Introduction
We evaluated the effects of screw placement angle on the frequency of root contact and the effects of root contact on screw stability, comparing self-drilling and self-tapping methods.
Methods
In total, 80 patients with 142 screws (diameter, 1.6 mm; length, 8.0 mm) were included. Cone-beam computed tomography images were taken. Cortical bone thickness, interroot distance, shortest distance between the screw and adjacent tooth root, and screw placement angle were measured.
Results
The success rates of the screws were 91.5% for the self-drilling method and 94.4% for the self-tapping method ( P >0.05). The self-drilling screws tended to contact the distal tooth roots in the right maxilla. In the self-drilling method, the failure rate was significantly higher in the root contact group than in the no-contact group ( P <0.05).
Conclusions
The success rate was not significantly different between the self-drilling and the self-tapping methods in the maxilla. Avoidance of tooth root contact may improve the success rate more in the self-drilling method than in the self-tapping method.
Highlights
- •
The self-drilling screws tended to contact distal tooth roots in the right maxilla.
- •
The self-drilling failure rate was higher in the root contact group than in the no-contact group.
- •
Success rates were not significantly different between self-drilling and self-tapping methods.
- •
Avoidance of tooth root contact may improve the success rate more in the self-drilling method.
In clinical orthodontics, for some patients a sufficient treatment outcome cannot be achieved because reciprocal tooth movement occurs. Thus, anchorage control becomes important and can affect treatment outcomes considerably. Intraoral devices or extraoral anchorages, such as lingual arch appliances or headgear, have been used in clinics. The absolute anchorage at the least anteroposterior direction would be achieved using headgear constantly as instructed, but the treatment results depend on the patient’s cooperation.
Orthodontic anchor screws are frequently used as an absolute anchorage device because the screws can be placed readily at various sites such as in alveolar bone or palatal bone with minimal surgical invasiveness. Anchorage by a screw enables more effective treatment with minimum anchorage loss and greater anterior distal movement than conventional anchorage devices such as headgear. These positive treatment outcomes can be obtained even without the patient’s cooperation. Upadhyay et al and Nagaraj et al reported positive treatment outcomes using screws for retraction and depression of anterior teeth, and protraction of molars.
However, several researchers have reported loosening of screws during orthodontic treatment. Papadopoulos et al reported that the success rate of the screw was 87.7% in a meta-analysis. A screw is typically placed in small gaps between adjacent teeth, possibly inducing root contact that might contribute to the failure of the screw. Kuroda et al and Chen et al reported that root proximity contributed significantly to screw failure. Kim and Kim reported that screws in contact with the adjacent tooth root may cause or worsen root external resorption. Papageorgiou et al also performed a meta-analysis to summarize current knowledge regarding the failure rates of screws and to identify significant risk factors affecting failure rates. They reported that the failure rate of screws was 13.5%, and screws with tooth root contact had a failure rate 3 times as large as those with no contact. Thus, tooth root contact by the screw should be avoided.
Two methods are used for the placement of screws: the self-tapping method, requiring the preparation of a pilot hole before insertion, and the self-drilling method, which enables the screw to be inserted without predrilling. Tachibana et al recommended using the self-drilling method or the self-tapping method, the latter by drilling a pilot hole of 1.0 mm in diameter when a screw of 1.6 mm in diameter was placed on the maxillary buccal alveolar bone. Son et al compared the 2 methods to identify the influence of root contact on the stability of the screw, and they reported that the self-drilling method showed significantly higher mobility than did the self-tapping method. However, screw mobility does not necessarily result in screw failure. Thus, screw stability should be correctly evaluated using the survival or success rate of the screw.
Deguchi et al suggested that the inclined screw might increase apparent cortical bone thickness and stability, and Inaba showed that the mobility of the inclined screw to the bone surface was significantly less than when the screw was placed perpendicularly. Deguchi et al also stated that a screw inclined to the bone surface is less likely to cause root contact for a shallow horizontal impaction depth, and they reported that the difference in the screw placement angle between the self-drilling and self-tapping methods may influence the frequency of root contact. However, the relationship between the placement angle of the screw and tooth root contact is not sufficiently clear.
In this study, we evaluated the effects of screw placement angle on frequency of root contact and the effects of root contact on screw success rate in the maxillary buccal alveolar bone, comparing the self-drilling and self-tapping methods. In this study, we hypothesized that the placement method of the screw would have no influence on screw placement angle, the frequency of tooth root contact, and the success and failure rates of screws in the maxilla. This study was intended to create evidence for clinicians regarding selection of placement methods for orthodontic anchor screws.
