Fig. 17.1
(a) Preoperative radiograph of a persistent infection on the first lower mandibular molar. (b) Postoperative radiograph after the retreatment. (c) A 6-month follow-up radiograph showing signs of healing
Why Does Nonsurgical Root Canal Treatment Fail?
It is of paramount importance to understand the main reasons why nonsurgical root canal treatment fails if the clinician wishes to prevent further occurrences of failure and to optimize the likelihood of successful retreatment. The main causes of endodontic therapy failure include: poor technical quality of the previous treatment; the occurrence of procedural errors such as overfilling, underfilling, perforating, missing canals, and breaching the infection control protocol; and inadequate sealing of the root canal system by the permanent restoration (Fig. 17.2). Dugas et al. [20] concluded that the periapical health of root-filled teeth in two Canadian populations was influenced by the quality of both the root filling and the restoration, with the impact of the latter being most critical when the quality of the root filling was adequate. The study also stated that the prevalence of periradicular disease in root-filled teeth did not differ between teeth treated by general dentists and endodontists.
Fig. 17.2
A 36-year-old presented with pain to biting on the mandibular first molar. Nonsurgical root canal treatment and a restoration had been completed 3 years prior to this painful episode. Note the incomplete root canal treatment with a radiolucency surrounding the mesial root
Reports of endodontic failure in cases in which the highest standards of care were followed are prevalent in the literature [42, 63]. Factors beyond the clinician’s control, such as a complex root canal system with areas that cannot be cleaned and filled adequately with the instruments and techniques that exist today [25, 35, 45, 46], in combination with the presence of extra-radicular infections [53] are typically the main cause of failure in these cases. Scanning electron microscopic analysis of the apical foramen and external radicular surfaces performed by Signoretti et al. [61] revealed microbial communities embedded in a polysaccharide matrix in a protein-rich environment called a biofilm.
This chapter will briefly focus on three main causes of endodontic failure, as missing canals, vertical root fractures, and infections are the most frequently encountered scenarios.
Missing Canals
Irrigation can play an important role when attempting to locate hidden canal orifices. When used to irrigate the pulp chamber floor, sodium hypochlorite will allow “champagne bubbles” to form in the location of these canals which can then be scouted with a sharp explorer. Magnifying loupes and a dental operating microscope may also increase the likelihood of visualizing the location of canal orifices [31] (Fig. 17.3).
Fig. 17.3
(a) Preoperative radiograph showing both first and second maxillary molars with under-filled canals. Patient was percussion sensitive on tooth 27; (b, c) proper access opening under magnification and illumination allowed negotiation of the second mesial-buccal canal on tooth 27; (d) gutta-percha fit; (e) Temporary filling with Glass Ionomer; (f) postoperative radiograph of the retreatment in both 26 and 27
Vertical Root Fracture
Traumatic injuries, restorative procedures, and the excessive removal of tooth structure during endodontic procedures are the main causes for vertical root fracture. Usually, it is diagnosed years after all endodontic and prosthetic treatments have been completed. The diagnostic process for cases of vertical root fracture is often frustrating. It is based on the combination of the patient’s subjective complaints and on an objective clinical and radiographic evaluation. Evidence-based data concerning the diagnostic accuracy and clinical efficacy of the objective clinical and radiographic dental evaluation for the diagnosis of vertical root fracture in endodontically treated teeth is lacking [72]. The most common signs and symptoms of vertical root fracture, as described in the literature, are the presence of deep osseous defects especially on the buccal aspect of susceptible teeth and roots and a cervically located sinus tract [69]. Endodontically treated teeth with an expected vertical root fracture typically have a poor prognosis and extraction should be considered (Fig. 17.4).
