Introduction
This article illustrates a new treatment method and evaluates the effect of the frequent use of fluoridated chewing sticks (miswaks) on the remineralization of white spot lesions (WSLs) diagnosed at debonding.
Methods
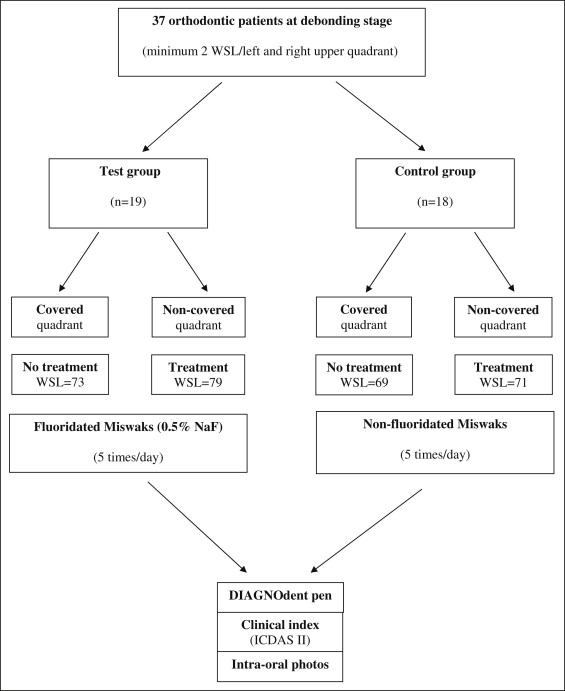
Thirty-seven orthodontic patients (mean age, 17.2 years), with a minimum of 4 WSLs on the buccal surfaces of the maxillary incisors, canines, premolars, and first molars after orthodontic therapy, were enrolled in a double-blind, randomized, longitudinal trial lasting 6 weeks. The subjects were divided into 2 groups using fluoridated miswaks impregnated in 0.5% sodium fluoride (test group, n = 19) and nonfluoridated miswaks (control group, n = 18). A custom-made mouth tray, covering half of the maxillary dentition, was used while brushing with the miswaks 5 times per day. The WSLs were scored by using a DIAGNOdent pen (KaVo, Biberach, Germany) and with the International Caries Detection and Assessment System (ICDAS II) index, at baseline and 2, 4, and 6 weeks after debonding.
Results
Both the DIAGNOdent readings and the ICDAS II index of the WSLs decreased in the test group on the uncovered side of the dentition but not on the covered side during the 6-week trial ( P <0.0001). There was also a slight improvement in the control group (not significant). There was a strong correlation between the DIAGNOdent values and the ICDAS II index when all the data were pooled ( P <0.001).
Conclusions
The frequent use of fluoridated miswaks had a remineralizing effect on WSLs. The DIAGNOdent pen might be a useful tool for diagnosing and monitoring changes of WSLs over a relatively short period of time.
Caries lesions on smooth surfaces are commonly found in patients with high caries activity during and after orthodontic treatment. Studies have shown that white spot lesions (WSLs) can develop within 1 month after bonding. The prevalence of WSLs after orthodontic treatment varies in different studies. Minor lesions can be esthetically disturbing and often remain after the treatment, and advanced lesions might require restorative treatment. This problem can be minimized by preventive treatment with fluoride toothpaste and rinsing solutions, oral hygiene instructions, and topical fluoride applications.
The clinical diagnosis of WSLs has been made primarily by using traditional methods, such as visual inspection after air drying and tactile examination by dental probing. However, the subjectivity, lack of reproducibility, and prerequisite of the presence of a significantly advanced lesion have led to the introduction of several optical devices in recent decades. One such technique is laser fluorescence. The results of recent studies suggest that this technique might be appropriate for the early detection and assessment of WSLs in orthodontic patients.
A new clinical index, the International Caries Detection and Assessment System (ICDAS), was developed as an internationally accepted caries detection system that would also enable the assessment of early enamel demineralization. In the ICDAS I (2003), the visual examination was carried out on clean, plaque-free teeth after careful drying. The criteria were subsequently modified, and the ICDAS II was created. The improvement consisted of an exchange of codes to ensure that the system would reflect increased severity.
