Dentinal hypersensitivity is a common dental complaint, especially in periodontal patients. It is believed to be mediated by a hydrodynamic mechanism in which various stimuli result in increased fluid flow in dentinal tubules, thereby generating action potentials in associated nerve fibers. Although it is often perceived as mild discomfort by the patient, it can be severe. A variety of interventions has been used, although few have been subjected to rigorous study. This article surveys those in-office treatments that are available, and suggests directions for research so that clinicians may treat patients based on best evidence. Until such evidence is available, it seems prudent to employ therapies that are least likely to cause harm and are reversible.
Dentinal hypersensitivity (DH) is a common dental complaint in adults. In most cases the pain response is initiated and persists only during the application of a suitable stimulus to the exposed dentin surface. DH may occur when dentinal tubules are exposed to the oral environment due to recession and loss of tooth structure. DH is provoked when exposed dentin is subjected to stimuli such as osmotic changes, thermal changes, or mechanical stimuli such as toothbrushing. It has been suggested that DH is mediated by a hydrodynamic mechanism in which a stimulus results in increased fluid flow in the dentinal tubules. This, in turn, activates nerves located on the pulpal aspect of the tubules, resulting in the generation of action potentials which are interpreted as pain by the patient.
There is some controversy regarding exactly what constitutes DH. For example, the European Federation of Periodontology uses the term “root sensitivity” (RS) to describe the DH-like sensitivity seen as a result of periodontal disease or treatment. It is conceivable that there may be a difference between long-standing DH in a patient with incipient recession and very good hygiene and that RS seen in a periodontal patient immediately following flap surgery.
Loss of enamel or cementum (and periodontal tissues) may result in exposed dentin. In 5% to 10% of teeth, the cementum does not reach the cementoenamel junction (CEJ) resulting in exposed dentin. Loss of enamel or tooth structure occurs by attrition, abrasion, or erosion; whereas denudation of the root surface can occur as a result of gingival recession, periodontal therapy, or improper tooth brushing. It has been reported that scaling and root planing may cause increased DH. This is probably because scaling and root planing (and periodontal surgical procedures) may remove the thin outer layer of cementum in the cervical third of the root, thus exposing the dentinal tubules. Gillam and colleagues reported that a significant number of patients reported DH following restorative treatment, but this study used a survey technique and it is possible that some patients may have actually been reporting hypersensitivity from microleakage or operative trauma.
DH is more accurately described as a symptom rather than a true disease entity. It is characterized as transient sharp pain originating from various types of stimuli. A number of other dental conditions such as carious lesions, cracked tooth syndrome, fractured restorations or teeth, periodontal disease, postoperative hypersensitivity, palatal-gingival grooves, enamel defects, a congenitally open CEJ, improperly insulated metallic restorations, occlusal traumatism, and tooth whitening may produce similar symptoms. According to a recent review, “DH is usually diagnosed after other possible conditions have been eliminated” and may be considered a diagnosis of exclusion. The role of plaque as an etiologic factor in DH is not resolved, although it has been suggested that dental plaque promotes and sustains DH, and that plaque control is important in preventing its development. However, it has been noted that hypersensitive dentin is often found in toothbrush abrasion areas that are almost plaque-free. Suge and colleagues recently demonstrated in a dog model that the patency of dentinal tubules was more reduced in teeth subjected to stringent plaque control. These authors suggest that plaque control may promote the natural resolution of DH in some circumstances.
The prevalence of DH in the adult population ranges between 8% and 35%. It has been reported that DH affects about 40 million adults in the United States. In an international survey, Murray and Roberts found that the prevalence of hypersensitive teeth was consistent across all the countries surveyed, affecting approximately 15% of the population. It has been shown that there is a slightly higher predilection of DH in females than males.
The peak prevalence of DH has been variously reported as occurring between the second and fifth decades of life. Orchardson and Collins reported a peak between 20 and 25 years, whereas Addy found peak prevalence to occur at the end of the third decade. Fischer and colleagues found it to be between 40 and 49 years.
