Fig. 3.1
Flow chart of the etiological factors contributing to DH
3.3.1 Loss of Enamel
3.3.1.1 Attrition
Attrition is defined as the gradual loss of tooth substance because of occlusal contacts with opposing dentition or restoration without the presence of food (Hattab and Yassin 2000; Kaidonis 2008). Physiological attrition gradually increases with age and accompanies the reduction of cusp height and the occlusal incline plane, with the loss of enamel and dentin (Hattab and Yassin 2000). However, it is interesting to note that the loss of dental hard tissue may not be a symptom of DH because of the formation of secondary dentin (Johnson and Sivers 1987; Hattab and Yassin 2000). Although attrition is a physiologic process, it can be accelerated by other factors, such as parafunctional habits, clenching and bruxism, traumatic occlusion, grinding, and malocclusion (Hattab and Yassin 2000). The occlusal and incisal surfaces are primarily affected, and tooth wear can be extensive in severe bruxism (Litonjua et al. 2003a). It may also involve the interproximal surfaces of the tooth, where tooth wear is associated with a decrease in the dental arch (Murphy 1964; Grippo et al. 2004). Studies have reported that bruxism may affect 8–20 % of the adult population (Glaros 1981), and tooth wear progresses more rapidly in patients with bruxism than in those with no bruxism (Xhonga 1977). Smith and associates reported that bruxism alone is an etiological factor in 11 % of referred cases of tooth wear and was the contributing etiological factor in approximately two-thirds of cases (Smith and Knight 1984). The clinical feature of attrition is characterized by an area with a relatively flat facet accompanying a well-circumscribed border on the cusp tip or ridge of a molar or the incisal edge of the anterior teeth (Litonjua et al. 2003a; Hattab and Yassin 2000). In the opposing arch, similar facets can be appreciated clinically. In areas in which dentin is exposed, the lesion appears to be flat without “cupping or scooping” (Kaidonis 2008). Although attrition can act independently, several combinations of the mechanism of tooth wear could act synergistically, thereby affecting the progression of loss of dental hard tissue. These combined mechanisms of tooth wear consist of “attrition-abfraction” and “attrition-corrosion,” which involves the integrated action of stress and corrosive agents on the areas of tooth wear because of attrition (Grippo et al. 2004). In summary, attrition can be exaggerated by parafunctional habits such as bruxism and by other predisposing factors such as abrasion, erosion, and abfraction, which result in the progressive loss of dental hard tissue and exposure of the dentin (Fig. 3.2).


Fig. 3.2
An elderly patient suffered from attrition due to gradual physiological loss of occlusal tooth substance
3.3.1.2 Abrasion
Dental abrasion is the pathologic wearing of teeth as the result of abnormal processes, habits, or abrasive substances. It is a non-carious loss of tooth substance that is deprived of bacterial involvement. It can be referred to as a mechanical process that produces tooth wear because of friction caused by external materials or objects (Knight 1969). Dental abrasion has been associated with diet, occupation, and toothbrushing. Mechanical abrasions result from the consumption of a coarse diet that produces wear on the tooth surface. This type of tooth wear is relatively common clinically but is frequently overlooked (Grippo et al. 2004). It often involves the buccal surface of the lower molars and the palatal surfaces of the upper molars (Kaidonis 2008). Certain occupations can result in dental abrasion; frequently affected are carpenters, tailors, and musicians, who may demonstrate abrasion of maxillary incisal edges (Hattab and Yassin 2000; Johnson and Sivers 1987). Other activities involving foreign objects, such as biting pens or hairpins, smoking pipes, or biting one’s nails could result in the development of notched abrasive lesions on the incisal edges. The clinical presentation of abrasive lesions appears to involve the entire occlusal surface, unlike attrition, which affects the wear facet. The exposed dentin appears to be scooped (Kaidonis 2008). Abrasive lesions may have sharp margins, in contrast to the broad and smooth margins of erosive