Single-tooth replacement may be effected through various methods, including the use of a resin-bonded fixed partial denture, a conventional fixed partial denture, and a single implant-supported crown. Although the introduction of newer therapeutic modalities, surgical and restorative techniques, and restorative materials has significantly expanded available treatment options, a greater demand is now placed on the diagnostic and treatment planning acumen of the clinician. The questions confronting each clinician are when to apply each treatment modality and how to use these therapeutic approaches to their maximum benefit for the patient. This article focuses on the factors that should be considered when making such clinical decisions and offers a framework within which to formulate appropriate treatment algorithms.
Single-tooth replacement may be effected through use of a resin-bonded fixed partial denture (RBB), a conventional fixed partial denture (FPD), a removable prosthesis, or a single implant-supported crown (SIC). The use of a removable prosthesis is excluded from consideration because the final treatment result of a removable prosthesis for replacement of a single missing tooth is considered a compromise in all situations.
Although the introduction of newer therapeutic modalities, surgical and restorative techniques, and restorative materials has significantly expanded available treatment options, a greater demand is now placed on the diagnostic and treatment planning acumen of the clinician. Mastery of available treatment techniques by the surgeon and the restorative dentist may be easily and predictably accomplished. The questions confronting each clinician are when to apply each treatment modality and how to use these therapeutic approaches to their maximum benefit for the patient.
This article focuses on the factors that should be considered when making such clinical decisions and offers a framework within which to formulate appropriate treatment algorithms.
Comparing success rates of various single tooth replacement treatments
The lack of direct comparative studies assessing treatment outcomes following the use of SICs or tooth-supported FPDs does not allow indisputable proclamations to be made regarding which therapy is most appropriately employed in such situations. Section 3 of the State of the Science of Implant Dentistry Consensus Conference (held by the Academy of Osseointegration in 2006) analyzed the available literature with the aim of answering the question, “In patients requiring single tooth replacement, what are the outcomes of implant- as compared to tooth-supported restorations?” In an effort to assess an adequate number of published articles to draw conclusions, inclusion criteria demanded only a minimum 2-year length of study. Fifty-one articles were assessed from the implant literature and 41 articles were examined from the FPD literature. The success rate of single-implant restorations at 60 months was 95.1%. The cumulative success rate of FPD and RBB was 84.0%. When conventional FPDs were assessed independently of RBBs, however, the 60-month success rate for FPDs was 94.0%. The higher failure/complication rate noted for RBBs is in agreement with that reported by Pjetursson and colleagues in 2008. These investigators conducted a meta-analysis of 93 articles and reported an estimated survival rate for RBBs of 87.7% after 5 years. Failures of RBBs were most often due to debonding or recurrent caries.
Failures of FPDs were most frequently attributed to caries, periodontal disease, and endodontic pathology. Failures of retention and abutment fracture were also noted.
Valderhaug assessed the status of crowned teeth over 25 years and noted caries, endodontic involvement, and periodontics pathology as the primary causes of complications with or without tooth loss.
The principal causes of implant loss or a failing implant, as defined by Albrektsson and colleagues’ criteria, were failure to osseointegrate following initial insertion, progressive bone loss in the face of persistent inflammation, or mechanical overload. Other complications that did not lead to implant loss included abutment loosening/fracture and crown fracture.
Salinas and Eckert noted higher failure rates in data reported in older studies. The significance of this observation is subsequently discussed.
A meta-analysis of 5- and 10-year survival rates of FPDs and SICs was performed by Pjetursson and colleagues. This meta-analysis included cantilevered FPDs and implant-supported FPDs. The estimated 5-year survival rates for FPDs, cantilevered FPDs, and SICs were 93.8%, 91.4%, and 94.5%, respectively. The estimated survival rates after 10 years of function for FPDs, cantilevered FPDs, and SICs were 89.2%, 80.3%, and 89.4%, respectively.
Attempts to compare 5 and 10 years’ cumulative success rates of FPDs and SICs in a tooth-bounded space are complicated by a number of factors in addition to the lack of studies performing direct comparisons between the two treatment modalities.
