Introduction
The aim of this prospective clinical trial was to assess the effects of varying force directions on the dynamic measurement of natural head position and orofacial airway dimensions of Class III patients during maxillary orthopedic protraction compared with an untreated control group.
Methods
The conventional facemask group comprised 15 patients (8 girls, 7 boys; mean age, 9.6 ± 1.3 years), the modified facemask group comprised 15 patients (7 girls, 8 boys; mean age, 9.5 ± 1.5 years), and the control group comprised 15 subjects (7 girls, 8 boys; mean age, 9.8 ± 1.6 years). Natural head position measurements and cephalometric records were obtained from all subjects before and after treatment or the control period (approximately 1 year). An inclinometer and a portable data logger were used to collect the dynamic natural head position data. For statistical comparisons, paired samples t tests, analysis of variance (ANOVA), and post-hoc Tukey tests were used at the P <0.05 level.
Results
Both treatment groups showed statistically significant changes in the sagittal (pitch) measurements of natural head position and upper pharynx, aerial, and total area of airway measurements during the treatment period. In the control group, the only statistically significant change was an increased upper pharynx measurement ( P = 0.020). According to the intergroup comparisons, statistically significant natural head position differences were found in the conventional (6.4° flexion) and the modified (5.7° flexion) facemask groups when compared with the controls. The modified facemask group also showed significant changes in aerial ( P = 0.003) and total ( P <0.001) areas of the airway measurements compared with the control group. No statistically significant differences were observed between the 2 treatment groups.
Conclusions
These findings suggest that modified and conventional facemask therapy with expansion have significant cranial flexion effects on the dynamic measurements of natural head position. Additionally, the modified facemask procedure showed significant effects on the orofacial airway dimensions compared with the initial values and the values of the untreated controls.
Facemask and palatal expansion therapy has become a common technique for the correction of developing Class III malocclusions in recent years. Studies have documented that facemask treatment before adolescence produces an orthopedic effect to bring the maxilla forward (with counterclockwise rotation), often accompanied by a downward-backward rotation of the mandible and favorable dental changes for correction of reverse overjet and Class III malocclusion.
Counterclockwise rotation of the maxilla is a benefit in the treatment of low-angle, deepbite Class III patients, but it is not recommended in Class III patients with high-angle skeletal patterns and anterior open bites. To eliminate these undesired side effects, some investigators have applied the protraction force close to the center of resistance of the maxilla with a modified face-bow. Investigators showed that a modified facemask application method with a face-bow is an effective way to prevent counterclockwise rotation of the maxilla.
Profitt and Fields claimed that rapid maxillary expansion (RME) had to be done before protraction of the maxilla. Other studies in the literature support the concept that RME treatment releases the maxilla’s sutures with the surrounding bones and enhances the protraction procedure. RME can also cause a total increase in the nasal cavity’s volume, since its lateral walls are displaced apart. A possible hypothesis about the role of facemask and palatal expansion therapy in postural changes might be that the increased palatal diameter results in the consequent enlargement of the pharyngeal airway space. This enlargement leads to improvement in respiratory function and consequent flexion of the head on the cervical column with an increase of the cervical lordosis angle and a decrease of the craniocervical angulations.
Various methods can obtain natural head position. Some authors accept natural head position as the most relaxed position of the head when the subject is not guided by any outer reference (self-balanced position). Others believe that natural head position is the position of the head when the subject’s visual axis is parallel to the ground. Orhan and Goyenc produced natural head position by the “target on the mirror” technique with high reproducibility but stated that it was an unnatural, forced, and static position. In addition, natural head position is described not as a single angular measurement but as a small range of angles around the natural head position. Thus, this position is dynamic and should be recorded as such.
To our knowledge, the effects of modified and conventional facemask therapies with expansion on the dynamic measurements of natural head position and orofacial airway dimensions compared with a control group have not been studied. The aim of this prospective clinical trial was to assess the effects of varying force directions on natural head position and orofacial airway changes with maxillary orthopedic protraction compared with a control group. The null hypothesis assumed that there were no statistically significant changes in natural head position and orofacial airway dimensions after treatment with conventional and modified facemasks and expansion therapy compared with the controls.
Material and methods
This study was approved by the Regional Ethical Committee on Research of the Erciyes University in Turkey.
A power analysis established by G ∗ Power software (version 3.0.10; Franz Faul, Universität Kiel, Kiel, Germany), based on a 1:1 ratio between groups and a sample size of 15 patients, would give more than 75% power to detect significant differences with an effect size of 0.30 and α = 0.05 significance level.
