This report describes a novel concept of en-masse retraction with temporary skeletal anchorage devices in place of posterior bonding or banding. The patient was a Korean woman, aged 24 years 4 months, with a Class II Division 1 malocclusion with severe mandibular anterior crowding. Both molars showed decalcification of the cervical areas. Partial osseointegration-based C-implants and C-tube plates were placed bilaterally between the maxillary second premolars and the first molars and in the posterior mandible. These temporary skeletal anchorage devices were used as independent appliances for full retraction of the maxillary and mandibular anterior teeth 3-dimensionally without the assistance of posterior bonded appliances. The posterior occlusion was not changed during treatment, and Class I occlusal relationships with optimal overjet and overbite were achieved. The 7-year posttreatment records showed a stable result.
A familiar concern during orthodontic treatment is to control Newton’s third law, the law of action and reaction. Orthodontic force protocols such as Tweed’s philosophy of anchorage preparation and the level anchorage system have been suggested to maintain or minimize any change in the molar positions in maximum anchorage cases. However, tooth-borne anchorage inevitably slips even with the application of complicated mechanics or supplementary appliances to control anchorage.
Numerous intraosseous anchors such as microscrews, miniplates, and palatal onplants have been introduced to reinforce anchorage and are preferred over dental or extraoral anchorage when loss of any anchorage is unwanted. Even though intraosseous anchors enable clinicians to move the teeth without extraoral appliances, they are typically used as anchorage support for the posterior teeth, bearing orthodontic appliances, which bring the usual risks of decalcification, periodontal side effects, and the need to close the remaining band space. We present a treatment protocol called biocreative therapy, which provides carefully controlled retraction of the anterior teeth in 3 planes without the assistance of bonded or banded anchor teeth. The use of the osseointegrated C-implant allows the application complex retraction forces (torque and intrusion) without the need for posterior bands or brackets. This treatment method is excellent when 100% anchorage is needed in patients with dental caries, severe periodontal disease, or missing teeth.
Diagnosis and etiology
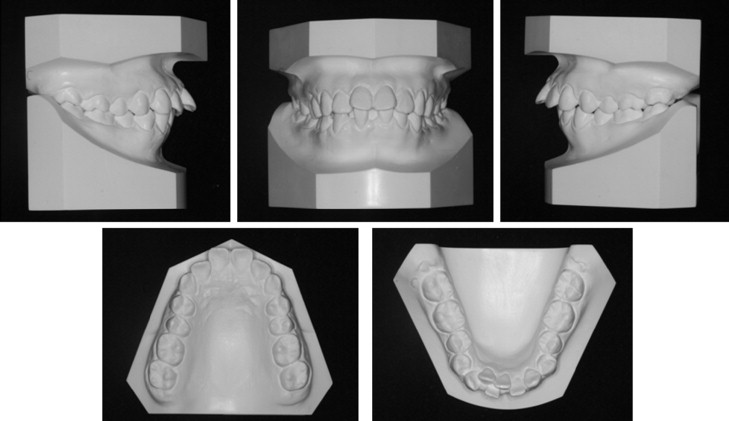
A woman, aged 24 years 4 months, came with a complaint of poor appearance caused by protruding maxillary and mandibular anterior teeth and a gummy smile tendency. The intraoral examination showed a Class II malocclusion with bidentoalveolar protrusion, midline discrepancy, and severe crowding of the anterior teeth ( Figs 1 and 2 ). Decalcification on the bucco-cervical areas of both molars was found in the intraoral examination. The cephalometric analysis showed a skeletal Class II pattern with an ANB angle of 8°, and excessive proclination of the maxillary and mandibular incisors (U1-NA angle, 32°; L1-NB angle, 39°; interincisal angle, 102°) ( Fig 3 , Table ).