lesions (Levitch et al. 1994). The most common cause of dental abrasion is toothbrushing. Toothbrush abrasion can result from incorrect technique, the application of heavy forces during brushing (Padbury and Ash 1974; Bergstrom and Lavstedt 1979), the frequency of toothbrushing (Phaneuf et al. 1962; Dyer et al. 2000; Bergstrom and Lavstedt 1979), bristle stiffness (Zimmer et al. 2011), and the use of abrasive toothpaste (Osborne-Smith et al. 1999; Dyer et al. 2000). The prevalence of toothbrushing as a causative factor is, however, unclear; published studies suggest that it affects 5–86 % of members of the population studied (Litonjua et al. 2003a). The cervical area at the cement-enamel junction on the buccal surface of all teeth is predominantly affected by toothbrush abrasion. The lesion appears as a V-shaped or rounded notch and commonly affects the maxillary canine, premolar, and first molar regions (Hattab and Yassin 2000; Bishop et al. 1997). Litonjua and co-workers studied the morphology of cervical lesions by analyzing experimentally induced toothbrush abrasive lesions. They found that 50 % of abrasive lesions were wedge shaped, 22 % were rounded, and 28 % of lesions were a combination of wedge shaped and round (Litonjua et al. 2004). Kitchin and colleagues reported an association between oral hygiene and the presence of abrasions: patients with good oral hygiene were more likely to exhibit abrasion than those with deprived oral hygiene. Also, the incidence of abrasion of the cementum and dentin increased from 42 % among patients aged 20–29 years to 76 % among those aged 50–59 years (Kitchin 1941). The dentin and cementum are less dense than enamel; therefore, tissue loss occurs more rapidly and progresses farther in these areas (Davis and Winter 1980). Right-handed patients exhibit more lesions on the teeth on the left side of the month than on those on the right side, probably because they use more force when brushing the left side of the mouth (Sangnes and Gjermo 1976). Radentz and associates reported that patients use more brushing force on the initial areas they brush; thus, these areas are more likely to suffer abrasion due to increased brushing forces (Radentz et al. 1976). Bergstrom and co-workers examined 818 individual adult groups and found a 30 % prevalence of cervical abrasion and a 12 % prevalence of wedge-shaped cervical lesions. They also reported a relationship between prevalence and severity of abrasion and the frequency of toothbrushing (patients who brushed twice daily), particularly when a horizontal toothbrushing technique was used (Bergstrom and Lavstedt 1979; Bartlett and Shah 2006). Although a relationship between the severity of abrasion and toothbrushing has been reported, some authors believe that erosion may play an important role in the progression of tooth wear. Attin and associates evaluated the period of remineralization of enamel previously eroded by brushing abrasion and concluded that the resistance to abrasion of eroded enamel continually increases as remineralization time increases (Attin et al. 2000). An in situ study by Jaeggi and colleagues was designed to assess the effect of tooth bushing at 0, 30, and 60 min after the exposure of enamel to citric acid (an erosive agent). Toothbrush abrasion was more severe at 0 min than at 60 min; thus, it is recommended that patients avoid brushing for at least 1 h after the intake of acidic food or beverages to allow a period of remineralization that can reestablish the resistance of formerly eroded enamel to toothbrush abrasion (Jaeggi and Lussi 1999). Patients with partial dentures may show signs of abrasion because of the lesions caused by clasps. Grippo and co-workers suggested that, although abrasion can act independently to produce the loss of dental tissue, it can also occur in combination with other predisposing factors, such as attrition, erosion, and abfraction, to produce a more additive effect on the process of tooth wear (Grippo et al. 2004). When it occurs in combination with attrition or abfraction, abrasion can further exaggerate the loss of tooth structure by friction, heavy occlusal forces, and the accumulation of stress concentration by loading forces on the weaker areas, subsequently causing the tooth substance to break (Grippo et al. 2004) (Fig. 3.3).