The assessment of older studies, which may have employed techniques and materials that differ significantly from those currently used, must be undertaken with great caution. There is no doubt that today’s restorative dentist has a greater number of options available for tooth preparation techniques, restorative materials, and cementation than in the past. The field of implant therapy has evolved at least as quickly as that of restorative dentistry in general. In addition to the use of a wider variety of implant diameters, lengths and morphologies, implant surface technology has dramatically altered many of the basic tenants of implantology. The time necessary to attain osseointegration has been significantly shortened, and the initial strength of the osseointegrative bond has been dramatically increased. Most germane to this discussion is that implant success and survival rates have been reported for rough-surface implants that are significantly higher than those previously reported for their smooth-surface counterparts. Success rates for rough-surface implants exceed those in the meta-analyses already discussed for FPDs and SICs.
Finally, the understanding of implant capabilities in the face of various load applications and inflammatory insults continues to evolve. There is no doubt that older studies often reported on implants placed in less than ideal situations because of limitations in available bone and implant sizes and morphologies, or because of a more primitive understanding of implant capabilities in various scenarios. Such considerations account, at least in part, for the lesser 5- and 10-year cumulative success rates of implants reported on in older studies, compared with studies, published within the last 3 to 4 years.
The cumulative success rates of rough-surface implants supporting single crowns are at least equal to those reported on for three-unit FPDs. The questions to be answered are when to use each treatment approach and how best to maximize treatment outcomes with each therapeutic modality.
Diagnostic requirements
Before the initiation of active therapy, a thorough examination must be performed, a diagnosis made, and a comprehensive interdisciplinary treatment plan formulated. A full series of high-quality radiographs must be taken. When necessary, three-dimensional images are also used. Panoramic films are not utilized because their accuracy is insufficient for providing useful information for comprehensive therapy. The components of a thorough clinical examination, including periodontal probing depths, hard and soft tissue examination, models and face-bow records, are well established and not discussed here. It is important to realize, however, that a thorough examination begins with an open discussion with the individual patient. It is crucial that the clinician determine the patient’s needs and desires. In this way, treatment plans may be formulated that are in the best interest of the patient and that represent a greater value for the patient.
Before formulating a comprehensive treatment plan, all potential etiologies must be identified and assessed. In addition to systematic factors, these etiologies include periodontal disease, parafunction, caries, endodontic lesions, trauma, and so forth.
The treating clinician should always formulate an “ideal” treatment plan and present it to the patient. Appropriate and predictable treatment alternatives must also be offered to the patient, thus allowing the patient to chose the treatment option to which he or she is best suited physically, financially, and psychologically.
Clinicians who fail to incorporate regenerative and implant therapies into their treatment armamentaria are depriving their patients of predictable therapeutic possibilities that afford unique treatment outcomes in a variety of situations.
Conversely, teeth that can be predictably restored to health through reasonable means should be maintained if their retention is advantageous to the final treatment plan. Clinicians who claim to be implantologists—performing only implant therapy while ignoring periodontal and other pathologies—do a disservice to patients. Such clinicians include practitioners who perform inadequate periodontal therapy to predictably halt the disease process or who remove teeth that could be treated through predictable periodontal techniques.
Diagnostic requirements
Before the initiation of active therapy, a thorough examination must be performed, a diagnosis made, and a comprehensive interdisciplinary treatment plan formulated. A full series of high-quality radiographs must be taken. When necessary, three-dimensional images are also used. Panoramic films are not utilized because their accuracy is insufficient for providing useful information for comprehensive therapy. The components of a thorough clinical examination, including periodontal probing depths, hard and soft tissue examination, models and face-bow records, are well established and not discussed here. It is important to realize, however, that a thorough examination begins with an open discussion with the individual patient. It is crucial that the clinician determine the patient’s needs and desires. In this way, treatment plans may be formulated that are in the best interest of the patient and that represent a greater value for the patient.
Before formulating a comprehensive treatment plan, all potential etiologies must be identified and assessed. In addition to systematic factors, these etiologies include periodontal disease, parafunction, caries, endodontic lesions, trauma, and so forth.
The treating clinician should always formulate an “ideal” treatment plan and present it to the patient. Appropriate and predictable treatment alternatives must also be offered to the patient, thus allowing the patient to chose the treatment option to which he or she is best suited physically, financially, and psychologically.