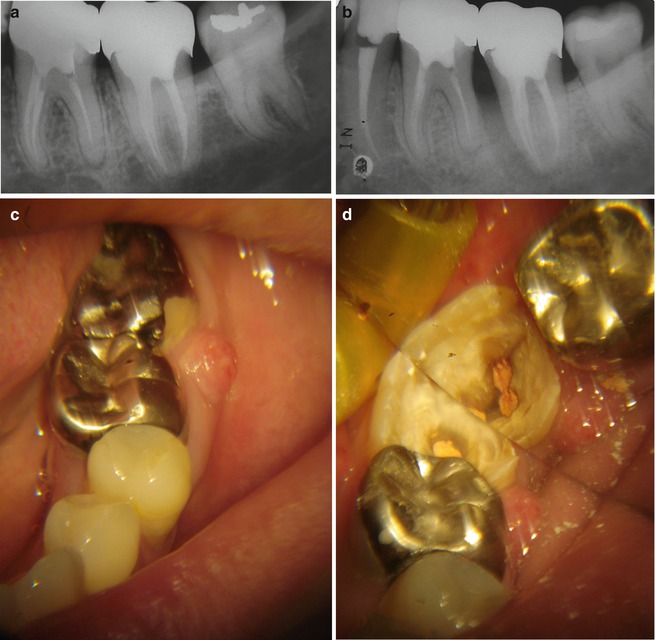
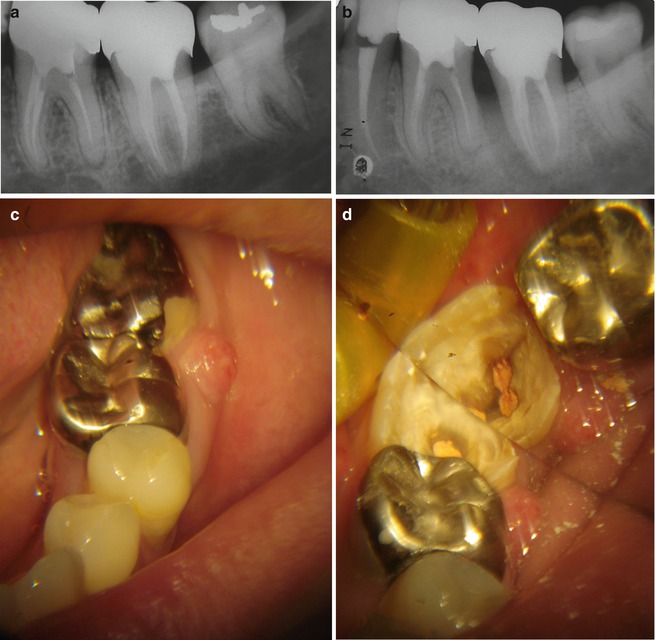
Fig. 17.4
(a) A 46-year-old patient had a nonsurgical root canal treatment concluded and a metallic crown was placed immediately after; (b) after a little more than 3 years, the patient complained of a throbbing pain and pressure on the left lower jaw. A halo-shaped radiolucency surrounding the mesial root could be seen suggesting the possibility of a vertical root fracture; (c) clinically there was a sinus tract close to the gingival margin between the first and second mandibular molars (36 and 37). At this point, a deep narrow pocket was observed in the mesial aspect of the 37; (d) once the crown is removed, the fracture is easily visualized
Infection
A periradicular inflammation may not respond to endodontic treatment due to the persistent nature of the infection. This occurrence is known as persistent disease. It is also possible for a new lesion to appear as a result of the introduction of bacteria into a canal during the treatment process, usually due to either a breach in the infection control protocol or in cases of coronal leakage. This scenario is known as emergent disease. Even after complete healing has occurred, a lesion can reappear after a period of time. This phenomenon is classified as recurrent disease or a late failure [73].
Even though studies have shown that endodontic infections are biofilm-related [10], Enterococcus faecalis has been identified as the single most commonly recovered species from teeth with persistent endodontic infections. Yeasts, archaea, and viruses can also be found as part of the microbial diversity of these infections [62].
Success Rate of Nonsurgical Retreatment Cases
Despite the fact that endodontic retreatment has a lower success rate when compared to orthograde treatment [57], according to Salehrabi and Rotstein [58], endodontic retreatment is a procedure with a very good survival rate and patients can be advised that 89 % of these teeth may be retained and functional for at least 5 years after the procedure. The potential for healing is improved if the previous filling material is removed safely and effectively and if patency can be achieved during the retreatment procedure. De Chevigny et al. [15] analyzed the outcome 4–6 years after retreatment was rendered to identify significant outcome predictors that could be determined preoperative such as: root-filling quality, previous perforation, and periradicular radiolucency. In teeth that had an associated radiolucency, the significant outcome predictors included the number of treatment sessions and the previous root-filling quality. The retreatment outcome was seen to be better in teeth with an inadequate previous root filling that did not have a perforation or an associated radiolucency. Gorni and Gagliani [28] differentiated the success rate of retreatment cases into two groups: one in which canal and apical morphology alterations had occurred and the other in which the previous treatment had not lead to adverse alteration of the original morphology. The authors discovered that the success rates differed between the two groups as a higher rate of success resulted when the natural course of the root canals was maintained during the previous endodontic treatment.