Our sample consisted of the dynamic natural head position records of 45 Class III patients with maxillary retrusion. Patients who satisfied the following inclusion criteria were selected: (1) Class III molar relationship, (2) anterior crossbite or edge-to-edge incisal relationship, (3) ANB angle of 0° or less and nasion perpendicular to A-point of 2 mm or less, (4) no congenitally missing or extracted teeth, and (5) no deformity in the nasomaxillary complex.
Patients with craniofacial abnormality, psychosocial impairment, craniofacial anomaly, skeletal openbite, nasal allergic conditions, airway obstructions due to adenoids, or previous orthodontic treatment were excluded from the study.
The conventional facemask group comprised 15 patients (8 girls, 7 boys; mean age, 9.6 ± 1.3 years), the modified facemask group comprised 15 patients (7 girls, 8 boys; mean age, 9.5 ± 1.5 years), and the control group comprised 15 subjects (7 girls, 8 boys; mean age, 9.8 ± 1.6 years). Treatment times in group 1 were between 0.6 and 1.5 years (mean, 1.12 ± 0.24 years); treatment times in group 2 were between 0.7 and 1.7 years (mean,. 1.24 ± 0.4 years); and the observation period in the control group was between 0.5 and 1.6 years (mean, 0.97 ± 0.32 years).
To constitute the control group, dynamic records of natural head postition were taken with parental permission by obtaining informed consent from subjects or parents who did not accept treatment with an extraoral appliance at that time.
In the conventional facemask group, a facemask and a bonded full-coverage maxillary acrylic splint expander with vestibular hooks and heavy elastics (500 g, depending on the distance between the hooks of the expansion appliance and the facemask) were used for orthopedic therapy.
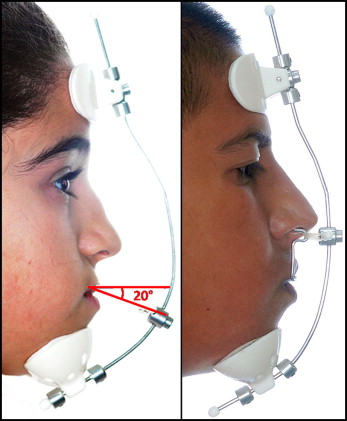
Elastics were connected bilaterally to the adjustable midline crossbow on the Petit-type facemask. The protraction elastics were applied to the vestibular hooks attached between the lateral incisors and the canines above 10 to 15 mm to the maxillary occlusion plane, with a downward and forward pull of 20° to prevent bite opening during maxillary protraction.
In the modified facemask group, a modified bonded RME appliance with full occlusal coverage, a specially designed facebow, a facemask, and heavy elastics (500 g, depending on the distance between the modified face-bow hook parts and the facemask) were used for orthopedic facemask therapy.
The bonded expansion appliance was modified by adding 2 tubes (Activator tubes; Dentaurum, Ispringen, Germany) on the buccal side of the acrylic in the premolar area. The purpose of these tubes was to accommodate the inner bows of the specially designed face-bow. The face-bow was constructed from an adjustable face-bow (standard stainless steel, G&H Wire, Franklin, Ind). The inner bows of the face-bow end went in the mouth with a special U-shape bend to enter the buccal tubes from the distal aspect and thus to retain it when an anterior pull was applied. The outer bow was bent upward at 90° to provide a point of force application at the level of the dentomaxillary center of resistance and also to apply the parallel forces in both sides ( Fig 1 ).
In both treatment groups, the midline expansion screw of the bonded maxillary expander was activated twice a day for the first week and once a day until the desired change in the transverse dimension was achieved. The patients were instructed to wear the facemask full time except during meals. We told the patients to keep track of their wearing time on the scorecard and to bring the card to each visit. The appliance was used in both treatment groups until a positive overjet was accomplished.
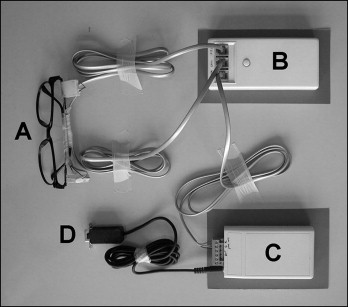
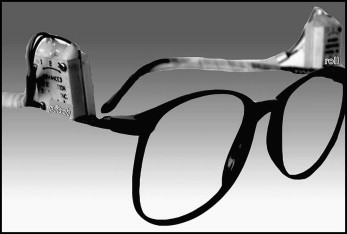
An inclinometer (linear tilt sensor, SX-070DLIN; Advanced Orientation Systems, Linden, NJ) and a portable data logger (XR440; Pace Scientific, Mooresville, NC) were used to collect the dynamic head posture data as described previously ( Figs 2 and 3 ). The inclinometers were placed on the eyeglasses’ arms, and cables from the inclinometers to the data logger were positioned not to obstruct the subject’s field of view. The right sensor was positioned parallel to the sagittal plane to determine changes in pitch, and the left sensor was positioned vertical to the sagittal plane to determine changes in roll. Analog data were used to record the dynamic changes in head position, and the data were stored in a portable data logger. The sampling rate of the data logger was adjusted to 1 sample every 2 seconds for a recording period of 6 minutes. The mean dynamic natural head position was calculated for each subject by using the collected data. When the head is tipped forward in the sagittal plane relative to the true vertical, the value measured by the inclinometers is positive. A negative value shows backward tipping.