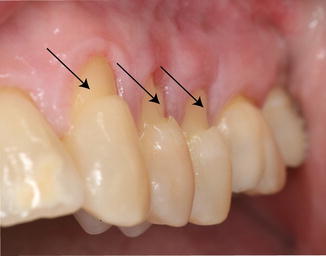
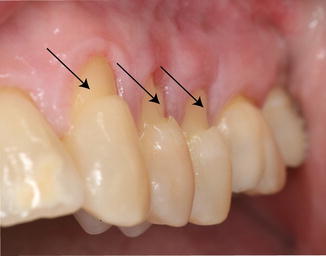
Fig. 3.3
Pathologic wearing of tooth substance of abrasion lesion (arrows) as the result of mechanical friction of foreign object
3.3.1.3 Corrosion/Erosion
Dental erosion is the loss of mineralized dental hard tissue caused by the direct impact of exogenous and endogenous acids. These acids produce a chemical reaction leading to the dissolution of hydroxyapatite crystals and to the softening and eventual loss of dental hard tissue. The term “corrosion” has been encouraged as a replacement for “erosion” because it more precisely describes the chemical and electrochemical actions that can cause tooth wear (Grippo et al. 2004). The lesion can be self-reported by patients as an esthetic concern or may be associated with dentin hypersensitivity. Erosive lesions in their early stages may appear as smooth concave or rounded defects, whereas advanced erosive lesions may display concavities identified as cupping (Litonjua et al. 2003a). The clinical presentation of erosion can be easily differentiated from bacterial decay that produces rough lesions (Hattab and Yassin 2000). Erosion associated with extrinsic factors such as diet may manifest itself as a scooped-out depression on the labial surface of the maxillary front teeth (Hattab and Yassin 2000; Johnson and Sivers 1987; Litonjua et al. 2003a). Erosion can affect younger children. A recent survey reported that the prevalence of dental erosion was 15 % in children aged 12 years and was twice as high in those aged 15 years. Furthermore, the mandibular first molars were the most frequently affected by dental erosion (Arnadottir et al. 2010). Although erosion can basically affect any teeth in the mouth, the site and severity of the lesions may depend on the exposure and frequency of the erosive materials or agents that come into contact with the teeth. The dissolution of the tooth surface results from extrinsic or intrinsic acids. Exposure of the tooth to extrinsic acids can occur as the result of diet, medication, occupation, or environment. The most common source of dietary acid is liquid drinks such as grapefruit, lime, or orange juice or wine. Aerated drinks such as colas can produce erosive lesions. Acid is also present in pickled foods and citrus fruits. Beverages popular in the USA, such as sports drinks (Gatorade), energy drinks (Red Bull), aerated drinks (Mountain Dew and Coca-Cola), can erode both the enamel and the root (Ehlen et al. 2008). Holding the drink in the mouth for longer periods before swallowing and taking long sips has been associated with the risk of erosion (Johansson et al. 2004). It has also been suggested that drinking methods should be addressed in the dietary counseling of patients with dental erosion (Johansson et al. 2004). Grenby and colleagues reported that some “healthful drinks,” such as pure citrus juice, exhibit higher dental erosive properties than carbonated cola drinks (Grenby et al. 1989). Commonly, exposed dentin surfaces may not be sensitive because of the natural process of occlusion of tubules by a smear layer. However, it is quite possible that the abrasive action of a toothbrush or even contact with erosive agents can eliminate the protective smear layer and expose the dentinal tubule, thereby creating a potentially sensitive site. Zandim and co-workers reported that several natural orange juices, such as those of navel oranges, Valencia oranges, and mandarin oranges, are more effective in exposing the dentinal tubules and removing the smear layer than are the juices of lime oranges and limes. However, when lime orange and lime juices were applied in combination with toothbrush friction, significantly more of the smear layer was removed (Zandim et al. 2008). Therefore, it has been suggested that erosive acids may be a predisposing factor in the progression of dentin tissue loss and sensitivity because it can act synergistically with abrasion in the oral cavity. A recent meta-analysis found that soft drinks are associated with a 2.4-fold higher risk of dental erosion (Li et al. 2012). Saliva and local fluid contribute protective functions that can help protect both enamel and dentin against the dental erosive process (Knight 1969). Properties of saliva, such as its cleansing, buffering capacity (Piangprach et al. 2009), remineralization, and acquired pellicle (Nekrashevych and Stosser 2003) can protect the tooth surface from acid attack. Piangprach and associates found that the concentrations of urea and salivary buffering capacity were higher in saliva samples of patients with erosive lesions than in samples from patients without erosion (Piangprach et al. 2009). Low saliva flow and poor buffering capacity allow the constant retention of exogenous and endogenous acids that would potentiate the erosive events on dental tissue (Zero and Lussi 2005). The critical pH of enamel is approximately 5.5; intermittent or continuous exposure of enamel to any acidic product with a pH lower than 5.5 can dissolve hydroxyapatite crystals (Meurman and ten Cate 1996). It has been reported that the pH of a cola-type drink is lower than this critical pH and is sufficient to demineralize the enamel (Ferrazzano et al. 2012a). However, it is interesting to note that once the tooth’s contact with the acidic agent is stopped or a chelating material is provided, the process of demineralization ends. Because erosion is a multifactorial event, oral health providers should evaluate the condition and diagnose the etiology of the erosive lesion. Dentists should recommend that patients control their frequency of soft drink consumption, should educate them about the consequences if it is continued, and should provide replacements such as milk as a substitute to prevent the progression of dental erosion. Zero and co-workers have suggested that there is a strong connection between dentin hypersensitivity and erosion (Zero and Lussi 2005).
