Introduction
The aim of this study was to compare Delaire and Grummons protraction facemasks with a new articulator system (Amtech MG1, American Technologies, Brazil) that can record condylar positions.
Methods
Thirty-four patients treated with protraction facemask therapy were divided into 2 groups; 18 were treated with the Delaire facemask (DFM) and 16 with the Grummons facemask (GFM). The observation periods were 8.5 months for the DFM group and 10 months for the GFM group. Mandibular position indicator (MPI) recordings were taken with the new articulator system and evaluated before and after the protraction facemask therapies.
Results
MPI recordings in the sagittal plane showed forward and downward movement from centric relation to maximum intercuspal position for both condyles at the beginning of treatment for most patients. After treatment, the discrepancy between centric relation and maximum intercuspation was less in the DFM group than in the GFM group. However, more compressive movement of the condyles through the glenoid fossa was observed in the DFM group.
Conclusions
Although the centric slide amount decreased more with the Delaire facemask compared with the Grummons facemask, patients treated with the Delaire facemask must be monitored for signs and symptoms of temporomandibular joint disorder.
Dentofacial orthopedics deals with the adjustment of relationships between and among the facial bones from heavy forces, or the stimulation and redirection of functional forces in the craniofacial complex. For patients with Class III malocclusion and maxillary deficiency, the use of maxillary protraction appliances is well documented in the orthodontic literature.
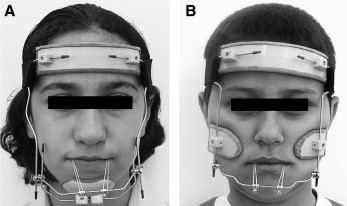
The conventional design of the facemask introduced by Dr Jean Delaire consists of a forehead support, a chincup, a prelabial arch, and a metal frame ( Fig 1 , A ). In order to protract the maxillary complex, the mandible and forehead are used as an anchorage unit with the Delaire facemask (DFM). In general, 700 to 800 g of orthopedic force is used to protract the maxilla with 70% to 75% of the force transmitted to the temporomandibular joint (TMJ). So, the TMJ must be considered under these heavy intermittent orthopedic forces. Dr Duane Grummons, who supported disengagement of the mandible during maxillary protraction, introduced a new type of facemask, called the Grummons facemask (GFM). It uses the zygomatic region as an anchorage unit for maxillary protraction, and consists of a forehead support, 2 suborbital pads, a prelabial arch, and a metal frame ( Fig 1 , B ). The animal study of Jackson et al showed that maxillary protraction without a chin support caused no histologic changes in the TMJ. Although there are hypotheses about the effects of the DFM and the GFM on the TMJ, the validity of these assumptions are still controversial.
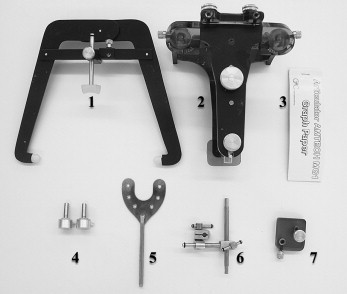
In the etiology of TMJ disorders, an important factor is the shift of the mandible due to the premature contacts in skeletal and dental Class III patients. Although TMJ sounds are less likely to occur in children than in adults, untreated mandibular deviations can lead to TMJ disorders. To determine the deviations in the TMJ and to view the condyles, contemporary radiology gives orthodontists various choices. However, trying to determine and evaluate 3-dimensional condylar positions by using 2-dimensional radiographic data is not reliable. Therefore, mounting the dental models in centric relation (CR) to the articulators with condylar position recording devices and applying the mandibular position indicator (MPI) procedure are recommended. Several companies such as SAM Präzisionstechnik GmbH (München, Germany), Panadent Corp. (Colton, CA, USA) and Whip Mix Corp. (Fort Collins, CO, USA) design and manufacture articulators that are widely used for this procedure. The instrumentation, working system, and reliability of these articulators are well documented in the literature. In this study, a new articulator system called the Amtech MG1 (American Technologies, Brazil) ( Fig 2 ) was used to evaluate condylar positions.
The purposes of this study were (1) to record the condylar positions of patients with Class III malocclusion and maxillary deficiency in CR and maximum intercuspation (MI) positions, (2) to evaluate the centric slide (CS) amount and direction in Class III patients with maxillary deficiency with the MPI method, (3) to examine and compare the effects of the DFM and GFM on TMJ by using the MPI method.