Clinicians who fail to incorporate regenerative and implant therapies into their treatment armamentaria are depriving their patients of predictable therapeutic possibilities that afford unique treatment outcomes in a variety of situations.
Conversely, teeth that can be predictably restored to health through reasonable means should be maintained if their retention is advantageous to the final treatment plan. Clinicians who claim to be implantologists—performing only implant therapy while ignoring periodontal and other pathologies—do a disservice to patients. Such clinicians include practitioners who perform inadequate periodontal therapy to predictably halt the disease process or who remove teeth that could be treated through predictable periodontal techniques.
Abutment-tooth considerations
When assessing the appropriateness of the use of specific teeth as abutments for a three-unit FPD, it is assumed that a comprehensive diagnosis has been made and a treatment plan has been formulated, that all dental disease in other areas of the mouth has been managed, and that a nonpathologic occlusal scheme has been created. In such a situation, the abutment teeth themselves must be assessed on a number of levels ( Box 1 ).
-
Overall health of the dentition
-
Occlusal stability
-
Presence of parafunction
-
Periodontal stability
-
Extent of attachment loss
-
Restorative margin position related to the gingival margin
-
Clinical crown available for preparation
-
Amount of tooth remaining following caries excavation
-
Amount of tooth remaining following preparation
-
Need for endodontic therapy
-
Ability to perform endodontic therapy
-
Amount of tooth remaining following endodontic therapy
-
Presence of adequate keratinized tissue
Periodontal Stability
Pocket depths beyond 3 mm are nonideal. Pocket depths of 5 mm or greater should be considered problematic, if not pathologic. Periodontal pockets are recognized as complicating factors in thorough patient and professional plaque control. Waerhaug demonstrated that flossing and brushing are only effective to a depth of about 2.5 mm subgingivally. Beyond this depth, significant amounts of plaque remain attached to the root surface following a patient’s oral hygiene procedures. Professional prophylaxis results are also compromised in the presence of deeper pockets. The failure of root planing to completely remove subgingival plaque and calculus in deeper pockets is well documented in the literature. Through the examination of extracted teeth that had been root planed until they were judged plaque-free by all available clinical parameters, Waerhaug demonstrated the correlation between pocket depth and failure to completely remove subgingival plaque. Instrumentation of pockets measuring 3 mm or less was successful (with regard to total plaque removal) in 83% of the cases. In pockets of 3 to 5 mm in depth, 61% of the teeth exhibited retained plaque after thorough root planing. When pocket depths were 5 mm or more, failure to completely remove adherent plaque was the finding 89% of the time. Tabita and colleagues noted that no tooth demonstrated a plaque-free surface 14 days after thorough root planning when the pretreatment pocket depths were 4 to 6 mm, even in situations in which patients exhibited excellent supragingival plaque control. This is not the forum in which to discuss pocket elimination periodontal surgical therapy. However, care must be taken to ensure no probing depths in excess of 3 to 4 mm are present around potential abutment teeth.
Furcation involvements must also be assessed and eliminated through resection or regeneration if teeth are to be considered good candidates to serve as abutments for an FPD. Periodontally involved furcations cannot be predictably “maintained” through root planning, curettage, and repeated maintenance care sessions. In a longitudinal study of patients who refused active periodontal therapy and who underwent only continuing maintenance care, Becker and colleagues reported an overall rate of tooth loss of 9.8% in the mandible and 11.4% in the maxilla. The same patients demonstrated a rate of tooth loss of 22.5% for mandibular furcated teeth and 17% for maxillary teeth with furcation involvements.
Goldman and colleagues assessed tooth loss in 211 patients treated in periodontal private practices and maintained for 15 to 34 years on a 3- or 6-month recall schedule. Patients were treated with root planning, curettage, and open-flap debridement. Furcation involvements were not eliminated. The overall rate of tooth loss experienced over the course of patient care was 13.4%. However, the incidence of tooth loss of maxillary and mandibular teeth with furcation involvements was 30.7 and 24.2%, respectively. Teeth that exhibited furcation involvements were lost at a greater rate than nonfurcated teeth.