DH most commonly occurs on the buccal aspect of permanent teeth near the CEJ, which is also the site that most frequently exhibits dentin exposure. Dentin exposure may also occur on occlusal and lingual cervical surfaces, but hypersensitivity is rarely reported in these locations. With regard to tooth type, it has been reported that canines and premolars in either arch are the most frequently involved.
Although DH can be very troubling to some patients, Gillam and colleagues found that most individuals affected with DH did not perceive it to be a severe problem and consequently did not seek treatment. For example, only one in four patients with DH reported use of a desensitizing toothpaste.
Several factors can reduce dentin permeability and subsequently contribute to the spontaneous remission of DH. For example, a dentin smear layer often covers the exposed surface of dentin and may occlude the dentinal tubules, thereby reducing DH. Adherence of salivary proteins to the dentinal surface and adherence of plasma proteins to the inner dentin surface may also reduce hypersensitivity, as can the formation of less permeable reparative dentin by the pulp. Finally, the obturation of tubules by the formation of intratubular crystals from salivary minerals, dentinal fluids’ mineral deposits, and calculus formation on the surface of dentin all reduce permeability.
These natural mechanisms can be used to explain the clinical course of DH following periodontal surgery. During root planing, tubules remain occluded by the smear layer created by root surface debridement. This smear layer may reduce permeability and also lowers hydraulic conductance by blocking fluid movement. As the smear layer dissolves, however, the permeability of dentin increases, resulting in the symptoms of DH in some patients. This occurs about 1 week after periodontal surgery, correlating with the observation of subjects having the highest DH rates 1 to 3 weeks postoperatively. Within a few weeks, the tubules may become partially occluded (eg, with crystalline deposits), thus decreasing permeability to bacterial products and intraoral stimuli. This correlates with the decreased DH symptoms within a period of 6 weeks postsurgery.
DH affects as many as 40 million adults in the United States. It is likely that the incidence of DH will increase because people are retaining their teeth longer, are living longer, and more dental root surfaces are exposed through gingival recession, scaling and root planing, and periodontal surgery. Therefore, identifying its mechanisms and causes may become more important.
Spontaneous resolution of dentinal hypersensitivity
Several factors can reduce dentin permeability and may contribute to the spontaneous remission of DH. There are a variety of mechanisms by which natural obturation of permeable tubules can occur. As noted above, formation of a smear layer covers exposed dentinal surfaces and may occlude dentinal tubules. Dentin covered with a smear layer may be less hypersensitive, although this is a difficult concept to test experimentally. In any event, the smear layer is easily removed and is, therefore, unlikely to provide any meaningful protection against DH.
Dental professionals have a variety of interventions to manage DH, including in-office treatments and self-applied products for home use. Much of the literature on the treatment of DH is anecdotal. There are few well-powered clinical trials that have examined interventions for DH. The purpose of this review is to review and critique the various treatment modalities for DH.
Search strategy
The search mechanism for this review included a MEDLINE search to identify English-language articles published between 1960 to 2007. The following search terms, including terms truncated with an asterisk, were used:
-
dentinal
-
dentin ∗
-
hypersensitivity
-
hypersensitiv ∗
-
sensitivity
-
desensiti ∗
-
desensitiz ∗
-
oxalate ∗
-
resin ∗
-
laser ∗
Various combinations of these terms were used. The “related articles” feature of PubMed was also used to identify additional citations. The searches yielded a large number of citations, most of which were found to represent a low level of evidence (eg, small exploratory studies and in vitro experiments). All returned citations were examined by title and abstract to ascertain applicability. The original inclusion criteria were human studies of these types: randomized clinical trials, clinical trials, meta-analyses, systematic reviews, or evidence-based practice guidelines. If the content was related to the research question and met the criteria, then the full report was retrieved. Very few publications met even the most liberal interpretation of the inclusion criteria.
A more focused search was then conducted, using the search terms “dentinal hypersensitivity” and using the “limits” tool to restrict the search to clinical trials, meta-analyses, practice guidelines, and randomized controlled trials. This search was also limited to English-language publications. Twenty-five citations were returned, of which none were systematic reviews of the topic. Only seven of the reports were published since 2000. Most were small pilot or exploratory studies that tested only two interventions. The more inclusive search did yield a number of narrative reviews, but none were systematic reviews or meta-analyses. Thus, the level of evidence in support of any intervention is rather weak, according to the techniques of evidence-based health care. The remainder of this article describes and analyzes the results of this search as it applies to in-office interventions for DH. However, the level of evidence is insufficient to permit definitive recommendations regarding the management of this condition. Owing to the paucity of high-level evidence, a systematic review of this topic is not possible at this time. Therefore, this article has, of necessity, been configured as a narrative review.
