Maxillary deficiency is a common feature in patients with repaired cleft lip and palate. Orthognathic surgery has been the conventional approach for the management of cleft-related maxillary hypoplasia. However, for patients with a severe maxillary deficiency, orthognathic surgery alone has many disadvantages, such as high relapse rates of 25% to 40%, instability, limited amount of advancement, and a highly invasive surgical technique. As an alternative treatment method, distraction osteogenesis has been used successfully in the distraction of the mandible, the maxilla, the entire midface, and the orbits as well as the cranial bones, with stable outcomes. The type of distraction device, either external or internal, can be chosen based on the surgical goals set for the patient. In this study, we report on the use of a rigid external distraction device for maxillary advancement in a 22-year-old woman with a repaired unilateral cleft lip and palate and severe maxillary hypoplasia. After the distraction osteogenesis, 2-jaw surgery was performed to correct the maxillary yaw deviation and the mandibular prognathism.
Highlights
- •
Distraction osteogenesis (DO) can be an efficient treatment modality in the management of cleft-related maxillary hypoplasia because it promotes correction of both the bone and the soft tissue simultaneously.
- •
Even in cases in which orthognathic surgery is inevitable, performing DO beforehand could reduce the amount of surgical movement during the surgery.
- •
If a proper distraction vector is applied and overcorrection with regard to relapse and good retention is accomplished, DO can be used successfully in the treatment of cleft patients.
Cleft lip and palate (CLP) are common congenital deformities in the oromaxillary area. Patients with orofacial clefts commonly have maxillary hypoplasia that is caused by the cleft itself, the patients’ genotype, or scarring from early surgical intervention. Early surgical corrections usually are performed to improve esthetics and function, but these early surgeries tend to result in poor skeletal and dental growth in the transverse and anteroposterior planes in the maxilla. Moreover, the maxillary dentition is often collapsed because of missing teeth. A systematic approach is thus required for patients with CLP; these often include surgery, growth modification, and comprehensive orthodontic treatment.
The selection of a proper treatment method for patients with CLP and severe maxillary hypoplasia is complicated because of palatal scar contracture, upper lip tension, and decreased postoperative stability from large anteroposterior discrepancies. Distraction osteogenesis (DO) has become an alternative technique for the correction of craniofacial skeletal dysplasias. Since the initial clinical trials on humans by McCarthy et al, in which a hypoplastic mandible was elongated, Figuero and Polley have reported success using DO to advance the maxilla in growing patients with CLP with no significant complications. More recently, the mandible and the maxilla, the entire midface, and the orbits have been successfully distracted.
The purpose of this article was to report the use of a rigid external distraction (RED) device for maxillary advancement in a 22-year-old woman with CLP and severe maxillary hypoplasia. The 2-jaw surgery was performed after the DO to correct the maxillary yawing and the mandibular prognathism.
Diagnosis and etiology
The patient was a Korean woman whose chief complaints were a concave profile and mandibular prognathism. She was born with a complete unilateral CLP and received a cheilorrhaphy and a palatorrhaphy when she was 10 years old. There was no history of orofacial congenital anomalies or deformities in her family. She had no other relevant medical history.
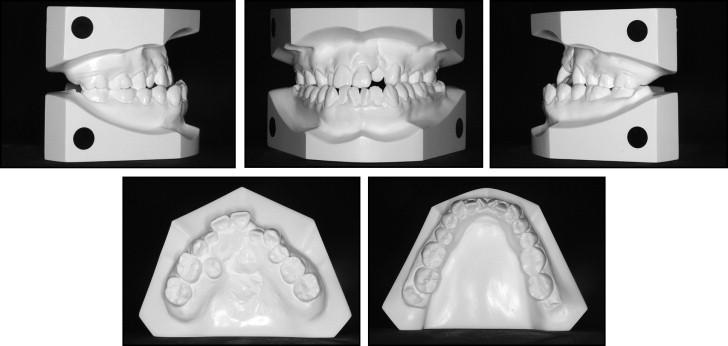
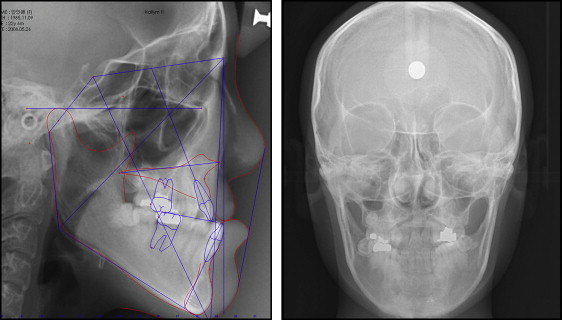
The extraoral examination showed a midface deficiency and an increased mandibular body length. Lower facial height was comparatively longer than midfacial height. The length of the mental region was much greater than that of the upper lip ( Fig 1 ). The intraoral examination showed an Angle Class III molar relationship with an anterior crossbite and a maxillary yaw deviated to the right. She was missing her maxillary second premolars, and her maxillary right first premolar had a palatal ectopic eruption. Her maxillary dental midline was deviated by 3 mm to the right of the facial and mandibular dental midlines. She had peg laterals ( Fig 1 ). Her study models showed an anterior Bolton ratio of 82.41% and a 1.54-mm mandibular excess ( Fig 2 ). The panoramic radiographs showed that the original cleft defect was in the maxillary left lateral incisor area ( Fig 3 ). The cephalometric analysis showed a skeletal Class III relationship with a retrusive maxilla and a hyperdivergent skeletal pattern. The Z-angle indicated a concave profile with a retrusive upper lip. Both the maxillary and the mandibular incisors were retroclined ( Fig 4 , Table ).


