Introduction
The first straight-wire appliance was introduced over 40 years ago to increase the consistency and efficiency of orthodontic treatment. More recently, computer-aided design and computer-aided manufacturing (CAD/CAM) technology has been used to create individualized orthodontic appliances. The purpose of this study was to investigate the clinical effectiveness and efficiency of CAD/CAM customized orthodontic appliances compared with direct and indirect bonded stock orthodontic brackets.
Methods
This retrospective study included 3 treatment groups: group 1 patients were direct bonded with self-ligating appliances, group 2 patients were indirect bonded with self-ligating appliances, and group 3 patients were indirect bonded with CAD/CAM self-ligating appliances. Complete pretreatment and posttreatment records were obtained for all patients. The American Board of Orthodontics (ABO) Discrepancy Index was used to evaluate the pretreatment records, and the posttreatment outcomes were analyzed using the ABO Cast-Radiograph Evaluation. All data collection and analysis were completed by 1 evaluator.
Results
There were no statistically significant differences in the ABO Discrepancy Index or the ABO Cast-Radiograph Evaluation among the groups. Treatment times for the 3 groups were significantly different; the CAD/CAM group was the shortest at 13.8 ± 3.4 months, compared with 21.9 ± 5.0 and 16.9 ± 4.1 months for the direct bonded and indirect bonded groups, respectively. The number of treatment appointments for the CAD/CAM group was significantly fewer than for the direct bonded group.
Conclusions
The CAD/CAM orthodontic bracket system evaluated in this study was as effective in treatment outcome measures as were standard brackets bonded both directly and indirectly. The CAD/CAM appliance was more efficient in regard to treatment duration, although the decrease in total archwire appointments was minimal. Further investigation is needed to better quantify the clinical benefits of CAD/CAM orthodontic appliances.
Highlights
- •
Treatment outcomes were compared in direct, indirect, and CAD/CAM bonded groups.
- •
Treatment outcomes (effectiveness) were similar in all 3 groups.
- •
Treatment time (efficiency) was shorter in the CAD/CAM group.
The goal of orthodontic treatment is to achieve an exemplary treatment outcome in a reasonable amount of time. Orthodontic treatment should be not only effective, but also efficient in terms of total treatment time and number of appointments. A critical component of achieving these goals is an optimal orthodontic bracket placed in the ideal position on each tooth.
Nearly 40 years ago, Andrews developed the first true straight-wire appliance. Andrews’ brackets had specific first-, second-, and third-order prescriptions for each tooth; this increased the consistency of the treatment results and improved the treatment efficiency because fewer bends were required in both aligning and finishing archwires. Many straight-wire bracket prescriptions are now available, all with a common goal of shortening the aligning and finishing stages of orthodontic treatment by minimizing the amount of wire bending.
A critical element in the success of any straight-wire appliance is that each bracket must be accurately positioned on every tooth in the arch; however, this is clinically difficult because of anatomic variations in tooth morphology and human error. Balut et al completed a study on direct bonding accuracy, analyzing brackets placed on dental casts mounted in mannequins, and found significant differences in both vertical positioning and angulation of the appliances. Interestingly, removing clinical obstacles such as patient management, isolation control, and visualization difficulties did not eliminate bonding errors by experienced clinicians.
To decrease direct bonding errors and doctor chairside time during bonding appointments, there has been much experimentation with laboratory-fabricated indirect bonding trays. Many materials have been used for the indirect delivery system, including polyvinyl siloxane, prosthodontics putties, silicone gels, and thermoplastic trays. The objective of laboratory-fabricated indirect bonding protocols is to easily and accurately place brackets extraorally on a handheld model and then precisely transfer the ideally placed brackets to the patient’s teeth. Indirect bonding techniques have shown good bond strength; however, the accuracy of the technique has had varying success in several investigations. Koo et al found minimal improvements in accuracy with laboratory-fabricated indirect bonding techniques compared with direct bonding; both failed to execute ideal bracket placement. In addition to inaccurate bracket placement and variations in tooth anatomy, Creekmore and Kunik cited variations in vertical and anteroposterior jaw relationships, tissue rebound, and inherent mechanical deficiencies of edgewise orthodontic appliances as other factors that must be addressed in the development of an actual “straight-wire” orthodontic appliance.