Some forms of erosion can be associated with occupation. Occupation erosion occurs as the result of workers’ exposure to erosive agents over a long period of time. Petersen and colleagues screened workers in a German battery factory and reported severe erosion on the front teeth and attrition on the posterior teeth of those who were exposed to sulfuric acid (Petersen and Gormsen 1991). Gas-chlorinated swimming pools with water maintained at a pH of 2.7 generated dental erosion because of the exposure of the swimmers to acid (Centerwall et al. 1986). Gray and associates reported cervical erosion and occlusal pitting in patients whose occupation was associated with wine tasting (Gray et al. 1998). The severity of facial erosion of the maxillary front teeth was increased in patients employed in pharmaceutical and biotechnological work because of an increased exposure to proteolytic enzymes (Westergaard et al. 2001). Dental products may be associated with dental erosion because of either excessive toothbrushing or faulty oral hygiene practices. Some over-the-counter mouthwashes have a low pH because of their ethanol content and may have the potential to expose the dentinal tubule (Bhatti et al. 1994). An in vitro study has demonstrated the remineralization potential of fluoride toothpaste on erosive lesions (Rirattanapong et al. 2012). Toothbrushing after consuming an acidic diet can speed up the chemical erosion activity on the tooth surface and may increase patients’ susceptibility to dental erosion (Zero 1996; Jaeggi and Lussi 1999).
Another etiological factor for dental erosion is stomach acid, a key source of intrinsic acid. Stomach acid can enter the oral cavity as a consequence of chronic vomiting, eating disorders such as bulimia, or gastroesophageal reflux disease. Patients will often report their reflux symptoms; however, some may not. Therefore, oral health providers should obtain a thorough medical history so that they can address this condition. The clinical presentation of erosion due to gastrointestinal reflux is the presence of concave depressions on the palatal and occlusal surfaces of the maxillary teeth and on the buccal and occlusal surfaces of the mandibular teeth (Hattab and Yassin 2000; Litonjua et al. 2003a). The erosive lesions produced as a result of chronic vomiting have been called perimolysis or perimylolysis (Hattab and Yassin 2000). Medication-induced dental erosion has been associated with asthma (Sontag 2000; Sivasithamparam et al. 2002), vitamin C preparations (Eriksson and Angmar-Mansson 1986), and hydrochloric acid for gastric achlorhydria (Hellwig and Lussi 2006; Dugmore and Rock 2003). In general, erosion is a chronic process that patients may or may not be aware of until it has reached an advanced stage. This condition must be detected early if further progression of this condition is to be prevented. A careful medical history, including information about diet, salivary function, and adjunct tooth wear processes as predisposing factors and a lifestyle evaluation are necessary (Fig. 3.4) (Table 3.1).