The natural head position recordings were collected at the initial stage of the appliance placement and at the end of the facemask and palatal expansion therapy (mean treatment periods, 1.12 ± 0.24 years for the conventional facemask group and 1.24 ± 0.40 years for the modified facemask group). Natural head position records from the control group were taken approximately 1 year after the initial records, similar to the treatment group (mean observation period, 0.97 years ± 0.32 months). All natural head position recordings in the study groups were taken from the patients without the RME and facemask appliances in situ.
Lateral cephalometric radiographs were taken with a cephalometer (Ortoceph OC100, Instrumentarium, Tuusula, Finland). All subjects were positioned in the cephalostat with the sagittal plane at a right angle to the path of the x-rays, the Frankfort plane was parallel to the horizontal, the teeth were in centric occlusion, and the lips were lightly closed.
All radiographs were traced manually, and whole measurements were recorded by an author (A.Y.) and reviewed twice by another investigator (T.U.) for accurate landmark identification.
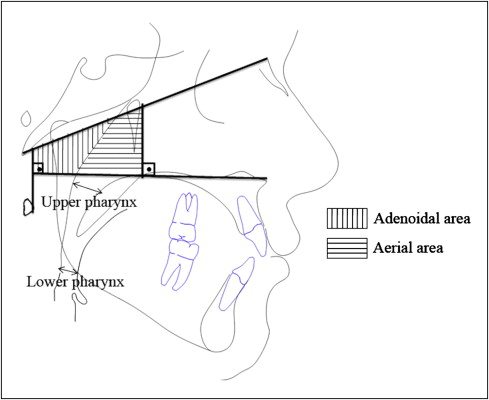
The following cephalometric measurements were made ( Fig 4 ): (1) McNamara’s upper pharynx dimension: the minimum distance between the upper soft palate and the nearest point on the posterior pharynx wall ; (2) McNamara’s lower pharynx dimension: the minimum distance between the point where the posterior tongue contour crosses the mandible and the nearest point on the posterior pharynx wall ; and (3) total, adenoidal, and aerial areas by using the method of Handelman and Osborne. This method takes as references the basion-nasion plane, the bispinal plane, and 2 perpendicular lines to the bispinal plane—1 crosses the more anterior point at the atlas vertebra and other crosses the posterior nasal spine. The resulting trapezoid is divided into 2 spaces (aerial and adenoid). Total area is the sum of adenoidal and aerial areas.
Statistical analysis
All statistical analyses were performed by using the Statistical Package for the Social Sciences (version 13.0 for Windows; SPSS, Chicago, Ill). The normality test of Shapiro-Wilks and the Levene variance homogeneity were applied to the data. The data were distributed normally, and there was homogeneity of variance between the groups. Descriptive statistics were given as mean and standard deviation. Intragroup comparisons were evaluated by using the paired samples t test, and intergroup changes were analyzed with analysis of variance (ANOVA). Post-hoc multiple comparisons were done by the Tukey honestly significance difference test. When the P value was less than 0.05, the statistical test was determined to be significant.
To determine the errors associated with the radiographic measurements, 10 radiographs were selected randomly. Their tracings were repeated 8 weeks after the first measurements. A Bland-Altman plot was applied to assess the repeatability. The differences between the first and second measurements were insignificant ( Table I ).
| Measurements | Correlation | Bias | 95% Cl | SE | SD of differences |
|---|---|---|---|---|---|
| Upper pharynx | 0.50 | −0.27 | −0.684 to 0.146 | 0.19 | 0.78 |
| Lower pharynx | 0.04 | −0.29 | −0.566 to −0.006 | 0.13 | 0.53 |
| Adenoidal area | 0.13 | −0.30 | −1.7 to 1.0 | 0.63 | 2.50 |
| Aerial area | 0.04 | −6.02 | −10.10 to −1.94 | 1.91 | 7.66 |
| Total area | 0.01 | −6.37 | −10.17 to −2.57 | 1.78 | 7.13 |
Results
Descriptive pretreatment and control values of measurements and statistical comparisons are presented in Table II . Pretreatment and posttreatment and control descriptive statistical values and comparisons are given in Table III . Mean difference and standard deviations of the measurements and the post-hoc statistical comparisons are presented in Table IV .