Computer-aided design and computer-aided manufacturing (CAD/CAM) have been a focus of dental research since the 1980s to minimize human error in dentistry. Traditionally, much of the dental utilization of CAD/CAM technology has focused on the milling of crowns and fixed partial dentures. Dental applications of CAD/CAM have expanded in recent years as the benefits of the technology have been realized in new applications. Current uses of CAD/CAM technology in orthodontics include aids for diagnosis and treatment planning, clear aligner therapies, custom labial and lingual systems, and titanium Herbst appliances. Customized brackets with patient-specific torque, machine-milled indirect bonding jigs, and robotically generated archwires are among recent CAD/CAM advances in achieving a true straight-wire appliance. The overarching goal of incorporating CAD/CAM technology into orthodontics can be best summed up as “improving reproducibility, efficiency, and quality of orthodontic treatment.”
The applications of CAD/CAM in orthodontics are undoubtedly growing; unfortunately, the clinical evidence to support the applications of the technology has not kept pace. Manufacturers of customized orthodontic appliances delivered with milled indirect bonding jigs claim that these appliances reduce total treatment time, improve treatment efficiency, and yield better overall treatment results. However, many of these claims are unsubstantiated by scientific evidence. Weber et al investigated a commercially available CAD/CAM orthodontic system comparing treatment effectiveness and efficiency of the customized appliances to traditional twin appliances. The study reported significantly lower American Board of Orthodontic (ABO) scores, fewer archwire appointments, and shorter overall treatment times in the CAD/CAM group. Although these findings are promising, the study did not distinguish whether the clinical benefits were due to indirect bonding in the CAD/CAM group or the actual customized brackets.
The aim of our study was to expand the existing CAD/CAM orthodontic appliance literature by comparing treatment effectiveness and efficiency of 3 systems: (1) direct bonded self-ligating brackets, (2) indirect bonded self-ligating brackets, and (3) indirect bonded CAD/CAM self-ligating brackets. The null hypothesis was there will be no difference in effectiveness or efficiency measures among the 3 treatment groups.
Material and methods
This retrospective study was approved by the institutional review board at the University of North Carolina at Chapel Hill. All patients were treated by a private orthodontic practitioner between March 2008 and August 2013. During this time, the practitioner sequentially used 3 bonding protocols for comprehensive patients with no overlap: group 1, direct bonded self-ligating (Damon Q; Ormco, Orange, Calif) appliances (2008-2010); group 2, indirect bonded self-ligating (Damon Q; Ormco) appliances (2010-2011); and group 3, indirect bonded CAD/CAM self-ligating (Insignia SL; Ormco) appliances (2011-2013).
Consecutively treated patients from these 3 treatment groups were identified, and the following criteria were applied. The inclusion criteria were (1) complete maxillary and mandibular fixed appliances were used; (2) treatment included only intraoral, intra-arch, or interarch mechanics; and (3) complete chart entries, pretreatment and posttreatment digital casts, pretreatment cephalometric radiographs, and posttreatment panoramic radiographs were available. The exclusion criteria were (1) functional appliances, growth modification, extractions, temporary skeletal anchorage, impacted teeth (other than third molars), or orthognathic surgery was involved in treatment; (2) postorthodontic restorative treatment was required; and (3) pretreatment or posttreatment records were incomplete.
After the inclusion and exclusion criteria were applied to the potential subjects, group 1 contained 31 patients, group 2 contained 33 patients, and group 3 contained 32 patients. The sequential patients evaluated for inclusion in the study were selected from the middle range of the patient list of each treatment group to minimize the learning-curve effects associated with a new treatment protocol.
Demographic data for the study participants included sex and age at the beginning of treatment. Treatment data consisted of the number of treatment appointments (including bonding, archwire adjustments, emergencies, and debonding), duration of treatment (months), initial and final clinical photographs, initial cephalometric radiographs, final panoramic radiographs, and pretreatment and posttreatment eModel digital casts (GeoDigm Corp, Falcon Height, Minn). Emergencies were counted as appointments if brackets were replaced or wires changed, but not if long wires extending out of molar tubes were clipped. Although digital measures of overjet, overbite, and crowding have been validated, marginal ridge, buccolingual inclination, and occlusal contacts have not. Therefore, the posttreatment digital models were converted from eModel’s proprietary software file format into a stereolithography file and then printed on a 3-dimensional printer (iPro 8000; 3D Systems, Rockhill, SC). All subjects and treatment data were assigned a random coded number by a research assistant to blind the evaluator (M.W.B.) during data scoring and analysis.
