Introduction
The aim of the study was to evaluate the dentoskeletal effects of the zygoma-gear appliance used for unilateral maxillary molar distalization in patients with Class II subdivision malocclusion.
Methods
This prospective clinical study consisted of 21 patients (9 boys, 12 girls; mean age, 15.68 ± 2.18 years) with unilateral Class II malocclusion treated using the unilateral zygoma-gear appliance supported by a zygomatic miniplate inserted on the Class II malocclusion side. The dentoskeletal effects of the system were evaluated using cephalometric lateral and panoramic films with a paired t test.
Results
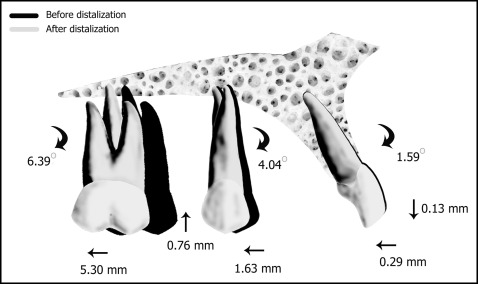
The mean amount of distalization for the maxillary first molar was found to be 5.31 ± 2.46 mm ( P <0.001) in 0.45 ± 0.12 years, showing an amount of 0.98 mm of distalization per month. It was also accompanied by a slight intrusion (0.76 ± 2.85 mm; P >0.05) and distal tipping (6.39° ± 5.39°; P <0.001) of the maxillary molars. The maxillary premolar also spontaneously moved distally 1.63 ± 1.90 mm ( P <0.01) with distal tipping (4.05° ± 3.47°; P <0.001). Moreover, the inclination of the maxillary incisors and overjet were decreased (−1.59° ± 1.45°, P <0.001; and −0.29 ± 0.63 mm, P <0.05; respectively) showing no anchorage loss. No statistically significant changes were found for the skeletal and soft tissue measurements ( P >0.05).
Conclusions
The zygoma-gear appliance system is an effective method for unilateral maxillary molar distalization.
Highlights
- •
The zygoma-gear appliance was used for unilateral molar distalization in 22 patients.
- •
Mean first molar distalization was 5.31 ± 2.46 mm (0.98 mm per month).
- •
Maxillary incisor inclination and overjet were decreased, with no anchorage loss.
The traditional treatment of a unilateral Class II molar relationship with asymmetry in the maxillary arch is the use of asymmetric extraoral traction in patients to be treated without tooth extractions. Although this method gives successful results in cooperating patients, the lack of cooperation results in anchorage loss and unsatisfactory treatment results. In addition, it has been shown that such a force delivery system unavoidably contains a lateral component that might cause posterior crossbite.
To eliminate the disadvantages of extraoral appliances, many clinicians use different intraoral distalization appliances to move the maxillary molars distally. Although appliances such as the distal jet, pendulum first class, Jones jig, Keles slider, Wilson arches, and Hilgers were reported to be successful for distalization of the maxillary molars, distal movement occurred mainly by tipping and rotation of the crowns. In addition, the anchorage loss characterized by maxillary premolar mesialization, maxillary incisor protrusion, and overjet increase was reported to be unavoidable with those appliances. To overcome the anchorage loss problems, clinicians described the use of intraosseous screws, onplants, and osseointegrated implants and plates. However, the distalization period is delayed owing to the waiting period of 3 to 6 months for the palatal implants to achieve osseointegration. In addition, the bulky acrylic Nance appliance used behind the maxillary incisors might be a problem during retraction of the anterior teeth.
Recently, a new approach called the zygoma-gear appliance (ZGA; GAC International, Bohemia, NY) was described for the distalization of the maxillary molars. It was found to be effective for bilateral molar distalization. However, only a few case reports have evaluated its efficiency for unilateral maxillary molar distalization.
The aim of this prospective clinical study was to evaluate the dentoskeletal effects of the ZGA when used for unilateral maxillary molar distalization.
