Introduction
Because alveolar bone is used for skeletal anchorage, the variability and reliability of its dimensions are important.
Methods
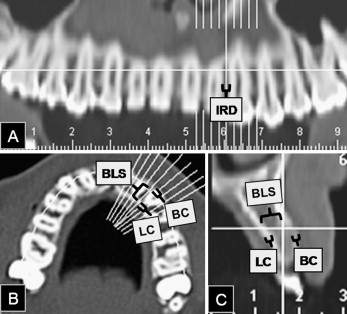
Interradicular distances, cortical thicknesses, and buccolingual spaces were measured on computed tomography images of 22 adults (13 maxillary and 9 mandibular). Intra-arch analyses were done with paired t tests; the interarch comparisons were studied with independent t tests. The intraclass correlation coefficient was calculated between corresponding units.
Results
Interradicular distances were greater for the molars than for the incisors, and apical distances were greater than cervical. The mandibular lingual cortical thickness was the greatest, and the maxillary buccal cortical thickness was less than the mandibular in the molar apical zones. The widest and narrowest buccolingual spaces were found at the maxillary molars and the mandibular incisors, respectively. The cross values of cortical bone thickness were wider than the axial means and they had low agreement, so they had interradicular distances on the right and left sides.
Conclusions
Although interradicular distances must be carefully assessed, the molars were favorable sites for skeletal anchorage. Placing anchorage in anterior sites requires even more careful planning, including the use of computed tomography records.
Editor’s comment
Temporary anchorage devices have become widely used as a method of improving the outcomes of orthodontic treatment. Orthodontists rely on them in difficult anchorage situations. Consequently, the success rate of placement of skeletal anchorage devices should be maximized to optimize their use.
These authors identified 3 parameters that they believe contribute to the success rate: interradicular space, cortical thickness, and buccolingual space. Adequate interradicular space is important to be able to place the skeletal anchorage device and not jeopardize adjacent teeth, whereas the other 2 parameters are important for maximizing the stability of the anchorage device. Greater cortical thickness lends stability to the device, as does deeper placement. They measured each parameter on computed tomography sections in the axial and cross-sectional planes.
They found that the mandibular lingual cortical plate was the thickest and the maxillary buccal plate the thinnest. Understandably, incisor interradicular space was significantly narrower than molar space, and buccolingual space was also significantly narrower in the incisor area than in the molar area.
These results will be helpful to clinicians as they plan their mechanics for patients. For example, an oblique buccal placement between the incisors would allow the use of a longer device, which would increase stability and strength. This would also allow the device’s head to be in the attached gingiva with less irritation of surrounding tissues.
In addition, the thinner cortical plate on the buccal side of the maxilla suggests that a wider diameter device might be indicated to ensure stability. However, clinicians need to be aware that the maxillary sinus might extend into the apical areas of the molars.
Leslie Will, Associate Editor
Boston, Mass