Material and methods
In total, 80 orthodontic patients who received screws in 2012 and 2013 at Nihon Dental Hospital in Japan were included (26 men, 54 women; average age, 23.2 ± 8.0 years). One hundred forty-two screws (71 self-drilling method; 71 self-tapping method) were investigated. We excluded patients who had second premolar extractions or in whom a screw penetrated to the maxillary sinus. All screws were placed at the beginning of treatment. This study was approved by the ethics committee of Nihon University. The data presented here were derived from patients who consented to participate in the study before surgical placement of the screws.
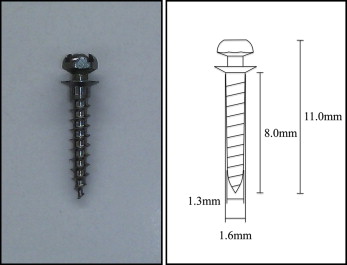
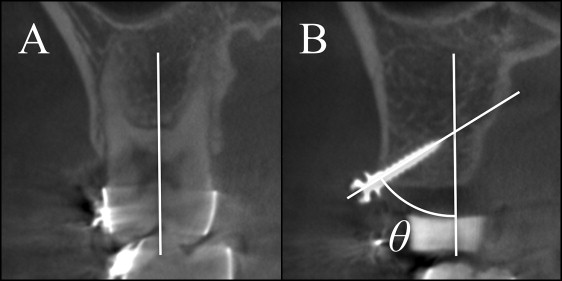
Orthodontic anchor screws (ISA; Biodent, Tokyo, Japan; Fig 1 ), 1.6 mm in diameter and 8.0 mm in length, were used. The screws were placed in the maxilla using the self-drilling method or the self-tapping method according to the study of Tachibana et al. In the self-drilling method, after administering local anesthesia, the screw was placed without predrilling. In the self-tapping method, a pilot hole (diameter, 1.0 mm; Fig 2 ) was drilled using a bone drill, with saline solution flow, before placing the screws. Placement position of the screw was fixed at the height of 6 mm on the gingival side from a bracket slot just under the contact point of the second premolar and the first molar. The screw made a vertical placement angle of 60° to the bone surface; this inclined the screw head to the crown side and made a horizontal placement angle of the perpendicular to the bone surface. Placement of the screws was performed by 2 clinicians (M.M., Y.U.) with clinical experience of 10 years or more and with screw placement experience of 3 years or more; placement procedures were not different between the clinicians. Placement methods of self-drilling or self-tapping were randomly assigned.

Screws used for more than 6 months were considered successes, and screws that were lost naturally or removed owing to mobility were considered failures. Screws that contacted the tooth root were removed and defined as failures when the patient experienced clinical manifestations such as pain and discomfort or when there was mobility of the screw. According to Shigeeda, screws that contacted the tooth root without root injury were not considered failures and were kept under observation.
After placement of a screw, cone-beam computed tomography (CBCT) (3D Accuitomo; J. Morita, Kyoto, Japan) with a voxel size of 0.125 × 0.125 × 0.125 mm, an x-ray tube voltage of 80 kV, and current of 5.5 mA was used for diagnostic imaging of the area around the site. The cortical bone thickness, the interroot distance, the shortest distance between the screw and the adjacent tooth root, and the screw placement angle were measured using a 3-dimensional viewer program (One Volume Viewer, version 1.6.1.13; J. Morita).