McFall reported on tooth loss in 100 treated patients who had periodontal disease and were maintained for 15 years or longer following active periodontal therapy. Therapy did not eliminate furcation involvements: 11.3% of all teeth were lost over the course of observation. Maxillary teeth that demonstrated furcation involvements were lost at a rate of 22.3%. Mandibular furcated teeth were lost at a rate of 14.7%. Similar findings are repeated throughout the literature.
A study by Fleisher and colleagues underscored the inability to adequately debride a periodontally involved furcation with curettes and ultrasonic instrumentation. Fifty molars were treated through closed curettage or open-flap debridement. All teeth were treated by experienced operators. The teeth were then extracted and stained for the presence of plaque and calculus. Assessment of the extracted and stained teeth demonstrated that only 68% of the tooth surfaces facing the involved furcation were plaque- and calculus-free.
Although there is no doubt that the use of microscopy and appropriate instrumentation greatly improves on this level of efficacy of furcation debridement, the three-dimensional structure of the involved furcation remains. The net result is repopulation of this area by plaque, and re-initiation of a periodontal inflammatory lesion in the area. Such an approach “slows down” the progression of bone and attachment loss and may prove valuable in an older patient, or in one who does not wish to undergo more comprehensive therapy. Most situations, however, require therapy to be aimed at eliminating the periodontally involved furcation and providing the patient with a milieu amenable to appropriate plaque-control efforts.
The treatment approach chosen, whether it is resection, regeneration, a combination of resection and regeneration, or tooth removal and implant placement, depends upon the involved furcation morphology.
Extent of Periodontal Attachment Loss
Following comprehensive periodontal therapy, abutment teeth should demonstrate a lack of probing beyond 3 mm and no furcation involvements. When active periodontal disease has been treated, however, varying degrees of supporting bone and attachment loss will have occurred. In severe cases, the tooth demonstrates mobility due to secondary occlusal trauma, defined as the development of mobility under normal load application due to reduced periodontal support. Teeth demonstrating such mobility may be ill suited to serve as abutments for a three-unit FPD.
Restorative Margin Position Related to the Gingival Margin
Restorative margin position may also influence long-term periodontal health. Plaque accumulation at the restorative margin–tooth interface is a consistent finding in research and in clinical practice. When this margin is subgingival, the resultant increased plaque accumulation often leads to acceleration of periodontal breakdown and recurrent caries. Appropriate preparation of the periodontium for restorative dentistry, including management of supporting bone, covering soft tissues and the tooth–bone interface, has been discussed in detail.
Clinical Crown Available for Preparation and the Development of Appropriate Retention/Resistance Form
A detailed discussion of related concepts and techniques may be found elsewhere. It is imperative that an assessment of the need or the lack of need for such therapy is completed before determining a final course of treatment, because such an assessment has a direct bearing on the physical and financial impacts of care.
The Need for Endodontic Therapy
In addition to impacting the financial ramifications of care when the tooth in question is to serve as an abutment for an FPD, the influence of endodontic therapy on the long-term prognosis of the tooth must be considered. Can endodontic therapy be performed appropriately? Will the residual tooth structure following endodontic therapy be sufficient to withstand load application over time as an abutment for a three-unit FPD? Areas of specific concern are two rooted maxillary first bicuspids following endodontic therapy are of specific concern, because the residual tooth structure in the isthmus of the tooth may be highly prone to fracture; and the aspect of the mesial buccal root of a lower molar that faces the furcation. The ribbon shaped nature of this root also renders it highly susceptible to perforation during endodontic therapy, or fracture at the time of post preparation or insertion, or in subsequent function.