Material and methods
The parent sample was chosen from among the patients who were referred to Hacettepe University, Ankara, Turkey, with the chief complaint of anterior crossbite or edge-to-edge incisal relationship. To choose patients with maxillary deficiency, lateral cephalograms of these 50 patients (26 girls, 24 boys) were obtained. All cephalograms were traced, digitized, and evaluated by using the Jiffy Orthodontic Evaluation (JOE) program (version 5.0, Rocky Mountain Orthodontics, Denver, Colo). Mainly, the Ricketts and Steiner analyses were used to evaluate whether there was a maxillary deficiency. Furthermore, patients’ digitized tracings were superimposed with the race-specific visual norms on the nasion-basion line at nasion by using the same software. We included patients with ANB angle less than 1°, convexity value less than 1 mm, maxillary depth less than 90°, Wits appraisal of −1.5 mm or less, overjet of 0 mm or less, Class III or super Class I molar relationship, no permanent teeth congenitally missing or extracted before or during treatment, apparent maxillary deficiency seen on the superimpositions, prepubertal maturation stages 2 and 3 according to the cervical vertebral maturation method, and no functional anterior crossbite.
From the parent sample of 50 patients, 35 patients who satisfied the inclusion criteria were selected for this study. One patient moved to another city after the study started and was excluded. Thus, our study was completed with 34 patients (15 girls, 19 boys). Patients were selected randomly for DFM and GFM therapy. The DFM group consisted of 18 patients (10 girls, 8 boys), and the GFM group included 16 patients (5 girls, 11 boys). The mean ages at the start of treatment (T0) were 9.03 ± 0.82 years and 9.2 ± 1.1 years for the DFM and GFM groups, respectively.
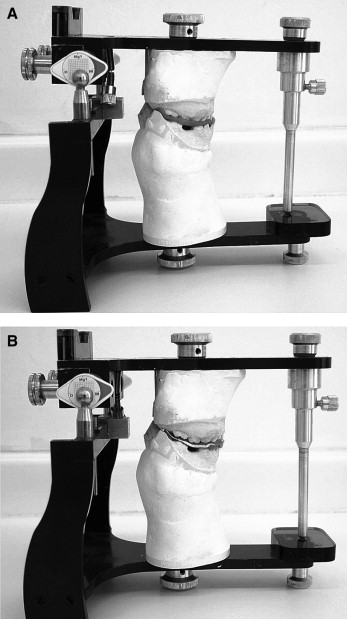
To obtain the necessary data for the MPI recordings, maxillary and mandibular casts, MI and CR bite registrations, and face-bow recordings for each patient were taken before facemask treatment. The bilateral manipulation method was used to take the CR bite registrations, and another bite registration was also taken for the MI position. The patients’ maxillary and mandibular casts were mounted on the MG1 articulator ( Fig 3 ) for the MPI procedure, as recommended by the manufacturer. First, the maxillary model was mounted to the articulator by using its custom face-bow. After mounting the maxillary cast, the articulator was placed upside down, and the CR wax registration was placed between the maxillary and mandibular casts. A layer of plaster was applied, and the lower part of the articulator was closed. After the plaster was set, condylar housings were replaced with condylar measurement drums, and the stickers were attached. The centers of the stickers indicated the condylar position in CR. Then, the CR registration wax was replaced with the MI registration wax. An articulation paper was placed between the condyle and the measurement drum. The measurement drum was moved outward to contact the condyle. As a result, a registration corresponding to the condylar position at MI was obtained on the sticker. The articulator also allowed recording the mandibular sliding in a transverse direction from CR to MI. To obtain these data, the sticker was placed on the lower side of the upper frame. Casts were placed in their respective frames with the CR registration wax between them. An articulation paper was placed between the sticker and the transfer pin. Then the transfer pin was inserted from the hole on the lower frame until it contacted the sticker. The same procedure was repeated with the MI registration wax between the casts. As a result, 2 registration marks were recorded corresponding to transverse mandibular sliding.