Removal of Filling Material
Gutta-percha, in combination with numerous endodontic sealers, is the most widely used material for root canal filling. Effective removal of gutta-percha in endodontic retreatment is necessary in order to obtain access to infected areas of the root canal system. Thorough removal is a significant factor in the successful retreatment of a previously failed procedure as it allows for the irrigating solution to come in contact with the canal walls and work effectively. Gutta-percha removal can be time consuming and can cause fatigue that may lead to procedural errors that put the success of the retreatment in jeopardy [27]. Oval and long-oval root canals offer an additional challenge to the removal of the previous filling material; there is a tendency to keep the file in the center of the canal, which does not allow adequate preparation in the buccolingual dimension [40, 50, 74, 77]. When previous filling material is not completely removed, it acts as a barrier, preventing the irrigating solution from touching the canal walls. Retention of the filling material also harbors necrotic tissue and microorganisms responsible for endodontic treatment failure.
Cunha et al. [14] assessed the obturation removal in canals filled with Resilon/RealSealTM (Pentron Clinical Technologies) in comparison to canals filled with gutta-percha/AH Plus in extracted teeth. The obturations were removed from both groups using chloroform, irrigating with 2.5 % NaOCl, and manual re-instrumentation. The teeth were then radiographically analyzed. Specimens without obturation material remnants visible during radiographic examination were selected for analysis under scanning electron microscopy. The Resilon/RealSealTM system was seen to be removed in greater quantities from the canal walls compared with the gutta-percha cones and the AH PlusTM (Dentsply Maillefer) cement. Scanning electron microscopy revealed material remnants in all portions of the canal. Again, Resilon was seen to be better removed from the canal than the gutta-percha cones and the AH PlusTM.
ProTaper UniversalTM (Dentsply Tulsa Dental), MtwoTM (VDW), and d-RaCeTM (FKG Dentaire) are systems that have instruments specifically designed for removing the previous filling material from the root canal. Takahashi et al. [68] evaluated the efficacy of these nickel-titanium rotary instruments used with or without a solvent versus the use of stainless steel hand files for gutta-percha removal in extracted teeth. The results showed that there was no significant difference between the two techniques in regard to the amount of endodontic filling remnants; however, the ProTaper UniversalTM rotary retreatment system without chloroform was found to be faster. Numerous studies have continued to evaluate filling material removal using different techniques and file systems. Conventional NiTi rotary files can also be used to remove root-filling material from previously treated root canals with the added advantage of avoiding the removal of excessive tooth structure as frequently occurs when using Gates-Glidden drills (Fig. 17.5). Zuolo et al. [82] compared the efficacy of reciprocating and rotary techniques with that of hand files for removing gutta-percha and sealer from root canals of extracted teeth. The remaining endodontic filling material was observed on the canal walls of all teeth regardless of the technique used. However, hand files combined with Gates-Glidden burs and the use of the reciprocating technique removed more filling material from the canal walls in comparison to the rotary files. Rios et al. [54] assessed the efficacy of 2 reciprocating systems in comparison to a nickel-titanium (NiTi) rotary system in the removal of root canal filling material from canals of extracted teeth. Again, all of the teeth examined had filling remnants within the canal and no significant difference among the file systems was found. Solmonov et al. [65] used a 25.06 ProFileTM (Dentsply Tulsa Dental) instrument followed by the Self-Adjusting FileTM (SAF; ReDent Nova) and found this sequence to be less time consuming and more effective at removing the root-filling residue in the canal in comparison to the use of ProTaper UniversalTM files for this purpose (Dentsply Tulsa Dental).
