Introduction
The aim of this pilot study was to analyze the morphology of the cervical vertebrae of subjects with transverse maxillary constriction.
Methods
The study population included 40 subjects (7-11 years of age) undergoing palatal expansion to correct transverse maxillary constriction, and a control group of 40 subjects (7-11 years of age) without transverse maxillary constriction. Two observers assessed cervical morphology on lateral cephalograms by means of templates showing cervical maturation sequences. Round angles and concave vertebral body edges were classified as vertebral anomalies that could not be associated with physiologic vertebral growth. Agreement between the data collected by the observers was assessed with the Cohen kappa test, and the data of the 2 groups were compared with the Fisher exact test ( P <0.05).
Results
The 2 observers agreed in their assessments (k >0.5). The greater percentage of vertebral defects in the study group was significant ( P <0.05) according to both observers. Rounding of the anterosuperior angle of the vertebral body was the most common defect in the study group. Vertebral defects of the study group were mainly at vertebrae C4 and C5.
Conclusions
A statistically significant correlation, worthy of further study, was found between transverse maxillary constriction and cervical vertebral defects.
Transverse maxillary constriction (TMC) is a malocclusion characterized by narrow and high palatal vault, unilateral or bilateral crossbite, possible dental crowding because of contraction of the dental arches, and reduced volume of the nasal cavities.
Reliable and objective techniques to assess the geometry of nasal cavities, such as acoustic rhinometry, rhinomanometry or 3-dimensional imaging, have allowed many authors to investigate the changes in the nasal cavities of patients undergoing correction of TMC. Among the findings of these investigations were reduction of nasal airway resistance, increased nasal minimum cross-sectional area, increased binasal cavity width, and increased total nasal volume after palatal expansion. Although correction of TMC is associated with improved mechanical airflow through the nose, the effect of this procedure on the breathing pattern is still debatable. The transition from oral to nasal breathing after palatal expansion is not predictable in frequency and scale because of the variability of individual responses.
Tecco et al studied changes in head posture in mouth-breathing girls after rapid maxillary expansion and found that it increased nasopharyngeal airway patency and significantly changed craniocervical angles. McGuinness and McDonald observed a progressive decrease in extended head posture in adolescents with unilateral or bilateral crossbite undergoing rapid maxillary expansion. They attributed this phenomenon to the change from oral to nasal breathing. The literature also reports a correlation between craniocervical alterations, especially changes in normal cervical lordosis, in subjects with impaired nasal respiration. The authors supposed that these changes reflected an adaptation that restored the correct dimensions of the upper airways and ensured adequate ventilation. These phenomena might be associated with altered balance of the muscles connecting the skull to the cervical spine and chest; these muscles maintain correct posture of the head and take part in respiratory movements. Huggare and Kylamarkula observed reduced thickness of the posterior arch of the atlas in subjects with altered respiratory function from enlarged adenoids. They believed that cranial extension induced by respiratory obstruction altered the soft tissues (functional matrix) around the atlas. Other authors found vertebral morphologic anomalies in subjects with dentofacial features typically associated with oral respiration: Class II malocclusion, increased overjet, and open bite.
Cervical vertebrae are a biologic indicator for skeletal maturity. Lamparski cited 6 stages corresponding to 6 maturational phases in the cervical vertebrae that can be identified during the pubertal period. The skeletal orthopedic effects of palatal expansion techniques vary according to the morphologic characteristics of the median suture palate, which are related to individual skeletal maturation. These studies suggested that the optimal age for orthopedic correction of TMC is before the pubertal peak (cervical vertebral maturation stage 1, 2, or 3).
The aim of this preliminary study was to analyze the cervical vertebrae of subjects with TMC awaiting rapid maxillary expansion and compare them with the vertebrae of a control group without TMC.
Material and methods
The study group included 40 subjects (20 boys, 20 girls; mean age, 8 years 7 months ± 1 year 2 months) awaiting rapid maxillary expansion to correct TMC. These patients were selected from the medical records of the dentistry department of Siena University, Siena, Italy, according to the following criteria: medical history and examination negative for congenital maxillofacial malformations and related syndromes, severe skeletal asymmetries, or dentofacial deformities requiring orthognathic surgery; clear pretreatment lateral cephalometric radiographs with good contrast including vertebrae from C2 to C6; and age between 7 and 11 years at the time of cephalometric films. The patients selected needed palatal expansion for correction of bilateral or unilateral crossbite, or maxillary tooth size-arch length discrepancy when transpalatal width was less than 33 to 34 mm.