Material and methods
The study was approved by the local ethics committee of the Karadeniz Technical University in Trabzon, Turkey. In addition, the patients or their parents had signed an informed consent form allowing us to use their data for scientific purposes.
Sample size for the study was calculated based on a significance level of 0.05 and a power of 90% to detect a clinically meaningful difference of 0.6 mm (±0.8 mm) for maxillary molar distalization in a month. Power analysis showed that 19 subjects were required. To compensate for possible dropouts during the distalization and increase the power of the study, we decided to include more patients.
The inclusion criteria for the study were (1) skeletal Class I (0° < ANB < 4°) ; (2) normal or low-angle growth pattern (SN-MP <38°) ; (3) dental Class II subdivision relationship and need for nonextraction treatment and unilateral maxillary molar distalization of at least 3 mm; (4) permanent dentition with erupted maxillary second molars; (5) presence of all teeth including third molars; (6) normal overbite (0-3 mm) ; and (7) good oral hygiene. The exclusion criteria were a skeletal Class II or Class III relationship, high-angle vertical growth pattern, and previous orthodontic treatment. According to those criteria, 22 patients were included to the study after they or their parents were informed about the study protocol and the ZGA system.
A titanium miniplate (Multipurpose Anchor MPI 1000; Tasarim Med, Istanbul, Turkey) with 3 holes was placed at the zygomatic buttress and fixed by 3 titanium bone screws (length, 5.0 mm; diameter, 2.0 mm) under local anesthesia ( Fig 1 ). The inner bow of the conventional face-bow was modified to include 2 U-bends in front of the maxillary molars and 2 hooks soldered at the lateral tooth region. Then, it was adjusted to the headgear tube with its anterior part about 3 mm away from the anterior teeth. Three weeks after the surgery, a force of about 350 g with a closed-coil spring (GAC International) was applied on the side requiring distalization, and the maxillary molar tube and the hook at the lateral region were ligated on the side not requiring distalization ( Fig 2 ). The force was checked and standardized with a gram-force gauge (Correx; Haag-Streit, Koeniz, Switzerland) at 4-week intervals, and the ZGA was adjusted by widening the U-bends with a plier to move away it from the anterior teeth if needed. The distalization was considered adequate when a super-Class I relationship was achieved. After the distalization was completed, further orthodontic treatment was done using the fixed appliances ( Fig 3 ).



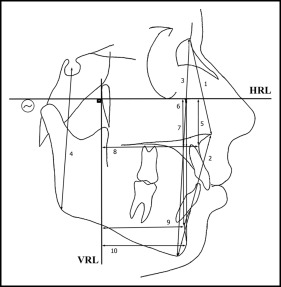
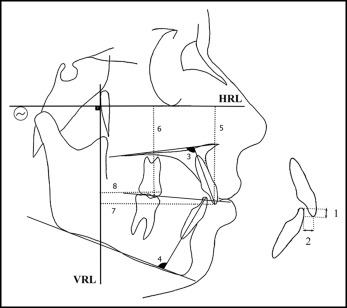
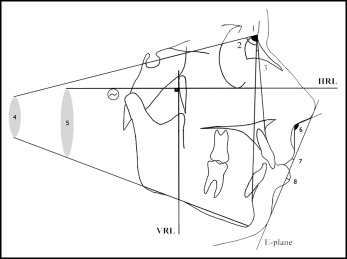
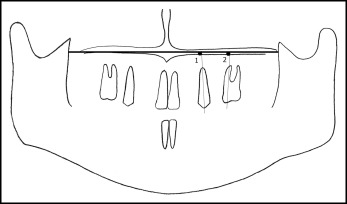
Cephalometric films were taken in a standard position with the same cephalostat (Veraviewepocs; Morita, Kyoto, Japan) by the same technician just before (within 2 weeks, T1) and after (within a week, T2) the distalization. The subjects were requested to keep their teeth in centric occlusion during the exposure, and special attention was given to ensure that the lips were at rest. The pterygoid vertical and Frankfort horizontal planes were used as vertical and horizontal reference lines. The pterygoid vertical plane was the perpendicular line from pterygoid to the Frankfort horizontal plane. Eight angular and 18 linear measurements were performed to evaluate the skeletal, dentoalveolar, and soft tissue effects using cephalometric lateral films ( Figs 4, 5, and 6 ) with NemoCeph software (NX 2006; Nemo Tec, Madrid, Spain). In addition, changes in the angulation of the maxillary first premolar and molar in the distalization side were assessed using panoramic films ( Fig 7 ). After the calibration, all radiographs were traced by an experienced orthodontist (D.K.) with a random queue so that the researcher was blinded.