Fig. 17.5
Remnants of gutta-percha threaded in the active portion of a NiTi rotary instrument (ProTaper Universal, Dentsply Tulsa Dental) during the desobturation step
The numerous studies mentioned confirm that it is almost impossible to completely remove the filling material from inside the root canal, and even in cases where this material cannot be seen radiographically, it can be assumed that remnants are still present in areas such as isthmuses, fins, and lateral canals (Figs. 17.6 and 17.7)
Fig. 17.6
(a) A mesial root of a mandibular molar was shaped and filled with gutta-percha and sealer; (b) the attempt to completely remove the filling material failed as it was still seen inside the isthmus between both canals at the end of the procedure using a micro-CT scanner
Fig. 17.7
(a) A three-dimensional image using a micro-computed tomography scanner of a mandibular molar mesial root showing both MB and ML filled with gutta-percha and sealer; (b) after the desobturation procedure, filling material remnants can still be seen on the canal’s walls
In recent years, the predictability of surgical and nonsurgical endodontic procedures has benefited from the combined use of the dental operating microscope (DOM), which allows for improved optics for magnification and illumination, and specially designed ultrasonic tips. Protocols using both devices have been proposed for cases in which nonsurgical retreatment is indicated as they allow for improved precision due to enhanced illumination and magnification. The combination of these devices is especially useful during the removal of filling remnants. De Mello Jr. et al. [17] compared the efficacy of gutta-percha/sealer removal from extracted endodontically treated teeth with and without the aid of a dental operating microscope used in conjunction with ultrasonic instruments. Despite the fact that all teeth had remnants of filling materials at the end of the retreatment, the average amount of remaining gutta-percha/sealer was significantly lower when both devices were used. The remnants of filling materials compacted against the root canal walls after using drills, files, and solvent can easily be removed using ultrasonic instruments due to the cutting efficiency of the piezoelectric oscillation. Grischke et al. [29] compared the efficiency of sonic, ultrasonic, and hydrodynamic devices in the removal of a root canal sealer from the surface and simulated irregularities of root canals. Again, the passive ultrasonic irrigation was seen to be effective in removing sealer from the root canal.
During endodontic therapy, dental instruments may separate within the root canal and impede the renegotiation of the canal path. As such, during radiographic examination in preparation for retreatment, the clinician may unexpectedly encounter one or more retained endodontic instrument fragments. In clinical studies, the incidence of this accident has been reported to range from 0.39 % to 5 % [18, 51].
In a systematic review, Panitvisai et al. [48] assessed the prognosis of teeth after instrument fracture during endodontic therapy and found no statistically significant difference in healing rates between teeth with and without retained instrument fragments. However, the odds of treatment failure are higher when fragments prevent a thorough cleaning and shaping of the entire canal system and when periradicular lesions are present preoperatively [13, 33, 66]. When infection is present, removing or bypassing the fractured instrument is essential to ensure that the irrigation solution reaches the working length in order to obtain disinfection and the associated increased predictability of the outcome. Dental operating microscopes (DOM) and ultrasonic tips have allowed clinicians to obtain access to separated instruments and can assure higher success rates in the removal of instrument fragments, as reported by [43].
Carrier-Based Filling Materials
Carrier-based filling materials provide a straightforward approach to the obturation procedure; however, removal of these materials can be particularly challenging especially when retreating small and curved canals as the plastic core is not soluble in common solvents [4] (Fig. 17.8).
Fig. 17.8
(a) A 48-year-old patient had a nonsurgical root canal treatment where the obturation was performed using a carrier-based technique in all four canals. A 7-year follow-up radiograph showed a periradicular lesion in both mesial and distal roots; (b) during the attempt to retrieve Thermafil from inside the canals, a ledge and subsequent perforation occurred in the mesial-buccal canal. The carrier inside the distal-lingual canal separated at the apical portion; (c) even though a portion of the previous obturation material was kept inside the canals and the perforation inside the mesial-buccal canal perforation, the treatment was concluded and the final restoration was placed; (d) a 10-month follow-up showed signs of healing and the patient was asymptomatic. Despite the technical difficulties in this case, the disinfection protocol was essential for a successful outcome
More recently, a 3rd generation of carrier-based obturators named GuttaCoreTM (Dentsply Tulsa Dental) was developed and employs cross-linked gutta-percha instead of a plastic carrier. According to a recent research study, this system is easier to remove than those containing plastic carriers [7, 44] (Fig. 17.9).
