Introduction
Enamel decalcification during orthodontic treatment is a persistent problem. Resin-based sealants have been developed to protect enamel from decalcification. The purpose of this in-vivo study was to compare the effect of a fluoride-releasing filled enamel sealant with that of an unfilled nonfluoride control.
Methods
A total of 177 teeth in 18 patients were evaluated over a period of 12 to18 months. A split-mouth design was used; half the teeth were treated with the fluoride-releasing sealant (Pro Seal, Reliance Orthodontic Products, Itasca, Ill), and the contralateral teeth received the control (Transbond MIP, 3M Unitek, Monrovia, Calif). The teeth were photographed before (T1) and after (T2) treatment. A panel of 12 orthodontic faculty and residents evaluated the photographs for decalcification on a graded scale.
Results
Sixty-nine percent of the teeth treated with Pro Seal showed progressive decalcification from T1 to T2 vs 72% of those treated with Transbond MIP. In the comparison of the contralateral paired teeth, there was a small average net disadvantage of –0.06 of a tooth per patient (95% CI, –0.97 to 0.85) for Pro Seal compared with Transbond MIP. That difference of 0.06 of a tooth is neither statistically significant ( P = 0.90) nor clinically important.
Conclusions
The 2 products tested were equivalent in their inhibition of decalcification during orthodontic treatment. The additional time and expense of using the fluoride-releasing sealant to prevent decalcification does not appear to be justified.
Enamel decalcification, or the formation of white spot lesions, during orthodontic treatment has been a persistent problem, with many attempts made to minimize or eliminate damage. Several resin-based sealants have been used to protect the enamel during treatment. Some sealants have shown promise in protecting the enamel to a clinically significant degree. Loss of sealant material during treatment from toothbrushing and masticatory abrasion is an important clinical problem. It is a challenging aspect of product design for manufacturers. Manufacturers have attempted to increase the strength and resistance to abrasion by adding filler materials to resin-based sealants. To minimize decalcification during orthodontic treatment, fluoride-containing particles have been included in resin sealants. The ability of a product to withstand abrasion and maintain clinical efficacy is the ultimate goal if the product is to have significant utility in clinical orthodontic practice. Although several studies were designed to evaluate sealants of varying formulations, in-vivo approaches to evaluating the efficacy of these sealants have been limited.
Pro Seal (Reliance Orthodontic Products, Itasca, Ill) is a fluoride-releasing filled-resin sealant that is purported to protect enamel during orthodontic treatment and remain intact without the need for reapplication.
Several in-vitro studies have been designed to study decalcification, including several that specifically assessed Pro Seal. Protocols that evaluated demineralization after simulated brushing and acidulated cycling, such as those described by Buren et al and Hu and Featherstone, found Pro Seal to be more effective at reducing demineralization compared with both untreated controls and products containing either unfilled resin or fluoride. This prospective, in-vivo study was designed to compare Pro Seal with a control in a time frame approaching typical orthodontic treatment. The principal objective was to assess its efficacy in preventing decalcification.
Material and methods
Twenty-two consecutively treated patients (13 female, 9 male; age range, 10-40 years; mean age, 17.6; median, 15; mode, 15) who came for comprehensive full 1-phase orthodontic treatment at Albert Einstein Medical Center (Philadelphia, Pa) were selected for this study; informed consent and institutional review board approval were obtained before each patient’s enrollment. Eighteen of the 22 patients were included in the final evaluation. The 4 patients who were lost to follow-up were not included in the analyses. Three patients did not return to the clinic for evaluation in the final months of the study, and 1 patient requested early termination of orthodontic treatment. Patients who did not return for follow-up evaluation accounted for 47 teeth; 19 more teeth were excluded because they were debonded or purposely repositioned during the study before the final evaluation. This resulted in 177 teeth remaining to be evaluated.
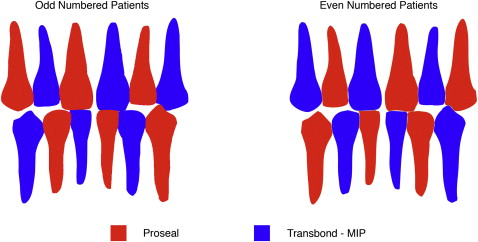
The patients served as their own controls via a split-mouth study design. Pro Seal and Transbond MIP (3M Unitek, Monrovia, Calif) were applied to the entire facial surface of alternating teeth in both arches from canine to canine (maximum of 12 teeth) ( Fig 1 ). Teeth that were unerupted, missing, or not planned to be bonded during treatment on the initial bonding date were excluded from the study. Teeth with white spot lesions at the start of treatment were not excluded from the study because we wanted to evaluate the net change in decalcification. The manufacturer’s handling protocols were followed for each material. All teeth were pumiced before etching, washing, air drying, and resin application. Pro Seal required curing with a halogen-type curing light source for 20 seconds (Ortholux XT, 400-500 nm, 3M Unitek). Transbond MIP was air dried according to the manufacturer’s instructions. The brackets were bonded by 1 clinician (C.L.) with Transbond composite bonding cement. The patients were then monitored and reevaluated for decalcification after an average of 14.6 months (SD, ± 2 months; range, 12-18 months).
