Introduction
A common orthodontic problem is a deep overbite malocclusion. Because of its high relapse tendency, it is also one of the most challenging problems to treat. To minimize relapse, the morphologic characteristics of patients need to be considered. The aim of this study was to compare deepbite relapse in 3 groups of patients categorized by vertical growth type.
Methods
The total sample included 60 patients treated at the University of Washington in Seattle, all with initial overbites greater than 50%. Data were collected from casts and cephalometric radiographs at 3 time points: pretreatment, posttreatment, and 10 years postretention. A mixed-effects model (analysis of variance) and post-hoc t tests were used for the statistical evaluations.
Results
The high-angle subjects showed the least deepbite relapse (0.1 ± 1.1 mm), whereas the low-angle (1.2 ± 0.9 mm) and the normal-angle (1.4 ± 1.3 mm) subjects had statistically significant relapses P <0.001. This overbite relapse might be partially due to changes in the mandibular and interincisal angles, which were also observed in these 2 groups.
Conclusions
High-angle subjects tend to relapse less in overbite than do low-angle and normal-angle subjects in the long term.
A common problem faced by orthodontists is the maintenance of deep overbite correction, which is considered to be one of the most challenging to retain, specifically because of its high tendency for postorthodontic relapse. Kim and Little analyzed 62 Class II Division 2 patients after an average of 15 years postretention and observed an average overbite relapse of 1.4 mm, and Canut and Arias used a similar sample and found a mean overbite relapse of 0.9 ± 1.2 mm during the postretention period. Al-Buraiki et al studied 25 subjects who were treated with cervical headgear and intrusion mechanics, and found that overbite increased by 0.7 mm, or 17%, during the posttreatment period. Berg observed a mean overbite reduction of 49.2% during treatment; it relapsed by 18.8% after treatment. Hirschfelder and Hertrich reported a mean relapse in overbite of 1.7 mm in 93.3% of their 49 deepbite subjects. Schutz-Fransson et al observed a mean relapse of 0.8 mm 11 years after treatment in a deepbite group, whereas in their untreated control group, a bite opening of 0.7 mm during the same time period was noted.
Overbite correction and retention require the clinician to be cognizant of certain morphologic characteristics of patients predisposed to greater amounts of relapse. Various characteristics have been studied and implicated, including relapse in the curve of Spee, relapse of the interincisal angle, pressure from the lips, and facial type with corresponding musculature.
Accordingly, if certain patients can be identified as high-risk candidates for overbite relapse, treatment mechanics and retention strategies might need to be altered for them to achieve the most stable outcome. With that in mind, the aim of this study was to evaluate and compare the amount of relapse of anterior deepbite together with the changes in various morphologic characteristics in a group of orthodontically treated patients with full-fixed appliances according to their facial type.
Material and methods
The sample was drawn from the long-term postretention database of the graduate orthodontic program at the University of Washington in Seattle. Of 858 available subjects, 309 were treated without extractions. Furthermore, the following inclusion criteria were applied to the remaining sample: pretreatment (T1), posttreatment (T2), and long-term postretention (T3) records of sufficient quality to allow for accurate landmark identification; permanent dentition; at least 11 years old at the start of orthodontic treatment; at least 10 years out of retention; treatment with full-fixed orthodontic appliances; and incisor overbites of 50% or greater at T1 and 50% or less at T2. Patients treated with growth modification and sectional arch mechanics were excluded to enable evaluation of the full-fixed appliance therapy approach only. The final study sample consisted of 60 subjects with either skeletal Class I (ANB, 0°-4°) or skeletal Class II (ANB, >4°) patterns, but 1 subject had a mild skeletal Class III pattern (ANB, <0°) ( Tables I and II ).
| Group | n | Sex distribution (n) | Sagittal jaw relationship (n) | |||
|---|---|---|---|---|---|---|
| Male | Female | ANB 0°-4° | ANB >4° | ANB <0° | ||
| Normal angle | 28 | 13 | 15 | 18 | 10 | 0 |
| Low angle | 16 | 10 | 6 | 8 | 7 | 1 |
| High angle | 16 | 7 | 9 | 8 | 8 | 0 |
| Group | Age (y) | Mandibular plane angle (°) | Y-axis (°) | Lower anterior facial height (mm) | Mean treatment time (mo) | Mean postretention time (y) | ||
|---|---|---|---|---|---|---|---|---|
| T1 | T2 | T3 | ||||||
| Normal angle | 13.4 | 15.9 | 28.9 | 32.5 | 66.3 | 42.5 | 30 | 12.9 |
| Low angle | 14.0 | 16.2 | 29.2 | 26.5 | 64.1 | 38.8 | 26 | 13.0 |
| High angle | 13.5 | 16.1 | 31.1 | 37.8 | 70.5 | 45.6 | 32 | 15.0 |
All subjects underwent routine edgewise therapy followed by a minimum of 2 years in retention (either maxillary and mandibular Hawley, or maxillary Hawley and mandibular fixed appliances). Maxillary anterior biteplates were incorporated into the retainers in 3 patients (2 normal-angle subjects and 1 high-angle subject).