Fig. 17.9
Two specimens representative of root-filling material remnants that remained covering the walls after retreating root canals previously filled with (a) GuttaCore and (b) Thermafil
Solvents: How Effective/Safe Are They?
The use of mechanical techniques and solvents to remove filling materials from previously root canal-treated teeth has been tested throughout the years [9, 11, 68]. The assertion that usage of an organic solvent is necessary for the removal of filling material can be considered inappropriate as several published articles demonstrate both root-filling remnants on the root canal surface and the formation of an artificial smear layer after using these agents [55, 64] (Fig. 17.10). A further disadvantage is the cytotoxic property of organic solvents, which is especially of concern when they are extruded into the periradicular area [5, 60].
Fig. 17.10
Artificial smear layer adhered to the canal’s walls after the usage of chloroform during an endodontic retreatment in a mandibular lower premolar
Solvents were studied more frequently in the 1980s and 1990s than they are in the present period [30, 70, 76]. Barbosa et al. [5] examined the effects of halothane, turpentine oil, and chloroform solvents on the fibroblastic cells of rats. These authors concluded that the use of solvents should be avoided because all of the agents analyzed were found to be toxic.
In certain cases, the hardening of the sealer is accentuated to such a degree that it is very difficult to remove the gutta-percha in its entirety or even establish a glide path through the gutta-percha, especially in curved canals [30, 70].
A consensus has not yet been reached regarding whether solvents are helpful during the process of gutta-percha removal. Despite this uncertainty, the issue of the cytotoxicity of the solvents used in endodontic retreatment needs to be analyzed more accurately. Although chloroform is generally considered highly effective, the claim that it is cytotoxic has led to the testing of some “alternative” solvents, such as halothane, eucalyptol, orange oil, and xylene [24, 59]. Wilcox [75] and Bueno et al. [9] have reported that chloroform is highly efficient. Recently, a similar study was performed by Sağlam et al. [56] in extracted molars with curved roots. The ProTaper Universal and Self-Adjusting File were used in conjunction with chloroform, Endosolv, or no solvent and the residual root-filling material was evaluated using micro-computed tomography (μCT), a noninvasive technology. No significant differences were found between the groups in terms of the percentage volume of residual root canal filling.
Regarding solvent cytotoxicity, McDonald and Vire [39] found that chloroform had no effect on the clinical staff or on the patient who had undergone the treatment involving chloroform. In addition, it was reported that if used under normal conditions, chloroform does not cause any irreversible cytotoxic effects. Chutich et al. [12] analyzed the toxicity of chloroform, halothane, and xylene by quantifying the apically extruded solvent and found that the amount of solvent that was carried through the apical foramen is much lower than the permitted dose. Nevertheless, the US Food and Drug Administration (FDA) specify that chloroform may not be used as an ingredient in drug products or in pharmaceutical compounding.
Fruchi et al. [26] used μCT imaging to evaluate the amount of filling material remaining after instrumentation with reciprocating files and again after passive ultrasonic irrigation (PUI) with xylene. The study concluded that both instruments efficiently, but not completely, removed the filling material from the inside of the curved mesial-buccal canals of extracted maxillary molars. Although the use of xylene with PUI slightly increased the removal of the filling material, this finding was not statically significant. Cavenago et al. [11] evaluated the percentage of remaining filling material in the mesial root canals of mandibular molars after retreatment in which 3 procedures were performed sequentially. The first step involved removal of the filling material, enlargement of the root canals to size 40, and instrumentation with a 0.04 tapered instrument. In the second step, the root canals were irrigated with xylene and an attempt was made to clean the root canals with paper points. In the third step, the PUI technique was performed using 2.5 % sodium hypochlorite. The authors concluded that the filling materials were not completely removed by any of the retreatment procedures alone; however, the use of xylene and PUI after mechanical instrumentation enhanced removal of the materials during endodontic retreatment of anatomically complex teeth.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