As noted above, 18 of the 22 patients enrolled in the study were included in the final evaluation. A total of 177 teeth completed the study from the 243 bonded.
Photographic evaluation was used to determine levels of decalcification. The protocols for evaluation of decalcification by photographic methods were adapted from previous studies by Wenderoth et al, Gaworski et al, and Le et al. Pretreatment (T1) and 12- to 18-month (T2) evaluation photographs (with brackets debonded) were taken with a digital camera (Stylus 710, Olympus, Center Valley, Pa) in super-macro mode without flash. After debonding and photographing, the brackets were replaced for patients who were continuing treatment. The compiled photographs were randomized to conceal whether they were taken at T1 or T2. The evaluators were blinded as to which product had been used on the teeth they evaluated. Twelve orthodontic professionals (faculty and residents) evaluated all photographs and scored them based on a 3-point scale: 0, no decalcification; 1, slight decalcification; 2, significant decalcification.
Statistical analysis
Decalcification was assessed at T1 and T2 by using the average decalcification level provided by the 12 raters for each tooth. By comparing the changes in decalcification in a pair of contralateral teeth (1 treated with Pro Seal and the other with Transbond MIP), we determined which treatment had superior decalcification performance for that pair. We computed the number of contralateral pairs of teeth with better decalcification performance for Pro Seal minus the corresponding number for Transbond MIP separately for each patient. If that difference was positive, it was called a net treatment advantage for Pro Seal in that patient. If it was negative, that difference indicated a net disadvantage for Pro Seal (compared with Transbond). The average of the net treatment advantage (or disadvantage) over all patients and the corresponding 95% confidence intervals were used to provide the statistical comparison of the decalcification performance of the 2 treatments. This analysis is equivalent to the confidence interval for a paired t test. We used Fisher’s exact test to compare the percentages of patients with a net advantage on the two treatments. All statistical analyses were performed with a statistical software program (version 10, Stata, College Station, Tex).
Results
Of the maxillary and mandibular anterior teeth, decalcification worsened in 60 of 87 teeth (69%) treated with Pro Seal and in 65 of 90 teeth (72%) treated with Transbond MIP. The results are given in the Table .
| Material | Worsened | Did not worsen | Total teeth |
|---|---|---|---|
| Pro Seal | 60 (69%) | 27 (31%) | 87 (100%) |
| Transbond MIP | 65 (72%) | 25 (28%) | 90 (100%) |
Of the 18 patients, 4 (22%) had a net advantage in mitigating decalcification with Pro Seal over Transbond MIP but 8 patients (44%) had a net disadvantage for Pro Seal ( Fig 2 ) ( P = 0.29). Thus, Pro Seal did not help a larger percentage of patients mitigate decalcification than Transbond MIP. Notice that 3 patients had a large net advantage for Pro Seal (> 3 pairs of teeth).
To ensure a fair comparison, we now provide an additional analysis which uses the size of the net advantage for each patient in comparing Pro Seal to Transbond MIP ( Fig 2 ). Changes in decalcification levels were computed and compared in pairs of contralateral teeth, 1 treated with Pro Seal and the other with Transbond MIP. When we computed the number of contralateral pairs of teeth with changes corresponding to better decalcification performance for Pro Seal minus the corresponding number for Transbond MIP, 1 patient had better decalcification performance for Pro Seal (than Transbond MIP) in 5 contralateral pairs but worse changes in 1 pair. This yielded a net of 4 more pairs of contralateral teeth in which the Pro Seal tooth did better overall in that patient ( Fig 2 , top left). We called this a 4-tooth net advantage for Pro Seal. A 3-tooth net advantage for Pro Seal was found in 2 patients (indicated by the 2 dots on the second row from the top of Fig 2 ), and a 1-tooth net advantage for Pro Seal occurred in 1 patient. In 6 patients, Pro Seal and Transbond MIP had the same numbers of pairs with advantages for each product (in changes in decalcification level). This is illustrated by the 6 dots (patients) on the 0 difference horizontal line in Figure 2 . On the other hand, all patients below that line had a net disadvantage for Pro Seal compared with Transbond. A 1-tooth net disadvantage for Pro Seal was found in 5 patients (5 dots on the –1 row in Fig 2 ). A 2-tooth net disadvantage for Pro Seal occurred in 2 patients. Finally, 1 patient had a 3-tooth net disadvantage for Pro Seal compared with Transbond MIP. Overall, on average, there was a small net disadvantage of –0.06 of a tooth per patient (95% CI, –0.97 to 0.85) for Pro Seal compared with Transbond MIP. That average difference of 0.06 of a tooth was neither statistically significant ( P = 0.90) nor clinically important.