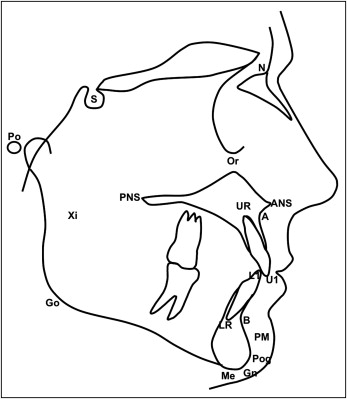
The cephalometric radiographs were scanned into imaging software (version 11.0; Dolphin Imaging, Chatsworth, Calif). Standard cephalometric landmarks ( Fig 1 ) were then identified on each radiograph. From these points, the following measurements were determined on each lateral cephalogram: SNA, SNB, ANB, mandibular plane angle, y-axis, FMA, occlusal plane angle, maxillary incisor angle, mandibular incisor angle, interincisal angle, anterior face height, posterior face height, upper face height, and lower anterior face height. The vertical positions of the maxillary and mandibular central incisors, premolars, and first molars were measured perpendicular to the palatal and mandibular planes, respectively ( Table III ). Additionally, overbite, overjet, and curve of Spee were also measured on the dental casts at each time point ( Table III ).
| Variable | Definition |
|---|---|
| SNA (°) | The acute angle formed by the intersection of a line from sella (S) to nasion (N) and a line from N to A-point (A). |
| SNB (°) | The acute angle formed by the intersection of a line from S to N and a line from N to B-point (B). |
| ANB (°) | This is measured as the difference between the SNA and SNB angles (SNA – SNB = ANB). |
| MPA (°) | The acute angle formed by the intersection of a line from S to N and a line from gonion (Go) to gnathion (Gn). |
| Y-axis (°) | The acute angle formed by the intersection of a line from porion (Pr) to orbitale (Or), which is also known as the Frankfort horizontal (FH), and a line from S to Gn. |
| LFH (°) | The acute angle formed by the corpus axis (line from Xi point [Xi] to protruberance menti [PM]) and a line from Xi to ANS. |
| FMA (°) | The acute angle formed by the intersection of a line from Pr to Or, which is also known as the FH, and a line from Go to menton (Me), which is also known as the mandibular plane (MP). |
| N-Me (mm) | The linear distance from N to Me. |
| S-Go (mm) | The linear distance from S to Go. |
| N-ANS (mm) | The linear distance from N to anterior nasal spine (ANS). |
| ANS-Me (mm) | The linear distance from ANS to Me. |
| OP-SN (°) | The acute angle formed by the intersection of a line through the overlapping cusps of the first premolars and the first molars (occlusal plane) and a line from S to N. |
| U1-SN (°) | The angle formed by the intersection of a line from the upper incisal tip (U1) to the upper incisal root apex (UR) and a line from S to N. |
| L1-MP (°) | The angle formed by the intersection of a line from the lower incisal tip (L1) to the lower incisal root apex (LR) and a line from Go to Gn, also known as the MP. |
| U1-L1 (°) | The angle formed by the intersection of a line from the U1 to the UR and a line from the L1 to the LR. |
| Overbite (mm) | The amount of vertical incisor overlap, measured as a linear distance from the maxillary central incisors to the mandibular incisors. |
| Overjet (mm) | The amount of horizontal incisor overlap, measured from the labial surface of the mandibular incisors to the labial surface of the incisal edge of the maxillary incisors. |
| Curve of Spee (mm) | Measured by placing a metal ruler from the most posterior mandibular tooth to the incisors and measuring the deepest part of the arc. |
After data collection, the subjects were grouped according to their facial types based on their pretreatment cephalometric values for y-axis, mandibular plane angle, and Ricketts’ lower facial height. The normal-angle group was chosen to be those with a mandibular plane angle between 29° and 35°, a y-axis between 63° and 69°, and lower facial height between 44° and 50°. The high-angle group included those with a mandibular plane angle greater than 35°, a y-axis greater than 69°, and lower facial height greater than 50°. The low-angle group consisted of those with a mandibular plane angle less than 29°, a y-axis less than 63°, and lower facial height less than 44°. It was arbitrarily decided that at least 2 of 3 of these variables were required to determine facial type. We identified 28 normal-angle, 16 low-angle, and 16 high-angle subjects ( Table II ).
Statistical analysis
A mixed effects model (analysis of variance) was used to determine whether there were differences between the changes in the groups with time. Variance analysis was then followed by pair-wise bivariate contrasts in the form of t tests if a significant difference was found. The level of significance was set at P = 0.05 for all statistical analyses. To determine the reproducibility of the data, Dahlberg’s formula was used. The method error was calculated from the equation: <SPAN role=presentation tabIndex=0 id=MathJax-Element-1-Frame class=MathJax style="POSITION: relative" data-mathml='ME=∑d2nx2′>ME=∑d2nx2−−−−√ME=∑d2nx2
M E = ∑ d 2 n x 2
where d was the difference between duplicated measurements and n was the number of replications.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