Search strategy
The search mechanism for this review included a MEDLINE search to identify English-language articles published between 1960 to 2007. The following search terms, including terms truncated with an asterisk, were used:
-
dentinal
-
dentin ∗
-
hypersensitivity
-
hypersensitiv ∗
-
sensitivity
-
desensiti ∗
-
desensitiz ∗
-
oxalate ∗
-
resin ∗
-
laser ∗
Various combinations of these terms were used. The “related articles” feature of PubMed was also used to identify additional citations. The searches yielded a large number of citations, most of which were found to represent a low level of evidence (eg, small exploratory studies and in vitro experiments). All returned citations were examined by title and abstract to ascertain applicability. The original inclusion criteria were human studies of these types: randomized clinical trials, clinical trials, meta-analyses, systematic reviews, or evidence-based practice guidelines. If the content was related to the research question and met the criteria, then the full report was retrieved. Very few publications met even the most liberal interpretation of the inclusion criteria.
A more focused search was then conducted, using the search terms “dentinal hypersensitivity” and using the “limits” tool to restrict the search to clinical trials, meta-analyses, practice guidelines, and randomized controlled trials. This search was also limited to English-language publications. Twenty-five citations were returned, of which none were systematic reviews of the topic. Only seven of the reports were published since 2000. Most were small pilot or exploratory studies that tested only two interventions. The more inclusive search did yield a number of narrative reviews, but none were systematic reviews or meta-analyses. Thus, the level of evidence in support of any intervention is rather weak, according to the techniques of evidence-based health care. The remainder of this article describes and analyzes the results of this search as it applies to in-office interventions for DH. However, the level of evidence is insufficient to permit definitive recommendations regarding the management of this condition. Owing to the paucity of high-level evidence, a systematic review of this topic is not possible at this time. Therefore, this article has, of necessity, been configured as a narrative review.
Clinical management of dentinal hypersensitivity: in-office treatments
Treatment of DH can be accomplished by covering the exposed tubules with soft tissue grafts or restorative materials, occluding the tubules with materials that cause precipitation of crystals within the tubules, desensitization by way of laser treatment, or through desensitization of the nerve fibers with potassium nitrate. All of these techniques have been used, but few have been subjected to rigorous testing for efficacy.
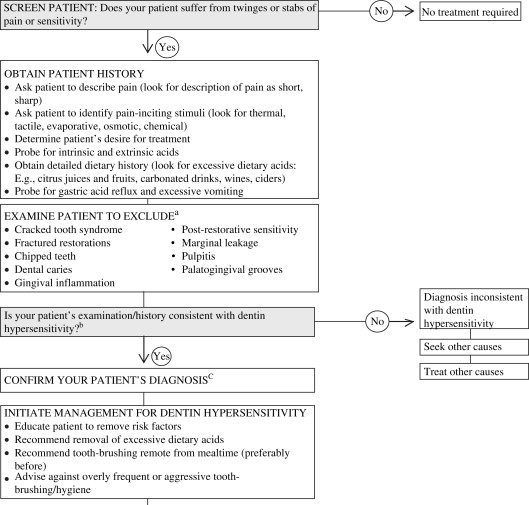
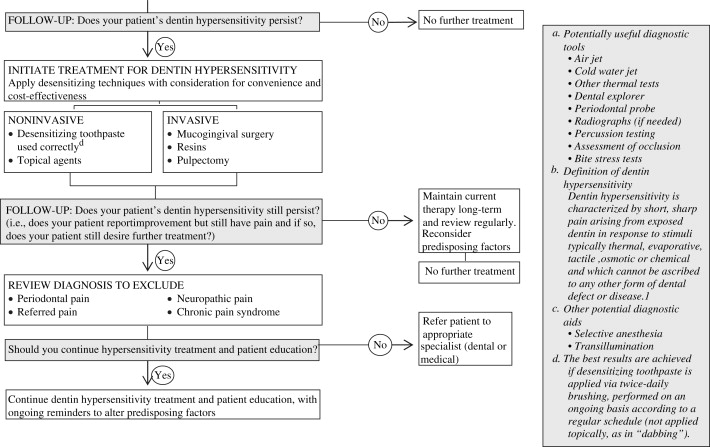
A recent consensus statement on DH by the Canadian Advisory Board on Dentin Hypersensitivity came to a similar conclusion after reviewing the state of the literature. These authorities stated that “the need for consensus recommendations was made evident by the lack of clear and robust evidence in the dental literature.” This advisory board went on to say that the “high prevalence of the condition, underdiagnosis and widespread availability of noninvasive, efficacious and inexpensive preventive treatment further underscored the need for direction.” This board developed an algorithm for diagnosis and treatment that is consistent with the evidence ( Fig. 1 ).