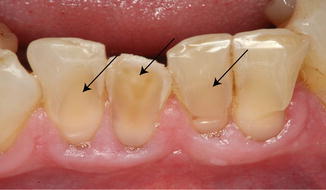
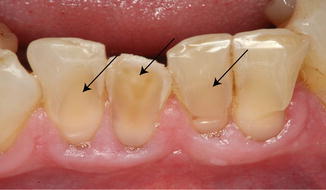
Fig. 3.4
Erosion lesion (arrows) due to loss of mineralized dental hard tissue caused by the direct impact of exogenous acids
Table 3.1
Etiological factors for dental erosion
|
Extrinsic
|
Intrinsic
|
|||
|---|---|---|---|---|
|
Dietary
|
Medication
|
Occupation
|
Environment/lifestyle
|
Chronic vomiting
|
|
Acidic fruits
|
Aspirin
|
Wine tasting
|
Healthier lifestyle – consuming more fruits/juices
|
Bulimia nervosa
|
|
Asthma medication
|
||||
|
Acidic drinks
|
Vitamin C
|
Battery manufacturing
|
Excessive oral hygiene – tooth brushing habit
|
Gastric achlorhydria
|
|
Pharmaceutical and biotechnical work
|
||||
|
Aerated beverages
|
Toothpastes
|
Swimmers
|
Self-inflicting
|
Chronic alcoholism
|
|
Mouthwashes
|
||||
|
Mouth refresher
|
||||
3.3.1.4 Toothbrushing
3.3.1.4.1 Excessive Toothbrushing
Traumatic toothbrushing is believed to be responsible for the development of gingival lacerations, cementum loss, and root dentin exposure, all of which predispose patients to cervical lesion sensitivity. Mannerberg and associates reported that toothbrushing produces scratches on tooth surfaces that can eventually cease to exist because of the deposition of inorganic substances that precipitate from saliva (Mannerberg 1961). Toothbrushing by itself can eliminate plaque but may not be able to remove stains from tooth surfaces. Alone, toothbrushing may not harm enamel surfaces (Addy 2005). Toothpaste is a potential adjunct oral health-care product that can eliminate stains and superficial deposits because their key ingredient is an abrasive (Addy 2005). Relative dentin abrasivity (RDA) indicates the degree of abrasivity of toothpastes. Joiner and co-workers performed an in situ study to evaluate toothpastes with various RDAs and found that the amount of enamel wear caused by toothpastes may not be clinically significant (Joiner et al. 2004). However, brushing with toothpaste does abrade dentin, and the rate of wear corresponds to the paste’s RDA value (Addy et al. 2002). Absi and colleagues reported that toothbrushing alone could not open the tubule; however, brushing with toothpaste exerted a constructive effect by forming a smear layer and closing the dentinal tubules (Absi et al. 1992). West and associates found that using toothpastes other than silica-based pastes to brush teeth with localized sites of dentin exposure can play a role in the removal of the smear layer, thus opening the tubule and leading to the development of DH (West et al. 2002). Interestingly, some authors have reported that some toothpastes remove the smear layer and then occlude the dentinal tubule with the abrasive particles that they contain (Banfield and Addy 2004; West et al. 2002). Therefore, it can be said that toothbrushing alone or with toothpaste can produce an insignificant change on the enamel surface; however, both types of brushing can enhance tooth wear by the action of a more prevailing process such as erosion (Fig. 3.5).
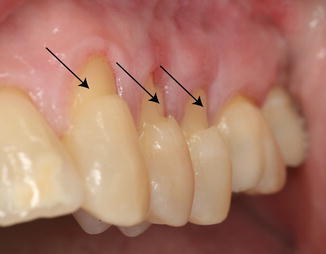
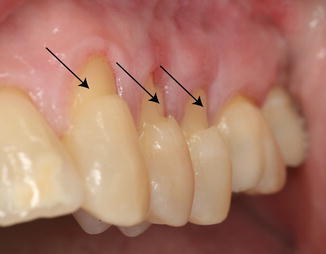
Fig. 3.5
Gingival recession and subsequent abrasion lesion (arrows) due to traumatic toothbrushing habit in right-handed patient
3.3.1.4.2 Lack of Toothbrushing
Lack of toothbrushing results in the accumulation of plaque. The role of plaque in the etiology of DH is debatable. Published reports indicate that patients who maintain effective plaque control are not affected by DH (Tammaro et al. 2000), whereas those whose root surface is exposed to plaque are predisposed to the development of DH (Trowbridge and Silver 1990; Cox 1994). Kawasaki and colleagues validated the effects of plaque control on dentinal tubule widening and occlusion in association with DH. They created dentin slabs by using human teeth and subjected one group of them to no measures for controlling plaque, a second group to mechanical plaque control with brushing, and a third group to chemical plaque control with chlorhexidine. They found that wider tubules were not associated with plaque control and that occluded tubules were associated with mechanical and chemical plaque-control measures (Kawasaki et al. 2001). Bacteria from dental plaque may penetrate the dentinal tubules and release their products, thereby stimulating the nerve fibers. It has been reported that bacteria can enter the dentinal tubule by dissolving the smear layer and can progress toward the dental pulp, thereby inducing DH (Adriaens et al. 1988). Adriaens and associates found that substantial numbers of viable bacteria are present throughout the radicular dentin of teeth with no periodontal diseases or caries (Adriaens et al. 1988). On the other hand, it is believed that plaque does not contribute to DH, because its incidence is higher among patients with excessive toothbrush abrasion at sites that are almost plaque free (Addy et al. 1987; Addy and Pearce 1994).