Statistical analysis
The Mann-Whitney U test was used to compare the sexes for the changes of each parameter. Since no significant sex difference was found ( P >0.05), the data were pooled for further statistical evaluations. The changes observed for each parameter were evaluated using a paired t test because the Shapiro-Wilk test showed normally distributed variables ( P >0.05).
To examine the errors associated with digitizing and measurements, 15 radiographs were selected randomly, and measurements were repeated 3 weeks after the first examination by the same author (D.K.). The Houston test, performed to analyze the reliability of the measurements, confirmed the reliability, since the values were between 0.891 and 0.943. All statistical analyses were performed using the SPSS software package (SPSS for Windows 98, version 10.0; SPSS, Chicago, Ill), and the significance level was set at P <0.05.
Results
One patient was excluded from the study because of an infection of the miniplate, and none of the remaining patients had problems of mobility, breakage, discomfort, and hygiene during the distalization period. Finally, 21 patients (male/female, 9/12; mean age, 15.68 ± 2.18 years) were analyzed at the end of the distalization period. No sex differences were found for the chronologic ages and distalization periods ( P >0.05; Table I ).
| Mean age (y) ∗ | Distalization period (y) ∗ | |
|---|---|---|
| Boys (n = 9) | 16.39 ± 1.57 | 0.51 ± 0.11 |
| Girls (n = 12) | 15.24 ± 2.43 | 0.41 ± 0.12 |
| Total (n = 21) | 15.68 ± 2.18 | 0.45 ± 0.12 |
∗ No significant difference between the sexes according to the Mann-Whitney U test.
The mean amount of distalization for the maxillary first molar was found to be 5.31 ± 2.46 mm ( P <0.001) in 0.45 ± 0.12 years, showing a 0.98-mm distalization rate per month. The distalization of maxillary first molar was accompanied by a slight intrusion (0.76 ± 2.85 mm; P >0.05) and distal tipping (6.39° ± 5.39°; P <0.001). The maxillary premolar also spontaneously moved distally 1.63 ± 1.90 mm ( P <0.01) with distal tipping (4.05° ± 3.47°; P <0.001). Moreover, the inclination of the maxillary incisors and overjet were decreased (1.59° ± 1.45°, P <0.001, and 0.29 ± 0.63 mm, P <0.05; respectively) ( Fig 8 ). On the other hand, no statistically significant changes were found for the skeletal and soft tissue measurements ( Table II ).