Cavity Varnishes
Brannstrom suggested the application of cavity lining and varnishes under restorations, so that the smear layer plugging open tubules is retained. In a narrative review of DH interventions, Wycoff recommended the use of a copal varnish, since covering exposed dentin with a thin film of varnish often renders it nonhypersensitive. For more sustained relief, a 2% sodium fluoride-containing varnish can be applied. The duration of effect of this varnish is usually 3 months. Further studies by Pashley and colleagues evaluated a series of commercial cavity varnishes and bases for efficacy in reducing dentin permeability. They reported that all cavity varnishes tested decreased dentin permeability by 20% to 50%. Use of a 5% sodium fluoride varnish has been shown to form a protective layer of calcium fluoride that inhibits fluid flow within tubules, which has been suggested to be effective in the treatment of DH.
Corona and colleagues compared the galium-aluminium-arsenide laser and sodium fluoride varnish (Duraphat) in the treatment of DH. They found no statistically significant difference between fluoride varnish and laser.
In a controlled study, Mazor and colleagues evaluated the effect of topical application of a sustained-release device in the form of a varnish containing strontium chloride on DH. They found that varnish containing strontium chloride showed a marked decrease in DH as compared with the placebo and untreated group.
Corticosteroids
It has been suggested that the application of anti-inflammatory drugs such as glucocorticoids to cavity preparations and exposed dentin may reduce DH by way of their effect on pain mediators. However, there is little experimental evidence to support or refute the use of such agents. In a double-blind study, Lawson and Huff found that paramethasone had a significant desensitizing action. Furseth and Mjor have reported complete obturation of dentinal tubules; hence, reduction of dentin permeability after an application of a corticosteroids preparation to exposed dentin. Mjor reported less pulpal inflammation following restoration with a corticosteroid-containing cement than with amalgam in a nonhuman primate model. In summary, there is insufficient evidence to support or refute the use of corticosteroids in the treatment of DH.
Calcium Compounds
Calcium hydroxide [Ca (OH) 2 ] has been used many years for the treatment of DH, particularly after root planing. Ca (OH) 2 has little or no direct effect on dentin sensory nerve activity. However, it is thought that it induces peritubular dentin mineralization and, subsequently, less hypersensitive dentin Calcium compounds have compared favorably to other desensitizing agents in vitro. For example, Suge and colleagues examined occlusion of dentinal tubules by scanning electron microscopy (SEM) and reported that calcium phosphate precipitation was more effective than potassium oxalate in occluding dentinal tubules.
Levin and colleagues found that the application of Ca(OH) 2 paste to hypersensitive exposed dentin resulted in an immediate decrease of DH in over 90% of treated teeth. Jorkjend and Tronstad applied a paste of Ca(OH) 2 to the exposed root surface following periodontal surgery. A thin layer of methacrylate and periodontal dressing where placed on top of the Ca(OH) 2 . After removing the dressing 7 days later, they found that the teeth were no longer hypersensitive to cold, air, carbohydrates, toothbrushing, toothpicks, scaling or ultrasonic devices. Giniger and colleagues also found that amorphous calcium added to a 16% carbamide peroxide-equivalent bleaching gel, significantly reduced DH.