The Presence of an Adequate Band of Attached Keratinized Tissue
Although a number of studies exist that assess the ability to maintain periodontal health in the face of minimal bands of attached keratinized tissue, none of these studies takes into account the added inflammatory insult placed on the periodontium when a restorative margin is placed intrasulcularly. All restorative margins trap some degree of plaque at the restorative margin tooth interface. Therefore, it is prudent to ensure that a stable band of attached keratinized tissue is present to help afford a “fiber barrier,” which, in conjunction with an attachment apparatus consisting of approximately 1 mm of connective tissue attachment and a short junction of epithelium (∼1 mm or less), helps prevent the initiation and propagation of periodontal disease in the area. Such a band of attached keratinized tissue, in addition to having sufficient thickness to prevent recession in the face of inflammation, trauma, or both, must demonstrate an apico coronal dimension of at least 3 mm. In the best of situations, the aforementioned short junctional epithelium and connective tissue attachment will have a dimension of 2 mm. Therefore, it is only when a third millimeter of attached keratinized tissue is present that the aforementioned “fiber barrier” overlays the alveolar bone crest.
Implant receptor site considerations
When contemplating implant placement, a number of site-specific considerations must be assessed ( Box 2 ). These considerations include not only the quantity and quality of available bone for implant placement, but also the position of such bone. When adequate bone is present to place an implant but such placement will result in a nonideal implant position/angulation from a restorative or force distribution point of view, the bone that is present must be classified as inadequate. A comprehensive patient workup must include appropriate diagnostic wax-ups, to allow assessment of ideal implant position and dimension when necessary. The role of implant length and width in long-term success is often misunderstood. The misconceptions that “longer implants are better” and that the maximum-sized implant should be placed whenever possible lead to the need for a greater degree of augmentation therapy and possible encroachment on vital structures.
-
Overall periodontal stability
-
Overall restorative stability
-
Overall occlusal stability
-
Quantity of available bone
-
Quality of available bone
-
Position of available bone
-
Potential encroachment on virtual structures
The role of implant dimension in long-term success
Crown-to-root ratios and Ante’s law are considered cornerstones of treatment planning periodontally healthy and periodontally compromised patients who require prosthetic intervention. The “normal” values for the crown-to-root ratio are 0.60 for maxillary teeth and 0.55 for mandibular teeth. It is important to realize, however, that such numbers are not an indicator of periodontal health or of the absence of periodontal attachment loss around teeth. When excessive wear has occurred and attachment loss is present, the crown-to-root ratio could still be within the normal range. Therefore, a normal crown-to-root ratio should not be interpreted as an indicator of a periodontally healthy situation.
After the introduction of osseointegrating implants to the dental community, it was assumed that longer implants would be more advantageous because they would present a greater surface area for potential osseointegration and a more favorable lever arm following force application. Such a belief seemed to be borne out in early studies documenting the use of machined-screw Brånemark implants (Waltham, Massachusetts). It is important to realize that all these studies were performed on smooth-surface hex-topped implants.
The use of shorter implants significantly impacted the development of appropriate treatment algorithms and the delivery of care. Shorter-implant use allowed the clinician to avoid vital structures such as the sinus floor and the inferior alveolar canal. Their use also eliminated the need for augmentation therapy in many situations. Even when augmentation was still required, a simpler procedure was necessary than for placement of longer implants in the same situation. Unfortunately, the use of shorter implants, has long been viewed as a compromise in patient care.
Do the available finite element analyses and clinical studies support the use of shorter implants to attain treatment outcomes comparable to those attained using longer implants?
Lum found that occlusal forces were distributed primarily to the crestal bone regardless of implant length and were well tolerated by the crestal bone. Parafunctional forces, were not well tolerated by the crestal bone, leading Lum to state that parafunctional forces must be attenuated. Lum also suggested the use of wider implants and a greater number of implants in patients demonstrating a significant parafunctional habit.
Pierriesnard and colleagues performed a finite element analysis on 3.75-mm wide hex-headed screw implants with lengths of 6 mm, 7 mm, 8 mm, 9 mm, 10 mm, 11 mm, and 12 mm, and found that the magnitude and distribution of bone stress was constant and independent of implant length.
Lai and colleagues applied 35 newton centimeters (Ncm) of vertical load to implant cylinders and found that the greatest stress was always concentrated at the neck of the implant. Peak stress was independent of implant length, but it was inversely proportional to the extent of osseointegration.
Holmgren and colleagues reported that implant length had no effect on peak stress magnitude or stress distribution. Stress was concentrated at the bone crest regardless of implant length.
Himmlova and colleagues also found that the greatest force concentration upon force application was always at the bone crest.