The control group consisted of 40 subjects (22 boys, 18 girls; mean age, 9 years 2 months ± 1 year 3 months) selected from the records of a dental office in Grosseto, Italy, inclusion criteria were the same as in the study group. No control subject had TMC.
The profiles of vertebrae C2 through C6 were traced on lateral cephalograms. Two independent observers (L.D.V., G.F.) assessed cervical vertebrae morphology on the images of the 2 groups. They used templates with different magnifications on 0.003-in acetate sheets showing Lamparski’s cervical maturation sequence to establish the cervical vertebral maturation stage of each subject without confusing physiologic development and growth with morphologic anomalies.
To facilitate visual analysis of the cervical vertebrae, morphologic anomalies known as vertebral defects were classified as either “round” or “concave” ( Fig 1, Fig 2 ) . “Round” was noted when extensions of the upper or lower edges met the anterior or inferior edges of the vertebral body outside the radiographic profile of the vertebra. Round was divided into anterosuperior, posterosuperior, anteroinferior, and posteroinferior according to the angle of that vertebral body.

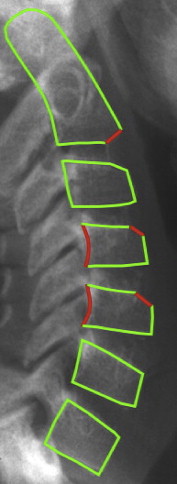
“Concave” was noted when at least 1 mm separated the midpoint of the edge of the vertebra and the line joining the vertices of the vertebra. Concave was divided into anterior, superior, inferior, and posterior according to its location on the side of the vertebra.
Normal maturation processes, such as absence of the C3 anterosuperior angle or concavity of the inferior edge of C2 characterizing Lamparski’s cervical vertebral maturation stage 2, were excluded.
Statistical analysis
The Cohen kappa test was used to measure the diagnostic concordance between the assessments of the 2 observers in the 2 groups. Detection of at least 1 vertebral defect in a patient by both observers was considered a concordant assessment. The Fisher exact test ( P <0.05) was used to compare the percentages of vertebral defects in the 2 groups. The test was calculated for both observations.
Results
Both observers found a higher percentage of vertebral defects in the TMC group (observer 1, 75%; observer 2, 83%) than in the controls (observer 1, 15%; observer 2, 15%). The Cohen kappa indicated good agreement between the 2 observers for the study group and was not calculated for the control group because of the congruence of the observations.
The higher percentage of vertebral defects in the TMC patients scored by observer 1 was statistically significant with respect to those scored in the controls ( P <0.05) ( Table I ). The same was true for observer 2 ( P <0.05), as suggested by the high concordance of the observations.
| Group | Defects | No defects | Total |
|---|---|---|---|
| Sample | 29 | 11 | 40 |
| Control | 6 | 34 | 40 |
| Total | 35 | 45 | 80 |
The types of defects in the study group were concavity of the posterior border and rounding of the anterosuperior, posterosuperior, and anteroinferior angles of the vertebral body. In the control group, only rounding of the anterosuperior angle was found. The most common defect in the study group according to both observers (observer 1, 57%; observer 2, 63%) was rounding of the anterosuperior angle of the vertebral body.
The vertebrae of the TMC patients with the most defects were C4 (observer 1, 34%; observer 2, 32%) and C5 (observer 1, 24%; observer 2, 42%). Both observers noted that the most common defect was rounding of the anterosuperior angle (observer 1, 46% in C4 and 29% in C5; observer 2, 35% in C4 and 45% in C5) ( Table II ).
| Sample | Control | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Observer 1 | Observer 2 | Observer 1 | Observer 2 | |||||||
| Type of defect | Vertebra | Number of defects | Total | Number of defects | Total | Vertebra | Number of defects | Total | Number of defects | Total |
| Anterosuperior angle | C3 | 9 | 35 | 5 | 40 | C3 | 2 | 6 | 2 | 6 |
| C4 | 16 | 14 | 4 | 4 | ||||||
| C5 | 10 | 18 | C4 | |||||||
| C6 | — | 3 | ||||||||
| Anteroinferior angle | C2 | 8 | 11 | 1 | 2 | |||||
| C3 | 2 | — | ||||||||
| C4 | 1 | — | ||||||||
| C5 | — | — | ||||||||
| C6 | — | 1 | ||||||||
| Posteroinferior edge | C3 | 2 | 15 | — | 20 | |||||
| C4 | 4 | 7 | ||||||||
| C5 | 5 | 9 | ||||||||
| C6 | 4 | 4 | ||||||||
| Posterosuperior angle | C3 | — | — | 2 | 2 | |||||
| Total | 61 | 64 | ||||||||
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