Yates and colleagues assessed the therapeutic effect of amorphous calcium phosphate in the treatment of DH in a split-mouth, randomized, placebo-controlled study, and reported no significant difference between the calcium phosphate group and the placebo group at the 84 day posttreatment follow-up.
Oxalates
Oxalate-containing products are a popular agent for in-office treatment of DH. Oxalate desensitizing agents are easy to apply, safe, relatively inexpensive, and well-tolerated by patients. It has also been shown that potassium oxalate has both dentinal tubule obturation properties and inhibitory effects caused by the potassium ions actions on nerve activity. Oxalate ions react with calcium to form insoluble calcium oxalate crystals that bind tightly to dentin and obturate the dentinal tubules. It has been shown that a 3% monohydrogen monopotassium oxalate releases a high concentration of calcium ions and accelerates crystal formation.
Three types of oxalates are available: 6% ferric oxalate, 30% dipotassium oxalate, and 3% monohydrogen monopotassium oxalate. In vitro studies have found that potassium oxalate preparations reduce dentin permeability. There is evidence from animal studies that any relief provided may be relatively short-lived as the oxalate crystals are dissolved or removed over time. Unfortunately, such in vitro and animal studies are, at best, suggestive and represent a weak level of evidence.
More relevant is an exploratory study by Pillon and colleagues in which a single application of 3% potassium oxalate gel was applied following nonsurgical periodontal therapy. There was a significant reduction in DH on those teeth treated by 3% potassium oxalate compared with teeth treated with placebo. Unfortunately, the sample size was quite small (n = 15) and the duration of follow-up quite short (ie, 21 days posttreatment).
Oxalate-containing phytocomplexes have recently been investigated for possible effects on DH. For example, Sauro and colleagues reported that dentinal permeability of extracted third molars was reduced after a single exposure to the oxalate-containing phytocomplexes. These same investigators have demonstrated that these phytocomplexes can protect the smear layer on recently instrumented dentin from removal by acidic soft drinks. This finding may be worthy of additional research, as it has been shown that scaling and root planing produces a smear layer that reduces dentinal permeability, but this smear layer is acid-labile.
While some of these reports are promising and worthy of further investigation, there is insufficient evidence to confirm the effectiveness of oxalates as an in-office treatment for DH.
Resins and Adhesives
The rationale for the use of resins and adhesives is to seal the dentinal tubules and hence to preclude the transmission of pain causing stimuli to the pulpal nerve fibers. This mode of treatment is performed on localized hypersensitive dentin after other forms of treatment have failed. Resin-based materials have been reported to successfully reduce DH. Unfortunately, many of the reports on these materials are in vitro studies which examine surrogate outcomes such as dentinal permeability.
Brannstrom and colleagues found that impregnating the dentinal tubules with a restorative resin material resulted in significant relief from DH. Wycoff suggested that adhesives be used for severe cases of DH that were unresponsive to other interventions. He specifically recommended the use of a glass ionomer cement, but the evidence supporting this recommendation is weak. Copeland reported successful treatment of DH for up to 18 months in 89% of hypersensitive teeth treated by Scotchbond.
A combination product consisting of an aqueous solution of 5% glutaraldehyde and 35% hydroxyethyl methacrylate (Gluma Desensitizer) has been reported to be an effective desensitizing agent for up to 9 months. The glutaraldehyde intrinsically blocks dentinal tubules counteracting the hydrodynamic mechanism that leads to DH. It should be noted that a significant placebo effect was seen with water, which yielded reductions in DH ranging from 5% to 27%. A subsequent study found that a low-viscosity glass ionomer was more effective than the glutaraldehyde-resin product at 25 months posttreatment. This was a small pilot study involving 14 subjects.
In another small exploratory study of eight patients, Ianzano and colleagues evaluated the effectiveness of a dentin primer (N-tolylglycine-glycidyl methacrylate and bisphenyl dimethacrylate) in the treatment of DH. These investigators reported that a single application of the primer was effective over the 9-month study period.
In summary, resin restorations have been used to cover areas of denuded dentin. This would seem to be a rational treatment strategy. As noted above, some investigators have reported significant success with such interventions, but most of these studies suffered from small sample size. It would also be helpful to have information on the longevity and safety of such treatments. Larger studies will be needed to validate these interventions.