The preponderance of finite element analyses demonstrates that peak stresses are always found at the bone–implant interface at the bone crest and are independent of implant length.
Clinical studies
Buser and colleagues demonstrated no difference in implant success rates between shorter and longer lengths in an 8-year life table analysis of 2359 titanium plasma–sprayed Straumann implants (Andover, Massachusetts).
Feldman and colleagues examined 5-year survival rates of 2294 rough-surface Osteotite implants (West Palm Beach, Florida) and 2597 smooth machine-surfaced implants. The difference in cumulative success rates between shorter and longer, rough-surfaced implants was 0.7% and was not statistically significant. The difference in cumulative success rates for smooth-surface implants when assessing implant length was 2.2%, which was statistically significant. Implant surface must be considered in the decision to use shorter implants in various clinical situations.
Deporter and colleagues documented the survival rates of 46 mandibular overdentures, each supported by three short Endopore implants (Toronto, Ontario, Canada). The cumulative implant survival rate 5 to 6 years post therapy was 93.4%.
A publication assessing the clinical results of 5526 Straumann implants documented the use of implants of different lengths in a variety of clinical applications. The implants were followed for a minimum of 72 months in function. The mean time in function was 32 months. Implant length had no influence on the reported cumulative success rates.
Anitua and colleagues, in a retrospective study examining 532 implants of between 7 and 8.5 mm in length with a diameter of 3.3 to 5.5 mm, demonstrated a cumulative survival rate of 99.2%.
Even in the face of a large number of studies supporting the high long-term success rates of shorter implants, another question remains. If the patients in the aforementioned studies were reconstructed at a reduced vertical dimension due to the severity of their oral health problems, a crown-to-“root” ratio approaching the “ideal” numbers quoted for the natural dentition would have resulted. Therefore, the influence of the crown-to-implant ratio on implant success and failure rates must be examined.
Rokni and colleagues examined 199 implants that had been restored with fixed prostheses. Implant length ranged from 5 to 12 mm. The mean crown-to-implant ratio was 1.5. The implants were in function for an average of 4 years. Crown-to-implant ratio and implant length had no effect on the supporting bone levels around the implants.
Tawil and colleagues assessed 262 machined-surfaced Branemark implants in function for a mean time of 53 months, and they found no relationship between crown-to-implant ratio and peri-implant bone loss or implant success/failure rates.
Blanes and colleagues, in a 10-year prospective study of Straumann implants placed in the posterior maxilla, reported no influence of crown-to-implant ratio on implant success in function. A recent publication documenting long-term success of 2073 implants of 6 to 9 mm in length in various applications demonstrated a cumulative success rate of 98.1% to 99%, depending on the clinical application, over a mean time in function of 36.2 months.
If shorter implants are to succeed in function, they must be employed within the parameters already discussed, including appropriate diagnosis and case workup, development of a comprehensive treatment plan, and amelioration of parafunctional forces.
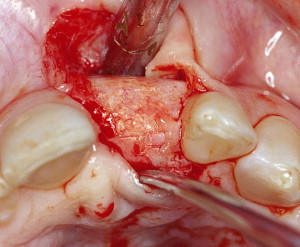
In addition, appropriate regenerative therapy must be performed to determine the need or the lack of need for regenerative therapy to allow placement of an implant of ideal diameter for the tooth to be replaced ( Figs. 1–3 ). It is imperative that implant diameter not be chosen by the available bone. Rather, an implant diameter should be selected that is ideal for the tooth to be replaced. After this implant diameter has been chosen, it must be positioned ideally on the model, as determined by the diagnostic wax-up/surgical stent. It is only at this point that a determination is made of whether regenerative therapy is required. Adequate bone must be present or regenerated to ensure buccal and palatal/lingual bone thickness of at least 2 mm following implant placement. Failure to provide such a thickness of bone significantly increases the chances of bone resorption and implant body exposure under function over time.