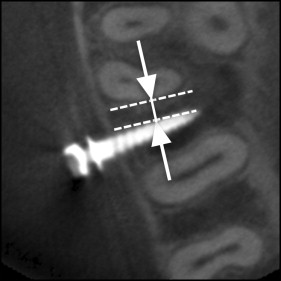
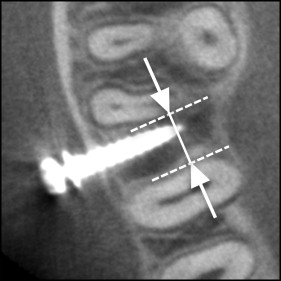
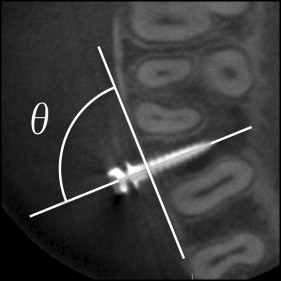
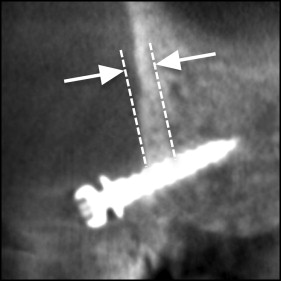
In the CBCT imaging, 3 horizontal cross sections were defined parallel to the occlusal plane, corresponding to the height of the placement position at the bone surface, the tip, and the middle of the impacted part of the screw. On these 3 sections, the mesial and distal distances between the screw and the adjacent tooth root were measured ( Fig 3 ). The nearest root of the adjacent teeth and the shortest distance from the screw were recorded as the shortest distance between the screw and root (shortest screw-root distance); a shortest screw-root distance of 0 mm indicated root contact. The interroot distance was measured at the height of the placement point of the screw ( Fig 4 ). In an occlusal view, the angle of the distal side between the major axis of the screw and the buccal cortical bone surface was measured as the horizontal screw placement angle ( Fig 5 ). The vertical cross section in the CBCT imaging was fixed perpendicular to the occlusal plane and fixed to the major axis of the screw ( Fig 6 ). In this vertical cross section, cortical bone thickness was measured at the nearest site from the screw. The angle from the major axis of the screw to the tooth axis of the first molar ( Fig 7 , A ) was measured on the vertical cross section as the vertical screw placement angle ( Fig 7 , B ).
To evaluate intraexaminer errors, we randomly selected CBCT images of 10 patients and remeasured all items 1 month after the initial measurements.
Statistical analysis
The chi-square or Fisher exact test was used to assess the difference between the self-drilling and self-tapping methods to evaluate the relationship between root contact and screw failure. A binomial test was used to evaluate the rate of tooth root contact between the mesial and distal teeth. For these analyses, SPSS software (version 16.0; SPSS Japan, Tokyo, Japan) was used. P values less than 0.05 were considered to indicate statistical significance.
Results
The measurement error test showed no significant difference in any item between the first and second measurements from the CBCT images. Significant differences between the 2 clinicians were not found in any items.
The success rates of the screws were 91.5% with the self-drilling method and 94.4% with the self-tapping method ( P >0.05; Table I ).
| n | Success rate (%) | P value | |
|---|---|---|---|
| Self-drilling | 71 | 91.5 | |
| Self-tapping | 71 | 94.4 | 0.512 |
The cortical bone thickness and the interroot distance showed no significant difference between the self-drilling and self-tapping methods. However, the shortest screw-root distance was significantly less in the self-drilling method ( P <0.05; Table II ). In the horizontal cross section, the angle of the screw was more perpendicular to the bone surface in the self drilling method ( P <0.05). In the vertical cross section, the angle tended to be more inclined in the self-tapping method ( P <0.05; Table III ).
| Cortical bone thickness | Interroot distance | Screw-root distance | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Mean (mm) | SD | P value | Mean (mm) | SD | P value | Mean (mm) | SD | P value | |
| Self-drilling | 1.02 | 0.39 | 2.66 | 0.62 | 0.61 | 0.44 | |||
| 0.650 | 0.149 | 0.039 ∗ | |||||||
| Self-tapping | 1.05 | 0.25 | 2.82 | 0.70 | 0.79 | 0.57 | |||
| Horizontal placement angle | Vertical placement angle | |||||
|---|---|---|---|---|---|---|
| Mean (°) | SD | P value | Mean (°) | SD | P value | |
| Self-drilling | ||||||
| Right | 86.75 | 6.57 | – | 54.42 | 13.04 | – |
| Left | 87.16 | 8.22 | – | 51.75 | 13.24 | – |
| Total | 86.95 | 7.38 | – | 53.11 | 13.11 | – |
| Self-tapping | ||||||
| Right | 85.82 | 7.27 | 0.046 ∗ | 49.12 | 17.31 | 0.021 ∗ |
| Left | 81.45 | 15.23 | – | 44.99 | 18.33 | – |
| Total | 83.54 | 12.21 | – | 46.97 | 17.84 | – |
The rates of adjacent tooth root contact were 21.1% in the self-drilling method and 19.7% in the self-tapping method, with no significant difference. The rates of tooth root contact were 22.9% on the right side and 18.1% on the left side, with no significant difference. A significant difference was observed between the distal and mesial sites in the right maxilla with the self-drilling method, and the self-drilling screws tended to contact the distal tooth root ( P <0.01; Table IV ). The failure rate was significantly higher in the contact group than in the no-contact group ( P <0.05; Table V ).



