with a facemask, the following changes occurred: the magnitude of maxillary protraction was much greater than with the conventional approach, almost as much correction as normally achieved by surgical treatment; maxillary protraction for patients in the early teenage years was also possible; unwanted dentoalveolar changes such as proclination of the maxillary incisors were not apparent, and, in some patients, the dental compensations corrected themselves as the skeletal relationship improved; lateral tipping of the maxillary posterior dentition during maxillary expansion and anterior tipping of maxillary posterior dentition during maxillary protraction were minimal; and subsequently, clockwise rotation of the mandible was rarely observed even in high-angle patients. Others also reported varying degrees of success from combining various bone anchors and facemasks.
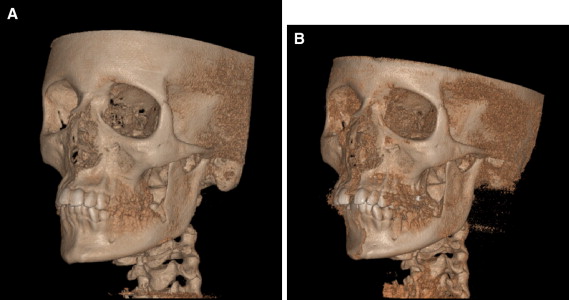
The maxillary skeletal expander disarticulates all perimaxillary sutures and impacts all structures surrounding the maxilla ( Fig 2 ). When a facemask is combined with it, the protraction force moves the maxilla in a distraction-like fashion. This may be why the magnitude and the speed of protraction exceed previously reported results with the conventional protraction approach. Wu et al suggested that adverse dental movements associated with tooth-borne devices are largely eliminated because the expansion and protraction with the maxillary skeletal expander is bone-borne. When skeletal balance was achieved by maxillary skeletal protraction, the maxillary dentition decompensated to a more normal position. This observation is supported by the functional matrix theory. Dental tipping during expansion and protraction is associated with clockwise rotation of the mandible, especially in high-angle patients. The maxillary skeletal expander and facemask combination can minimize such adverse effects and is recommended for high-angle patients.
De Clerck et al reported successfully treated Class III patients by placing maxillary and mandibular bone plates and using Class III elastics with an orthopedic force level. More favorable patient compliance compared with the facemask treatment approach can be expected. The dentoalveolar side effects were eliminated, as with the maxillary skeletal expander and facemask, and no deformations in the vertical dimensions were found, even though the force vector was more vertical. One disadvantage was the necessity for surgical placement and removal of the bone plates.
The natural progression of maxillary protraction will be combining the advantages of the novel protraction concepts. The maxillary skeletal expander and the facemask provide the most satisfactory results but require extremely dedicated patients who are willing to wear a facemask. Bone plates and elastic approaches require less patient cooperation, but surgeries are necessary. Developing nonsurgical skeletal anchorage for the mandible and applying orthopedic elastic force against the maxillary skeletal expander were proposed by Moon at the World Implant Orthodontic Conference in 2011 in Verona, Italy. Three in-vitro studies about developing self-drilling and self-tapping microimplants for orthopedic forces have been reported recently by Hong et al and Song et al, and the results were promising.
Camouflage Class III treatment in nongrowing Class III patients
Nongrowing patients with a skeletal Class III malocclusion are of great interest to practicing orthodontists. The choice between camouflage treatment and orthognathic surgery remains a challenge to the specialty. Class III patients who decline orthognathic surgery have been aggressively treated using multibrackets with Class III elastics, extractions, and multiloop edgewise archwire therapy.
Class III elastics or extraoral cervical anchorage (J-hook headgear) applied to the mandibular teeth can be used to retract the mandibular teeth and control the bite depth, but it requires patient cooperation. In addition, Class III elastics may inadvertently affect the inclination of the occlusal plane, the interincisal relationship, and the temporomandibular joint. These undesirable side effects can produce downward and backward rotation of the mandible, proclination of the maxillary incisors, and extrusion of the maxillary molars. These changes can lead to an unpleasing esthetic profile and instability during retention.
