Cone-beam CT (CBCT) has made a dramatic contribution and has been quickly adopted in endodontics. It is a game changer in research and clinical applications. Although CBCT and its application in implantology is well known, the surgical placement of implants is now a factor in endodontics. This article illustrates unique applications of CBCT in implantology in a specialty endodontic facility. Endodontics creates the foundation for restorative dentistry for a healthy tooth, a well-treated endodontically treated tooth, or a well-placed dental implant. CBCT helps make this possible and predictable.
Key points
- •
When a procedure demands precise localization, cone beam computed tomography (CBCT) provides undistorted, unmagnified, reliable images that contribute to accurate implant placement.
- •
When first available, CBCT was considered too expensive for the average dental facility. Now, CBCT is affordable, available, user-friendly, and readily accepted.
- •
CBCT is becoming the imaging modality of choice for many dental tasks. The use of CBCT should be seriously considered in many significant dental procedures.
Case 1: tooth number 14
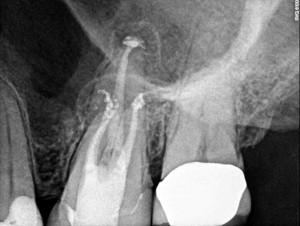
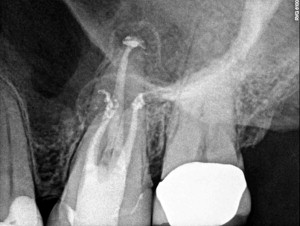
The first case illustrates missed canal and failing endodontic therapy. A 56-year-old woman was referred for evaluation and potential retreatment of tooth number 14. The tooth was treated approximately 2 years earlier by an endodontist. The patient returned to her general dentist numerous times over 18 months and reported pain and discomfort in the upper left quadrant. She was told that things looked fine based on two-dimensional (2D) periapical radiograph (PA) ( Fig. 1 ). The patient finally requested to be referred to another endodontist.

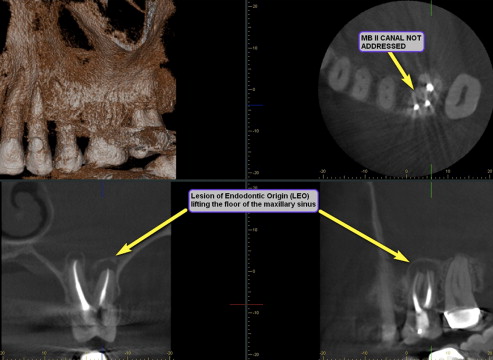
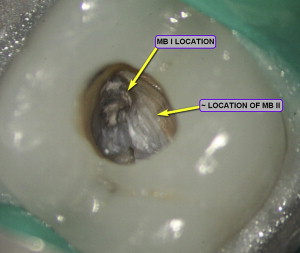
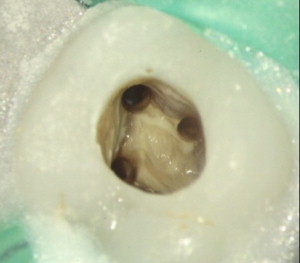
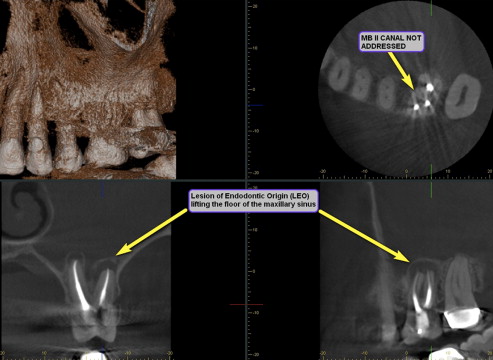
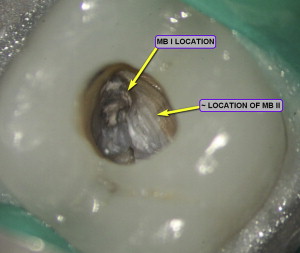
A preoperative CBCT was taken that clearly illustrated lesions of endodontic origin (LEOs) periradicularly on all three roots ( Fig. 2 ). There was no indication that an mesial buccal II canal was ever treated. Nonsurgical retreatment was initiated ( Fig. 3 ). The root canal system consisted of four canals ( Fig. 4 ). The system was reshaped and disinfected. Calcium hydroxide was placed as an interappointment medicament.
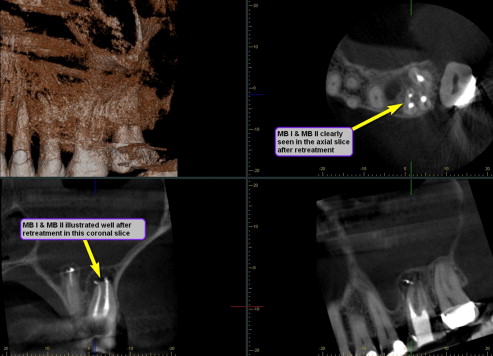
Both the coronal and axial CBCT slices ( Fig. 5 ) clearly illustrate obturation of the MB II canal, which has a separate portal of exit from the MB I ( Fig. 6 ).
Case 1: tooth number 14
The first case illustrates missed canal and failing endodontic therapy. A 56-year-old woman was referred for evaluation and potential retreatment of tooth number 14. The tooth was treated approximately 2 years earlier by an endodontist. The patient returned to her general dentist numerous times over 18 months and reported pain and discomfort in the upper left quadrant. She was told that things looked fine based on two-dimensional (2D) periapical radiograph (PA) ( Fig. 1 ). The patient finally requested to be referred to another endodontist.

A preoperative CBCT was taken that clearly illustrated lesions of endodontic origin (LEOs) periradicularly on all three roots ( Fig. 2 ). There was no indication that an mesial buccal II canal was ever treated. Nonsurgical retreatment was initiated ( Fig. 3 ). The root canal system consisted of four canals ( Fig. 4 ). The system was reshaped and disinfected. Calcium hydroxide was placed as an interappointment medicament.
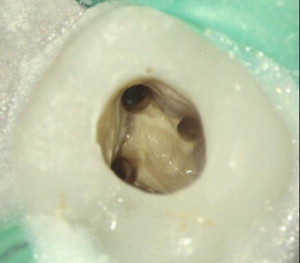
Both the coronal and axial CBCT slices ( Fig. 5 ) clearly illustrate obturation of the MB II canal, which has a separate portal of exit from the MB I ( Fig. 6 ).

Case 2: maxillary first bicuspid, tooth number 12
The second case illustrates a diagnosis ( Fig. 7 ) of irreversible pulpitis caused by symptomatic apical periodontitis. A coronal fracture was present ( Figs. 8 and 9 ). Tooth number 12 exhibited class III mobility and was given a hopeless prognosis due to the extent of the coronal fracture. The patient chose an implant instead of a three-unit fixed bridge. The CBCT data were used to plan the location and size of the implant ( Fig. 10 ).