| Measurement | CFM group (pretreatment) | MFM group (pretreatment) | Control group (initial) | P | |||
|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | ||
| Natural head position measurements | |||||||
| Transversal (roll) (°) | 9.2 | 2.1 | 5.3 | 11.8 | 3.2 | 11.9 | 0.388 |
| Sagittal (pitch) (°) | −6.3 | 6.4 | −8.8 | 9.7 | 1.4 | 11.4 | 0.056 |
| Skeletal measurements | |||||||
| SNA (°) | 77.1 | 1.5 | 77.3 | 2.1 | 77.8 | 2.0 | 0.544 |
| SNB (°) | 79.8 | 2.3 | 80.2 | 2.4 | 79.9 | 2.2 | 0.680 |
| ANB (°) | −2.7 | 1.4 | −2.9 | 2.2 | −2.1 | 1.7 | 0.154 |
| SN-MP (°) | 35.4 | 2.5 | 34.6 | 3.4 | 34.9 | 2.7 | 0.241 |
| SN-PP (°) | 9.5 | 3.6 | 9.2 | 3.2 | 9.4 | 3.1 | 0.169 |
| A to N perp (mm) | −2.8 | 1.8 | −3.1 | 2.4 | −2.2 | 1.9 | 0.174 |
| Pg-Na Perp (mm) | −1.1 | 3.4 | −0.8 | 4.1 | −0.5 | 3.7 | 0.632 |
| Dental measurements | |||||||
| Interincisal angle (°) | 132.8 | 11.2 | 137.1 | 11.8 | 136.3 | 9.9 | 0.089 |
| U1-NA (mm) | 3.3 | 1.7 | 4.0 | 2.2 | 2.9 | 2.4 | 0.076 |
| U1-NA (°) | 24.3 | 6.1 | 26.3 | 7.1 | 23.9 | 8.3 | 0.321 |
| L1-NB (mm) | 2.9 | 1.4 | 2.2 | 1.2 | 2.7 | 1.3 | 0.678 |
| L1-NB (°) | 22.3 | 5.7 | 20.6 | 6.4 | 21.7 | 6.1 | 0.576 |
| Soft-tissue measurements | |||||||
| UL to E plane (mm) | −3.5 | 1.9 | −4.0 | 2.1 | −4.1 | 2.2 | 0.746 |
| LL to E plane (mm) | 0.6 | 2.2 | 0.0 | 2.1 | −0.1 | 2.4 | 0.781 |
| Measurement | CFM group | MFM group | Control group | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pretreatment | Posttreatment | P value ∗ | Pretreatment | Posttreatment | P value ∗ | Observation 1 | Observation 2 | P value ∗ | |||||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | ||||
| Transversal (roll) (°) | 9.24 | 2.13 | 6.51 | 7.51 | 0.229 | 5.34 | 11.80 | 6.96 | 5.41 | 0.890 | 3.23 | 11.89 | 6.79 | 10.00 | 0.583 |
| Sagittal (pitch) (°) | −6.31 | 6.44 | 7.25 | 18.85 | 0.009 | −8.77 | 9.66 | 6.25 | 24.57 | 0.017 | 1.37 | 11.39 | 0.86 | 10.52 | 0.326 |
| Upper pharynx (mm) | 7.58 | 2.90 | 9.73 | −2.71 | 0.005 | 9.28 | 2.972274 | 10.96733 | −3.00794 | 0.005 | 8.591333 | 2.800398 | 9.614667 | −3.28113 | 0.020 |
| Lower pharynx (mm) | 10.69 | 2.98 | 10.50 | 2.20 | 0.813 | 10.76133 | 3.550758 | 10.96667 | 4.320702 | 0.880 | 11.47333 | 4.195368 | 11.05267 | 3.633777 | 0.669 |
| Adenoidal area (mm 2 ) | 311.82 | 154.11 | 303.27 | 149.20 | 0.712 | 220.9353 | 85.90047 | 259.696 | 90.78401 | 0.052 | 319.414 | 107.9055 | 301.4147 | 92.8669 | 0.094 |
| Aerial area (mm 2 ) | 478.83 | 132.76 | 604.95 | 157.76 | 0.003 | 376.132 | 90.99299 | 555.1667 | 130.5534 | <0.001 | 531.3 | 143.7499 | 568.1627 | 150.56 | 0.135 |
| Total area (mm 2 ) | 790.65 | 244.88 | 908.22 | 183.38 | 0.030 | 597.0673 | 128.1281 | 814.8627 | 145.9195 | <0.001 | 850.714 | 174.2346 | 869.5773 | 175.0755 | 0.499 |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