The multiloop edgewise archwire technique has many loops with second-order bends to control the vertical movements of the posterior teeth. It controls the movement of individual teeth and transmits the force produced by Class III elastics. The entire mandibular arch can be distalized and uprighted by a combination of the multiloop edgewise archwire technique and intermaxillary elastics. This combined effect induces a counterclockwise rotation of the occlusal plane, without significant downward and backward rotation of the mandible. This technique is particularly helpful for patients with increased lower face height or an open-bite tendency. However, the open bite can become worse without patient cooperation with elastics.
Extraction of mandibular teeth is occasionally indicated for patients with a moderate Class III skeletal malocclusion and may include extraction of the first premolars or incisors. Extraction of a mandibular incisor is occasionally indicated for patients with an anterior crossbite or an edge-to-edge incisor relationship. The decision is determined by factors such as the severity of anterior crowding in the mandibular arch, the Bolton discrepancy, and the degrees of negative overjet and overbite.
The use of temporary anchorage devices such as microimplants for anchorage has opened up a variety of options for the treatment of Class III patients. In contrast to extraoral anchorage or intermaxillary elastics, the use of temporary anchorage devices as anchorage does not require patient cooperation; these devices simplify the treatment mechanics, reduce the amount of archwire bending, and minimize the loss of anchorage. For treatment of Class III malocclusions, microimplants can be placed in the mandibular or maxillary dentition. For retraction of the mandibular dentition, microimplants can be placed in the retromolar area or the interradicular space between the mandibular first molars and the second premolars, or between the first and second molars. Intra-arch elastics or coil spring is attached to the microimplants, and the entire mandibular arch can be distalized or uprighted with minimal movement of the maxillary dentition. Microimplants can be placed more anteriorly in the maxillary arch and used for en-masse protraction when anterior movement of the maxillary dentition is allowed. The relatively small interradicular space in this area may not allow a large amount of protraction. Placing microimplants apically allows for more movement. The microimplant can also be placed in the anterior palate, and the protraction can be performed from the palatal side. Buccal protraction produces a moment in the outward direction, causing the arch to expand, and palatal protraction produces a moment in the opposite direction, causing arch constriction. Combining palatal and buccal protractions is most efficient, creating a moment and a countermoment in the occlusal plane and, in turn, canceling their side effects. Combining a microimplant with a multiloop edgewise archwire to eliminate the patient compliance factor has been reported to be effective. In addition, patients with Class III problems and facial asymmetry can be treated with temporary anchorage devices to resolve dental problems followed by orthognathic surgery to resolve the remaining skeletal problems.
Improving Anchorage for Camouflage Class III Treatment
Camouflaging became more predictable with microimplants; consequently, more severe Class III problems can be treated. These difficult cases pose great challenges because treatment duration proportionally increases with the level of severity. Sakthi et al reported creating a regional acceleratory phenomenon during the en-masse distalization, and it increased the speed of tooth movements. Average rates of space closure of 1.8 mm per month in the maxilla and 1.57 mm per month in the mandible were observed in the study group compared with 1.02 mm per month in the maxilla and 0.87 mm per month in the mandible in the control group during the first 2 months. Combining regional acceleratory phenomenon creation and a microimplant anchor system may help in achieving satisfactory results with a shorter treatment time. Extraction of the mandibular third molars immediately before distalization can create a regional acceleratory phenomenon and assist in speedy tooth movements. Puncturing cortical bone in localized areas during microimplant-assisted retraction can potentially create a regional acceleratory phenomenon. However, microimplant failure can occur when a regional acceleratory phenomenon is created near the microimplants, and careful operation is essential. Other means of creating accelerated tooth movement, such as laser treatment, vibration, and a pharmaceutical approach, during retraction and protraction of the mandibular and maxillary dentition have been proposed. Although these concepts are promising, more scientific evidence is needed.
When microimplants are used as anchors during retraction and protraction of the mandibular and maxillary dentition, caution must be used not to displace the dentition beyond the alveolar housing. It is tempting to camouflage more severe patients with microimplants because of the mechanical advantages that this absolute anchorage system provides; however, the biologic limitations should be considered, and surgical treatment might be an option.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