| Average (female) ∗ | Pretreatment | Posttreatment | 7 years retention | |
|---|---|---|---|---|
| SNA (°) | 81.6 | 83 | 83 | 82 |
| SNB (°) | 79.2 | 75 | 75 | 75 |
| ANB (°) | 2.4 | 8 | 8 | 7 |
| PFH/AFH (%) | 66.8 | 57.3 | 58.0 | 57.1 |
| SN-OP (°) | 17.9 | 22 | 26 | 26 |
| FH-UI (°) | 116.0 | 125 | 101 | 101 |
| FMA (°) | 24.3 | 35 | 35 | 35 |
| IMPA (°) | 95.9 | 99 | 89 | 89 |
| FMIA (°) | 59.8 | 46 | 56 | 56 |
| UL to E-plane (mm) | −0.9 | 6 | 3 | 2 |
| LL to E-plane (mm) | 0.6 | 7 | 3 | 3 |
| Interincisal angle (°) | 123.8 | 102 | 135 | 134 |
| U1-NA (mm) | 7.3 | 9 | 0 | 1 |
| U1-NA (°) | 25.3 | 32 | 8 | 9 |
| L1 To NB (mm) | 7.9 | 11 | 9 | 9 |
| L1-NB (°) | 28.4 | 39 | 30 | 30 |
| SN-PP (°) | 10.2 | 12 | 12 | 10 |
∗ For Korean women, data from Korean Association of Orthodontists.
Treatment objectives
The treatment objectives based on the results of the cephalometric and study model analyses were to (1) camouflage the skeletal malocclusion by retraction of the anterior dentition after extracting all first premolars, (2) correct the molar and canine relationships to a Class I relationship with mutually protected canine guidance, (3) achieve optimal overjet and overbite, and (4) improve the facial balance.
Treatment objectives
The treatment objectives based on the results of the cephalometric and study model analyses were to (1) camouflage the skeletal malocclusion by retraction of the anterior dentition after extracting all first premolars, (2) correct the molar and canine relationships to a Class I relationship with mutually protected canine guidance, (3) achieve optimal overjet and overbite, and (4) improve the facial balance.
Treatment alternatives
A headgear treatment option for anchorage support was discussed, but the patient was a clerk and rejected this treatment option. All treatment plans required the extraction of all first premolars. Based on these objectives, 3 treatment options were proposed. The first alternative was to perform an anterior segmental osteotomy under general anesthesia. However, the patient refused the surgical treatment option and requested full retraction of the maxillary and mandibular anterior teeth by using the first premolar extraction spaces with conventional orthodontic treatment.
Thus, en-masse retraction by using temporary skeletal anchorage devices with 2 alternatives was presented to the patient: (1) retract the anterior teeth with conventional mini-implants as anchorage support by reinforcing the bonded or banded posterior anchorage teeth during anterior retraction, or (2) use temporary skeletal anchorage devices as independent appliances for anterior alignment and retraction without the assistance of bonded or banded posterior anchorage teeth. After en-masse retraction, conventional orthodontic treatment would be performed on the posterior dentition for detailing. The third treatment plan was selected because no molar banding or bonding during en-masse retraction would allow good oral hygiene, considering the decalcification areas of both molars, and since the posterior occlusion was excellent.
Treatment progress
Treatment was preceded by placement of C-tube plates (prototype made of pure gold casting) on the buccal cortical plate of the mandible ( Fig 4 ). These miniplates have a 0.9-mm diameter hole to accept an archwire and can be used when mini-implants are inappropriate (proximity of sinus or nerve, bone loss, or root proximation). We first placed 0.022 × 0.028-in preadjusted brackets on the 6 mandibular anterior teeth, followed by the placement of a 0.016 × 0.022-in stainless steel archwire appliance between the anterior teeth and the miniplate hole. We applied traction to the canines with 0.25-in, 3.5-oz elastics for anterior alignment. One month later, we placed 2 C-implants (CIMPLANT, Seoul, Korea), 1.8 mm in diameter and 8.5 mm in length. The screw surfaces of these temporary skeletal anchorage devices are sand blasted with a large grit and acid etched. They were inserted into the interseptal bone between the maxillary second premolar and first molar. After 4 weeks of healing, maxillary en-masse retraction was started ( Fig 5 , A and B ).