| Measurement | Mean | Initial | After DO (3 mo) |
Posttreatment | 2 years posttreatment |
|---|---|---|---|---|---|
| SNA (°) | 81.6 | 72.10 | 76.86 | 77.66 | 76.98 |
| SNB (°) | 79.10 | 78.92 | 76.02 | 73.68 | 74.04 |
| ANB (°) | 2.40 | −5.15 | 0.84 | 3.99 | 2.91 |
| A-point to N-perpendicular (mm) | 0.40 | −10.93 | −3.82 | −3.53 | −3.57 |
| FMA (°) | 24.20 | 32.18 | 31.97 | 31.55 | 32.07 |
| Sum of angles (saddle angle + articular angle + gonial angle [°]) | 393.3 | 400.5 | 401.71 | 398.72 | 399.32 |
| Wits appraisal (mm) | −2.70 | −11.47 | −1.64 | −3.76 | −3.90 |
| Mandibular body length (mm) | 78.00 | 83.03 | 83.50 | 76.04 | 76.16 |
| U1 to SN (°) | 107.0 | 103.52 | 100.11 | 98.70 | 100.13 |
| U1 to FH (°) | 116.0 | 111.72 | 109.82 | 107.87 | 108.37 |
| IMPA (°) | 95.9 | 82.17 | 82.94 | 90.24 | 89.64 |
| Upper lip to E-plane (mm) | −1.00 | −9.02 | −5.4 | −0.14 | −0.89 |
| Lower lip to E-plane (mm) | 2.00 | 0.77 | 1.46 | 2.38 | 1.60 |
Treatment alternatives
Based on those objectives, 2 treatment options were suggested.
- 1.
Combined orthodontic and surgical treatment that included maxillary advancement with posterior impaction and mandibular setback.
- 2.
Combined orthodontic and distraction osteogenesis treatment with orthognathic surgery. The maxillary advancement would be performed with DO followed by orthognathic surgery to posteriorly impact the maxilla and set back the mandible.
Considering the severity of the skeletal discrepancy, the second option was chosen as a potentially more stable treatment method. The RED device was planned to be used to accomplish the maxillary DO.
Treatment progress
Active treatment by DO was divided into 3 phases: predistraction phase, distraction and consolidation phase, and postdistraction phase. In the predistraction phase, the intraoral appliance for the RED device was fabricated to apply traction force to the maxilla using the maxillary dentition as the anchorage. Orthodontic bands were fitted on the maxillary second molars before the maxillary impression. The intraoral device was made by soldering the bent stainless steel orthodontic wire (0.90 mm diameter) that crossed both the labial and palatal sides of the maxillary dentition, making 1 point of contact with every tooth. Vertical wires with hooks were soldered perpendicular to the labial wire, positioning these extraoral wires just medial to the oral commissures ( Fig 5 ). Two additional short vertical wires with hooks were also soldered to the labial wire at the position of the canines. This permitted the use of the same intraoral appliance with a facemask after removal of the extraoral wires during the consolidation phase.
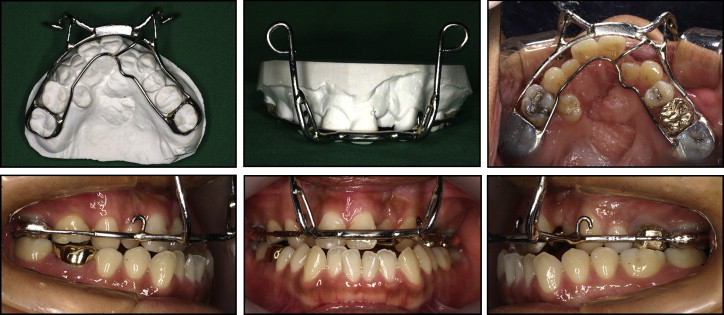
In the distraction and consolidation phases the patient was hospitalized and a complete maxillary osteotomy without down-fracture was performed in preparation for the distraction. A RED system was attached to the cranium with 3 screws on each side. The extraoral hooks of the maxillary intraoral device were tied to the vertical pin of the RED device ( Fig 6 ). After a latency period of 8 days, distraction commenced at the rate of 0.5 mm twice per day and continued for 10 days. The intraoral device was maintained during the 8 weeks of the consolidation period.