Laser Treatment
There are a number of reports that suggest that laser treatment may be useful in the treatment of DH, although definitive trials are lacking. A recent review of the literature by Kimura and colleagues reported that effectiveness of laser treatment of DH ranged from 5% to 100%. However, these authors also reported that the laser was less effective in cases of severe DH.
Moritz and colleagues examined the long-term effects of combined carbon dioxide (CO 2 ) laser treatment and fluoridation on DH. He found that 97% of laser group showed complete relief from DH compared with conventional fluoridation. Furthermore, SEM examination at 18 months posttreatment showed complete closure of dentinal tubules. These authors concluded that the CO 2 laser is an ideal desensitizer for DH. More recently, Slutzky-Goldberg and colleagues have demonstrated that CO 2 laser treatment resulted in decreased permeability of dentinal tubules as shown by a dye penetration test.
Zhang and colleagues studied the effect of irradiated teeth by CO 2 laser on the pulp and in the treatment of DH. He found that all patients were free of DH immediately following laser treatment. Over 3 months, the CO 2 laser treatment reduced DH to air stimulus by 50% without obvious loss of pulpal vitality.
Lan and Liu reported that the neodymium: yttrium-aluminum-garnet (Nd:YAG) laser reduced DH to air by 65% and to tactile stimulation by 77%. In a subsequent publication, these authors reported that Nd:YAG laser irradiation at can be used to seal the exposed dentinal tubules and suggested that this may be the mechanism by which DH is affected.
In a clinical and SEM study, Kumar and Mehta found that Nd:YAG laser irradiation in combination with 5% sodium fluoride varnish has higher efficacy in the management of DH than either treatment alone. The SEM findings were a reduction in number or patency of tubules.
Not all studies have reported positive results. In a double-blind, controlled, split-mouth clinical trial, Lier and colleagues evaluated the efficacy of a single Nd:YAG laser application on treatment of DH versus negative control. There was no difference between the Nd:YAG laser group and the placebo group at 16 weeks.
The combination of a dental laser with other modes of treatment for DH was an effective and lasting dentinal tubule obturation procedure. Lan and colleagues used SEM to evaluate the combination effect of sodium fluoride and Nd:YAG laser irradiation on human dentinal tubules in vitro. They found that 90% of dentinal tubules were occluded when fluoride varnish was first applied to exposed dentin and then treated with a ND:YAG laser. Furthermore, the fluoride varnish within the dentinal tubules could not be removed by electric toothbrushing. Once again, this is an in vitro study using a surrogate variable, as opposed to a clinical trial.
A combination of dental laser with dentin bonding agents has been reported to be an efficient method for improving dentin bonding. Theoretically, this combination could provide better and more lasting occlusion of the dentinal tubules, although robust evidence to support this assertion is lacking. Vlacic and colleagues reported the utility of using a laser-activated fluoride therapy to protect enamel from erosive challenges that could cause dentin exposure and hypersensitivity. Unfortunately, these were also in vitro studies that have yet to be tested in the clinical setting.
Some of the clinical studies using various lasers for treatment of DH report very encouraging results. However, additional studies are needed to conclusively demonstrate the utility and safety of such interventions.
Gingival Augmentation
Gingival reconstructive surgical periodontal procedures, such as root coverage grafts, have been used to treat DH due to gingival recession. Although many investigators have reported on the efficacy of various methods of soft tissue augmentation for root coverage, it was not possible to locate any studies which were designed to specifically test such grafting as a treatment for DH. A PubMed search was conducted using the search terms “hypersensitivity” and “graft. ∗ ” The search was limited to clinical trials, meta-analyses, practice guidelines, and randomized controlled trials. Two of the citations involved soft tissue augmentation of recession defects, but neither was tested as an intervention for the treatment of DH. Broader searches were conducted, and studies were located that discussed postoperative sensitivity as an undesirable outcome, but no study was located that tested the reduction of DH as a primary aim. Thus, as with other in-office treatments for DH, the evidence is insufficient to provide definitive guidelines for clinical decision-making.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