3.3.1.5 Abfraction
Abfraction, a new term introduced by Grippo (1991), is associated with cervical lesions that are anticipated to play an important role in the process of tooth wear. It is related to eccentric occlusal loading (Dababneh et al. 1999). The lateral occlusal forces exerted during mastication, parafunction, or malocclusion produce tensile stresses that can result in cusp flexure and may transmit these stresses particularly in the cervical areas, resulting in weakening and eventually cracking in the cervical region around the cementoenamel junction (CEJ) (Lee and Eakle 1984; Hattab and Yassin 2000). The lesion appears to be a V-shaped defect in the cervical areas of the buccal surface of the teeth; this lesion must be differentiated from tooth abrasion, microfracture (Bevenius et al. 1993), and erosion lesion. Clinical observations have suggested that abfraction lesions are more prevalent in maxillary (upper jaw) incisors (Grippo 1991) and in bruxism patients (Xhonga 1977). Although abfraction can be linked to DH because of the development of cervical cracks and lesions, there is not enough published evidence to suggest that abfraction alone can be a potential etiological factor in tooth wear (Litonjua et al. 2003b). On the other hand, factors such as erosion and abrasion are more potentiating and can occur in combination with abfraction to further elicit the development of DH (Fig. 3.6).


Fig. 3.6
Abfraction-related tooth wear that is related to eccentric occlusal loading
3.3.2 Iatrogenic Factors
Mwangi and colleagues performed a retrospective survey to evaluate the long-term relationship between malocclusion, orthodontic treatment, and tooth wear. They found no significant differences in tooth wear between patients who had or had not received orthodontic treatment. Furthermore, they also reported no correlation between tooth wear and acidic intake in these patients (Mwangi et al. 2009).
Dentin hypersensitivity is also reported after the application of restorative materials, tooth-whitening procedures, and ill-fitting trays with a surplus of tooth-whitening materials (Nathanson 1997). Restorations with a composite material that involves an acid-etching step performed beyond the CEJ margin can also predispose patients to sensitivity. Furthermore, sensitivity can also occur if the dentin tubule that is newly cut during cavity preparation is left exposed during the restorative procedure. The pain associated with restorative sensitivity can occur for a short period of time. However, if the dental pulp tissue is involved because of the process of caries, severe pain that persists for a longer duration must be differentiated from DH. Incorrect use of whitening solutions (bleaching agents) places patients at risk of DH and gingival irritation, particularly when the night guard vital bleaching technique is used (Leonard et al. 1997). Although DH is a common side effect after using bleaching agents, the mechanism of bleaching-associated sensitivity is not fully understood. It has been shown that bleaching agents may change the surface roughness of enamel and predispose teeth to enamel erosion (Azrak et al. 2010). Controlled clinical studies have shown that although some bleaching gels produce some alterations of the enamel surface, these alterations return to normal within 3 months (Turkun et al. 2002). A recent clinical study found that tooth sensitivity is lower (16.7–26.7 %) when hydrogen peroxide bleaching gels are used (Reis et al. 2013). On the other hand, some clinical studies have reported higher levels of tooth sensitivity ranging from 63 % (Marson et al. 2008) to 80 % (Reis et al. 2011). It is recommended that clinical practitioners carefully evaluate exposed dentin, enamel fractures or cracks, large restorations, and cervical erosion because patients with these conditions may be prone to sensitivity after vital tooth bleaching (Nathanson 1997).
3.3.3 Physiological Cause
The CEJ is the anatomical juncture of the enamel that covers the crown and the cementum that covers the root of the teeth. In some patients, enamel and cementum fail to meet at the CEJ, thus resulting in the exposure of some amount of dentin. As the patient ages, the number of teeth with exposed roots increases in association with gingival recession. An increasing number of aged patients with missing natural teeth tend to experience dental extrusion of the opposing tooth, increased gingival recession (Marini et al. 2004), and root exposure, all of which place them at increased risk of DH.
3.3.4 Cementum Loss
Loss of cementum is a multifactorial condition. Exposure of root dentin is apparent in periodontal diseases and is usually associated with gingival recession. It is not uncommon to find exposed root dentin after periodontal surgery, where it can be associated with the healing process. Exposed root dentin is also associated with mechanical trauma such as vigorous toothbrushing.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