Fig. 4 demonstrates a patient who presented missing a maxillary central incisor. Flap reflection revealed a fairly atrophic residual alveolar ridge. Although adequate bone was present to allow implant placement within the remaining alveolar bone, such placement would have represented a threefold compromise. Because the alveolar ridge was deficient, a soft tissue graft would have been necessary to improve the final esthetic treatment outcome. More important, the implant would have been placed off angle and subjected to traumatic off-axis loading. Hsu and colleagues assessed off-angle loading at 0°, 30° and 60° using finite element analyses. They demonstrated that, for each 30° increase in off-angle loading, stress to the crestal bone increased three to four times. Finally, an implant of a narrower than ideal diameter would have been placed, resulting in less surface area for potential osseointegration at the bone crest, the area subjected to the greatest stresses. These stresses, in turn, would be magnified due to the off-angle loading that would occur.
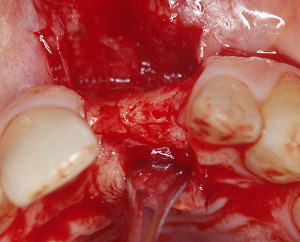
To avoid these problems, appropriate regenerative therapy was performed using particulate graft material beneath a titanium-reinforced Gore-Tex membrane. The net result was an ideal ridge form that allowed placement of an implant of the desired diameter in a restoratively driven position ( Fig. 5 ).
In addition to choosing implant diameter by the dimension of the tooth to be replaced, the implant chosen should demonstrate a rough surface and an internal abutment connection. The advantages of rough-surface implants as opposed to their smooth-surface counterparts have already been discussed. Meadd and colleagues applied 30 Ncm of vertical and horizontal load to implants with internal or external abutment connections. Increased strain at the cervical area was noted around external abutment connection fixtures compared with internal abutment connection implants. Load also was found to be better distributed around internal connection implants than around external connection implants.
The use of wider implants has been called into question by a number of investigators. Ivanoff and colleagues found a significant relationship between wider implant diameters and implant failure. Eckert and colleagues found a higher failure rate of wide-diameter implants as opposed to 3.75-mm diameter implants. Shin and colleagues reported a statistically significant higher failure rate of wider diameter implants compared with standard-diameter implants. However, such a finding may be due to a number of factors, including the necessary learning curve when placing wider-diameter implants and the need to minimize thermal and mechanical damage to the cortical bone during preparation. Equally important is ensurance that adequate bone will remain on the buccal and palatal/lingual aspects of the implant to attain osseointegration and maintain itself under function. As already discussed, such a concern may mandate regenerative therapy even when no implant exposure is noted following placement.
Bischof and colleagues, in a 5-year life table analysis of 263 wide-neck implants, reported a cumulative success rate of 94.3% for the SICs and of 96.21% for the FPDs in the study.
Mericske-Stern and colleagues reported a 5-year cumulative survival rate of 99.1% for wide-neck implants supporting single crowns.
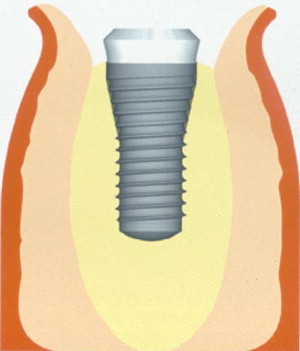
An implant design may also be used that is characterized by a 4.8-mm-wide body with parallel walls, which broadens to a 6.5-mm-wide platform supracrestally ( Fig. 6 ). Such a design helps maintain bone buccally and palatally/lingually to the implant if the implant is placed in a ridge that has undergone resorption, atrophy, or both following tooth removal. The use of a more conventional tapered, wide-platform implant design, which begins to flare to its final restorative platform subcrestally necessitates removal of a greater amount of bone, resulting in a lesser dimension of bone buccally and lingually/palatally following placement ( Fig. 7 ). Such a situation is inherently less stable under function.
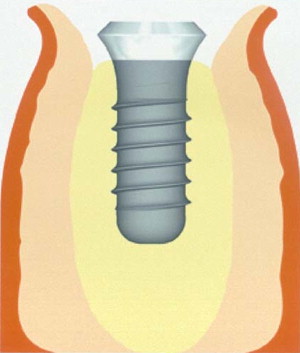
When used appropriately, short implants afford a predictable means of replacing missing teeth in the least traumatic manner possible for patients (see Fig. 6 ).
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