Chewing sticks (miswaks) are used in many countries around the world for cleaning purposes, often up to 5 times a day. We have recently developed a procedure to impregnate miswaks with fluoride. The data show that the fluoride released from the chewing stick is rapid, and miswaks are thereby suitable for caries prevention. The advantage of fluoridated miswaks is that they have a dual effect: cleaning the buccal surfaces and producing a high fluoride concentration on the teeth. The aim of this study was to evaluate the effect of the frequent use of fluoridated miswaks on the remineralization of WSLs diagnosed at debonding.
Material and methods
Thirty-seven orthodontic patients (11 males and 26 females; mean age, 17.2 years) were recruited from 3 dental hospitals in Jeddah, Saudi Arabia: King Fahad Armed Forces Hospital, King Faisal Specialist Hospital and Research Center, and King Fahad General Hospital. Figure 1 shows the schematic design of the study. The subjects were selected from a group of orthodontic patients who had full fixed appliance therapy (straight wire appliances) because of bimaxillary crowding, with a mean treatment period of 18 months. The inclusion criterion was at least 2 WSLs on both the left and right sides of the maxillary dentition (teeth 16-26), adjacent to the site of the orthodontic band or bracket: ie, a minimum of 4 WSLs per subject (totals of 152 WSLs in the test group and 140 WSLs in the control group). Ethical approval was obtained before starting the study (reference number, 1430H-05-09; May 4, 2009).
All participants and their parents were informed about the study, and written consent was obtained before the start. After debonding and debanding, full-mouth cleaning with a rotating rubber cup, by using pumice and water, and, if necessary, professional supragingival scaling, was performed to remove plaque, calculus, and any remaining composite bonding material. Care was taken to avoid disturbing the WSLs that would be evaluated.
The study was performed as a double-blind, longitudinal trial lasting 6 weeks. The participants were randomly divided based on a randomization list into 2 groups: a test group of 19 patients using fluoridated miswaks impregnated in 0.5% sodium fluoride, and a control group with 18 patients using nonfluoridated miswaks. The fluoridated miswaks were impregnated in 0.5% sodium fluoride as previously described in detail by Baeshen et al. The 2 types of miswaks were identical except for their fluoride content. They were packed in plastic bags and coded.
The chewing sticks for both groups were used on 1 side of the maxilla, 5 times a day for 6 weeks; special attention was paid to the WSLs. An individual plastic mouth tray (Essix, Dentsply International, Parkland, Fla) covering half of the dentition was used, as shown in Figure 2 . The rationale of the tray was to keep the covered side away from the direct effect of the fluoride released from the fluoridated miswak to compare it with the noncovered side; the tray was placed based on the randomized order list. The tray was applied to the teeth immediately after toothbrushing and kept in place while using the miswak and for a minimum of 30 minutes afterward. Written instructions, with photo illustrations, were also given to the patient and his or her parent to ensure that the miswak and the mouth tray were used correctly. All subjects were told to use fluoridated toothpaste (1450 ppm F, Signal 2, Binzagr Unilever, Jeddah, Saudi Arabia) twice a day, but they were instructed to use no other fluoride products during the 6-week trial.

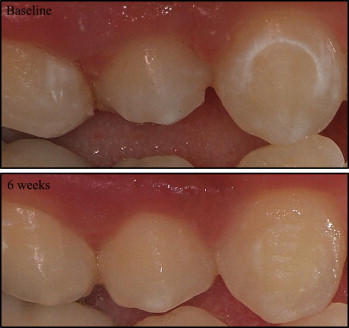
At baseline (debonding visit) and 2, 4, and 6 weeks after debonding, the WSLs were scored by using 2 methods: DIAGNOdent pen (KaVo, Biberach, Germany) and visual examination with the ICDAS II index. The buccal surfaces of all test teeth were photographed with a digital camera (Fujifilm FinePix S3 Pro SLR, Fuji Photo Film, Tokyo, Japan), equipped with a 105-mm macro lens and a ring flash with cross-polarization filters. The intraoral photos (1 front and 1 for each side) were taken at each visit ( Fig 3 ). The same examiner (H.B.) made all measurements and was calibrated before the study.