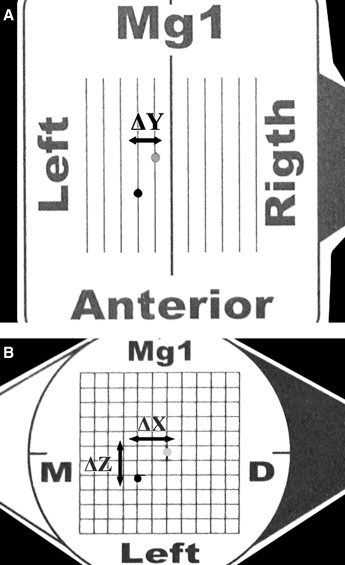
On millimetric graph paper, the transverse (mediolateral) shift was represented by ΔY ( Fig 4 , A ). The ΔY value is negative when the MI position is on the left of the CR position. The ΔY value is positive when the MI position is on the right of the CR position. Sagittal (anteroposterior and superoinferior) shifts of the condyles were marked and represented by ΔX and ΔZ ( Fig 4 , B ), respectively. The ΔX value is positive when the MI position is located anterior of the CR position. The ΔX value is negative when the MI position is posterior of the CR position. The ΔZ value is positive when the MI position is located inferior to the CR position. The ΔZ value is negative when the MI position is superior to the CR position. Negative and positive values for ΔZ are also called compression and distraction, respectively.
To evaluate the reliability of the MG1 articulator, the MPI recordings were retaken from 10 randomly selected patients before facemask therapy. Random error was calculated by using Dahlberg’s formula. Method errors for the ΔX, ΔZ, and ΔY linear measurements were less than 0.3 mm.
In both groups, force was applied through a maxillary fixed labiolingual bar with an anterior point of application. A total of 600 to 700 g of force (300-350 g for each side) was applied between the lateral incisors and canines. The angle between the occlusal plane and the force vector of the facemask was approximately 20° to 25°, and the patients were instructed to wear the appliance 14 to 16 hours a day in both treatment groups. After a positive overjet was achieved (T1), the MPI recordings were repeated as stated previously.
To evaluate the treatment changes between T0 and T1, Wilcoxon signed rank tests were used, and, to compare the T0 values of both groups, Mann-Whitney U tests were used. The level of significance was established as P <0.05 for all statistical tests.
Results
The mean age of the patients in the DFM group was 9.03 ± 0.82 years, and the mean treatment time was 8.06 ± 1.63 months. The mean age of the patients in the GFM group was 9.20 ± 1.10 years, and the mean treatment time was 10.59 ± 1.42 months.
No statistically significant differences were found for the ΔX (anteroposterior), ΔZ (superoinferior), and ΔY (mediolateral) distances between the groups at T0 ( Table I ). When the means of ΔX of all patients were evaluated together at T0, 26 patients (76.5%) had a protrusive slide, 6 patients (17.7%) had a retrusive slide, and 2 patients (5.8%) had no anteroposterior slide for the right condyle; 27 patients (79.4%) had a protrusive slide, 6 patients (17.7%) had a retrusive slide, and 1 patient (2.9%) had no anteroposterior slide for the left condyle. When the means of ΔZ of all patients were evaluated together at T0, 28 patients (82.4%) had distraction, 1 patient (2.9%) had compression and 5 patients (14.7%) had no superoinferior slide for the right condyle; 32 patients (94.2%) had distraction, 1 patient (2.9%) had compression, and 1 patient (2.9%) had no superoinferior slide for the left condyle. Graphical representations of CS relative to CR are shown in Figures 5 and 6 for the DFM and GFM groups, respectively. The transverse slide (ΔY) was equal (left slide in 17 patients and right slide in 17 patients) at T0.