| Measurement | Before distalization | After distalization | Mean difference | SE | P |
|---|---|---|---|---|---|
| Skeletal | |||||
| SNA (°) | 79.80 ± 4.04 | 79.57 ± 3.88 | −0.23 ± 0.70 | 0.15 | NS |
| SNB (°) | 76.57 ± 3.52 | 76.42 ± 3.52 | −0.14 ± 0.85 | 0.18 | NS |
| ANB (°) | 3.23 ± 1.54 | 3.14 ± 1.68 | −0.09 ± 1.04 | 0.22 | NS |
| FMA (°) | 22.00 ± 6.99 | 21.80 ± 7.30 | −0.19 ± 1.63 | 0.35 | NS |
| SN-MP (°) | 31.95 ± 7.49 | 31.52 ± 7.75 | −0.42 ± 0.97 | 0.21 | NS |
| MP-PP (°) | 22.95 ± 7.63 | 22.71 ± 7.32 | −0.23 ± 1.17 | 0.25 | NS |
| N-ANS (mm) | 51.33 ± 3.85 | 51.57 ± 3.90 | 0,23 ± 1.48 | 0.32 | NS |
| ANS-Me (mm) | 62.19 ± 7.03 | 62.00 ± 6.37 | −0.19 ± 1.99 | 0.43 | NS |
| N-Me (mm) | 113.52 ± 9.19 | 113.57 ± 8.89 | 0,04 ± 2.88 | 0.63 | NS |
| S-Go (mm) | 75.47 ± 9.21 | 76.14 ± 9.77 | 0.66 ± 3.63 | 0.79 | NS |
| VRL-A (mm) | 49.97 ± 3.08 | 49.61 ± 3.02 | −0.35 ± 1.38 | 0.30 | NS |
| VRL-B (mm) | 44.27 ± 4.84 | 44.33 ± 4.59 | 0.06 ± 1.25 | 0.27 | NS |
| VRL-Pg (mm) | 45.78 ± 6.24 | 46.14 ± 6.24 | 0.36 ± 1.56 | 0.34 | NS |
| HRL-A (mm) | 28.80 ± 3.51 | 28.92 ± 4.01 | 0.12 ± 2.62 | 0.57 | NS |
| HRL-B (mm) | 63.97 ± 5.71 | 64.01 ± 6.70 | 0.03 ± 2.38 | 0.52 | NS |
| HRL-Pog (mm) | 76.40 ± 7.11 | 76.45 ± 8.00 | 0.04 ± 3.79 | 0.82 | NS |
| Dentoalveolar | |||||
| U1-PP (°) | 111.45 ± 8.14 | 109.85 ± 7.95 | −1.59 ± 1.45 | 0.31 | 0.000 ‡ |
| L1-MP (°) | 95.19 ± 8.09 | 95.00 ± 8.30 | −0.19 ± 0.67 | 0.14 | NS |
| U4-PP (°) | 88.47 ± 6.53 | 92.52 ± 5.80 | 4.04 ± 3.46 | 0.84 | 0.000 ‡ |
| U6-PP (°) | 97.18 ± 6.17 | 103.58 ± 7.07 | 6.39 ± 5.38 | 1.3 | 0.000 ‡ |
| Overjet (mm) | 3.65 ± 0.94 | 3.36 ± 1.14 | −0.29 ± 0.62 | 0.13 | 0.047 ∗ |
| Overbite (mm) | 2.77 ± 1.07 | 3.00 ± 1.33 | 0.23 ± 0.55 | 0.12 | NS |
| VRL-U1 (mm) | 53.30 ± 3.98 | 52.80 ± 3.44 | −0.50 ± 1.72 | 0.37 | NS |
| VRL-U4 (mm) | 38.06 ± 3.83 | 36.43 ± 3.37 | −1.63 ± 1.90 | 0.41 | 0.001 † |
| VRL-U6 (mm) | 27.30 ± 4.00 | 21.99 ± 3.18 | −5.30 ± 2.45 | 0.53 | 0.000 ‡ |
| HRL-U1 (mm) | 49.60 ± 4.88 | 49.74 ± 5.91 | 0.13 ± 3.03 | 0.66 | NS |
| HRL-U6 (mm) | 45.50 ± 4.70 | 44.74 ± 4.94 | −0.76 ± 2.83 | 0.61 | NS |
| Soft tissue | |||||
| Nasolabial (°) | 110.53 ± 9.03 | 111.59 ± 10.16 | 1.06 ± 6.69 | 1.46 | NS |
| UL-E (mm) | −3.28 ± 1.92 | −3.33 ± 1.74 | −0.04 ± 1.20 | 0.26 | NS |
| LL-E (mm) | −1.76 ± 1.89 | −1.42 ± 1.98 | 0.33 ± 1.19 | 0.26 | NS |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