The same DIAGNOdent pen was used throughout the study. Before each session, the instrument was calibrated against the ceramic standard supplied by the manufacturer and then calibrated for each subject by measuring a sound area of the buccal surface. The surface was dried with compressed air for 5 seconds before measurement, which was made for 10 seconds. Each buccal surface was divided into 3 areas: mesial, center, and distal. Each site was scanned 3 times with the pen, by using probe tip 2, and the highest value from the 3 readings was registered.
Visual examination was performed immediately at debonding. The buccal surfaces of the test teeth were examined and recorded at each visit by using the ICDAS II index. This was done after drying the tooth surfaces for 5 seconds with compressed air. The assessment was performed with the aid of a mouth mirror and a blunt probe under clinical lighting, according to the ICDAS II index criteria, presented in Table I .
| Score | Meaning |
|---|---|
| 0 | Sound tooth surface. There should be no evidence of caries (either no or a questionable change in enamel translucency after prolonged air drying (approximately 5 seconds). Surfaces with developmental defects, such as enamel hypoplasias, fluorosis, tooth wear (attrition, abrasion. and erosion) and extrinsic or intrinsic stains will be recorded as sound. |
| 1 | First visual change in enamel. When seen wet, there is no evidence of any change in color that can be attributed to carious activity, but, after prolonged air drying, a carious opacity is visible that is not consistent with the clinical appearance of sound enamel. |
| 2 | Distinct visual change in enamel when viewed wet. There is a carious opacity or discoloration that is not consistent with the clinical appearance of sound enamel (Note: the lesion is still visible when dry). The lesion is located in close proximity (in touch with or within 1 mm) to the gingival margin. |
| 3 | Localized enamel breakdown due to caries with no visible dentin. After being dried for 5 seconds, there is carious loss of surface integrity without visible dentin. |
| 4 | Underlying dark shadow from dentin with or without localized enamel breakdown. This lesion appears as a shadow of discolored dentin visible through the enamel surface beyond the white or brown spot lesion, which may or may not show signs of localized breakdown. This appearance is often seen more easily when the tooth is wet and is a darkening and intrinsic shadow that might be gray, blue, or brown. |
| 5 | Distinct cavity with visible dentin. Cavitation in opaque or discolored enamel exposing the dentin beneath. |
| 6 | Extensive distinct cavity with visible dentin. Obvious loss of tooth structure, the cavity is both deep and wide, and dentin is clearly visible on the walls and at the base. An extensive cavity involves at least half of the tooth surface or possibly reaches the pulp. |
The participants and the examiner were not aware of the group assignments, not even the covered or noncovered side, to ensure the complete double blindness of the study. No records of the readings from the previous registrations were available at any of the follow-up measurements.
Statistical analysis
A power analysis was performed before the study with an assumed significance level of 0.01, a standard deviation of 3.0, at least a detectable difference of 4.0 (based on the DIAGNOdent pen values), and a power for that detection of 90%. A sample size of 17 patients per group was suggested. The “within factors” were time (4 time points) and quadrant (covered and noncovered), and the “between factor” was treatment group (fluoridated and nonfluoridated miswaks).
Means and standard deviations were calculated for each visit and patient for both ICDAS II and DIAGNOdent pen measurements. The mean values were calculated for the teeth in the same quadrant. The mean changes at baseline and at 6 weeks for the covered and noncovered sides were analyzed by using paired t tests. For comparisons between the test and control groups, a nonpaired t test was used. Since a multiple t test was used, a statistically significant difference of P <0.01 was accepted. The correlations between the ICDAS II index score and the DIAGNOdent readings at baseline and at 6 weeks were analyzed by using the Pearson’s correlation coefficient.
Twenty percent of the measurements for both the ICDAS II scores and the DIAGNOdent readings were recorded twice by the same examiner (H.B.). Cross-tabulation showed that 91% of the ICDAS II readings were the same, and 9% had a difference of ±1% only. For the DIAGNOdent readings, 84% were the same, with ±1% readings for 14.5% and ±2% readings for 1.5%.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