| DFM (n = 18) | GFM (n = 16) | ||||
|---|---|---|---|---|---|
| T0 | Mean | SD | Mean | SD | P |
| ΔX right condyle (mm) | 1.13 | 1.46 | 0.81 | 1.10 | 0.427 |
| ΔX left condyle (mm) | 1.31 | 1.30 | 0.90 | 1.42 | 0.512 |
| ΔZ right condyle (mm) | −0.97 | 0.96 | −0.90 | 0.57 | 0.628 |
| ΔZ left condyle (mm) | −1.27 | 0.88 | −1.16 | 0.79 | 0.557 |
| ΔY (mm) | −0.06 | 1.02 | 0.07 | 0.78 | 0.691 |
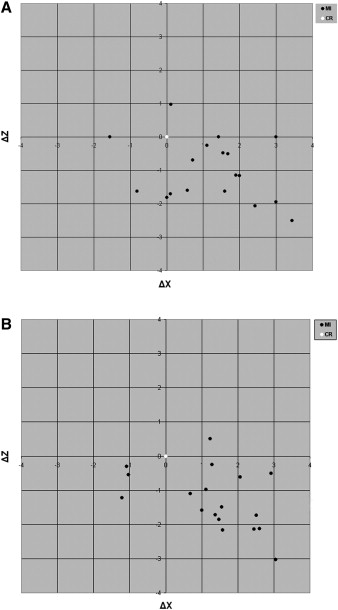
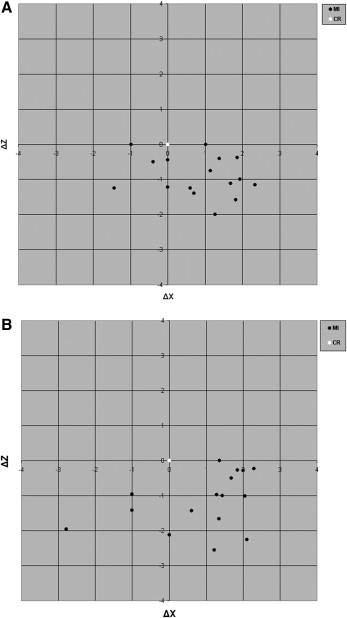
There were statistically significant decreases for ΔX and ΔZ in both groups at T1 ( Table II , Figs 7 and 8 ). However, when the groups were compared in terms of treatment type, there were significant differences for the ΔX values of the right and left condyles and the ΔZ value of the left condyle ( Table III ). Although there were no significant differences for the ΔZ value of the right condyle and the ΔY value, the discrepancies between the CR and MI positions decreased more in the DFM group compared with the GFM group ( Table III ).
| Variable interval | |||||||
|---|---|---|---|---|---|---|---|
| Mean | SD | Median | Minimum | Maximum | P | ||
| DFM group | |||||||
| ΔX right condyle (mm) | T0 | 1.13 | 1.46 | 1.48 | −1.56 | 3.44 | 0.007 † |
| T1 | 0.02 | 0.14 | 0.00 | −0.25 | 0.47 | ||
| ΔX left condyle (mm) | T0 | 1.31 | 1.30 | 1.43 | −1.21 | 3.05 | 0.002 † |
| T1 | 0.08 | 0.20 | 0.00 | −0.12 | 0.71 | ||
| ΔZ right condyle (mm) | T0 | −0.97 | 0.96 | −1.16 | −2.51 | 0.97 | 0.001 † |
| T1 | 0.03 | 0.07 | 0.00 | −0.24 | 0.30 | ||
| ΔZ left condyle (mm) | T0 | −1.27 | 0.88 | −1.35 | −3.03 | 0.50 | 0.000 ‡ |
| T1 | 0.05 | 0.08 | 0.00 | −0.27 | 0.25 | ||
| ΔY (mm) | T0 | −0.06 | 1.02 | −0.22 | −2.21 | 1.72 | 0.879 |
| T1 | −0.01 | 0.06 | 0.00 | −0.17 | 0.18 | ||
| GFM group | |||||||
| ΔX right condyle (mm) | T0 | 0.81 | 1.10 | 1.08 | −1.43 | 2.34 | 0.012 ∗ |
| T1 | 0.43 | 0.72 | 0.38 | −1.00 | 1.45 | ||
| ΔX left condyle (mm) | T0 | 0.90 | 1.42 | 1.35 | −2.78 | 2.30 | 0.041 ∗ |
| T1 | 0.26 | 0.54 | 0.30 | −1.28 | 1.00 | ||
| ΔZ right condyle (mm) | T0 | −0.90 | 0.57 | −1.06 | −2.00 | 0.00 | 0.001 † |
| T1 | −0.59 | 0.47 | −0.65 | −1.48 | 0.25 | ||
| ΔZ left condyle (mm) | T0 | −1.16 | 0.79 | −1.01 | −2.55 | 0.00 | 0.000 ‡ |
| T1 | −0.51 | 0.55 | −0.38 | −1.76 | 0.42 | ||
| ΔY (mm) | T0 | 0.07 | 0.78 | 0.32 | −1.62 | 1.56 | 0.569 |
| T1 | 0.06 | 0.18 | 0.05 | −0.26 | 0.33 | ||
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