The ABO Discrepancy Index was used on the pretreatment digital casts using eModel’s software analysis program and by evaluation of the initial cephalometric radiographs. The ABO Discrepancy Index score established a numeric value correlating to the relative severity of the orthodontic problems of each subject. The stereolithography posttreatment models and final panoramic radiographs were evaluated using the ABO Cast-Radiograph Evaluation to objectively quantify the treatment outcome of each patient. Before data collection, the evaluator was trained and calibrated on both the ABO Discrepancy Index and the ABO Cast-Radiograph Evaluation techniques. He performed all measurements and case analyses.
One week after completion of the data collection, the ABO Discrepancy Index and Cast-Radiograph Evaluation were repeated on 10 randomly selected subjects to assess intraexaminer reliability. The intraclass correlation coefficient values were 0.95 for the ABO Discrepancy Index and 0.91 for the ABO Cast-Radiograph Evaluation scores; these show almost perfect correlations and demonstrate the reliability and consistency of the principal investigator with the evaluation techniques.
Statistical analysis
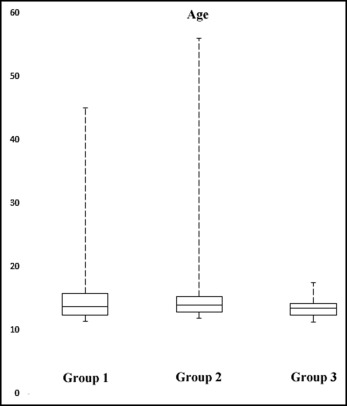
Statistical analysis was performed using SPSS software (version 22.0; IBM, Armonk, NY). The age distribution of the groups at the beginning of treatment is shown in Figure 1 . Age, ABO Discrepancy Index values, ABO Cast-Radiograph categorical values and overall scores, treatment duration (months), and number of treatment appointments did not pass normality testing; therefore, the Kruskal-Wallis test was used for statistical analysis. The Benjamini-Hochberg test was then applied to control for the false discovery rate. A multiple comparison test was used for the post hoc analysis.
Results
The median ages at the beginning of treatment were 13.58, 13.92, and 13.42 years for groups 1, 2, and 3, respectively ( Table I ; Fig 1 ). There were no significant differences in the median ages between the groups ( P = 0.252). Group 1 consisted of 15 females and 16 males, group 2 consisted of 17 females and 16 males, and group 3 consisted of 17 females and 15 males ( Table I ). The ABO Discrepancy Index values were 16.0 ± 9.1 for group 1, 15.9 ± 8.1 for group 2, and 16.8 ± 6.5 for group 3 ( Table II ). These differences were not statistically significant ( P = 0.56).
| n | Median age (y) | Females (n) | Males (n) | |
|---|---|---|---|---|
| Group 1 | 31 | 13.58 | 15 | 16 |
| Group 2 | 33 | 13.92 | 17 | 16 |
| Group 3 | 32 | 13.42 | 17 | 15 |
| 0% (minimum) | 25% | 50% (median) | 75% | 100% (maximum) | Mean | SD | P value | |
|---|---|---|---|---|---|---|---|---|
| ABO DI | 0.56 | |||||||
| Group 1 | 2 | 12 | 15 | 19 | 44 | 16.0 | 9.1 | |
| Group 2 | 4 | 12 | 14 | 19 | 40 | 15.9 | 8.1 | |
| Group 3 | 5 | 13 | 17 | 20 | 33 | 16.8 | 6.5 | |
| ABO CRE | 0.13 | |||||||
| Group 1 | 15 | 21.5 | 28 | 34.5 | 47 | 28.5 | 8.5 | |
| Group 2 | 18 | 26 | 34 | 37 | 52 | 32.3 | 7.8 | |
| Group 3 | 17 | 26.5 | 34 | 39 | 49 | 32.2 | 9.3 | |
| Treatment time (mo) | <0.001 | |||||||
| Group 1 | 12 | 19 | 22 | 25 | 33 | 21.9 | 5.0 | |
| Group 2 | 9 | 15 | 18 | 19 | 30 | 16.9 | 4.1 | |
| Group 3 | 8 | 11 | 13 | 17 | 21 | 13.8 | 3.4 | |
| Treatment appointments (n) | 0.02 | |||||||
| Group 1 | 10 | 14 | 16 | 19 | 28 | 16.5 | 4.0 | |
| Group 2 | 9 | 12 | 14 | 18 | 25 | 14.9 | 3.7 | |
| Group 3 | 8 | 11 | 13 | 17 | 23 | 14.1 | 3.9 |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


