Introduction
The temporomandibular joint (TMJ) is a complex joint that often develops degenerative joint disease. Clinical examination alone cannot usually diagnose this accurately, and a radiographic examination complements and aids in diagnosis and treatment. The osseous components of the TMJ complex are best imaged using computed tomography. The evolution of cone-beam computed tomography (CBCT) offers a low radiation dose and a high spatial resolution alternative and is becoming the imaging modality of choice for the TMJ. To further reduce the dose and yet not compromise the diagnostic task at hand, some alternative rotation acquisition protocols are available but have not been adequately evaluated. The aim of this study was to evaluate the diagnostic efficacy of 2 CBCT acquisition protocols to detect degenerative changes associated with the TMJ complex.
Methods
Thirty-four TMJs, from 17 dry human skulls, were obtained from the anatomy department at the School of Dental Medicine of the University of Connecticut. The sample consisted of complete dentate and partially dentate skulls with no identifiable markers such as age, sex, or ethnicity. Small and large lesions simulating early and established arthritic changes were created on the mandibular condyle. Each defect was randomly created on the medial pole, articulating surface, or lateral pole. After simulating the articular disc with rubber dam material, the condyle and the glenoid fossa were articulated and positioned in place by a rubber band. The skulls were scanned by using an Accuitomo CBCT scanner (J. Morita Corp, Kyoto, Japan) with 180° and 360° rotation protocols. Two operators scored the lesions and compared the results to the gold standard, which was the master list of where the lesions were made on the condyles.
Results
On the 102 randomly selected sites, 39 large and 33 small lesions were made, and the rest of the sites had no lesions. The detection rates for areas with large lesions and areas with no lesions were 100% between the examiners. However, of the 33 small lesions, each examiner was able to identify 32 of them with the 360° scans: a 97.4% detection rate when compared with the gold standard. With the 180° scan, 94.9% of the small lesions were detected when compared with the gold standard, and 96.9% were detected with the 360° scan. The overall interexaminer reliability was over 90% for both imaging protocols (Cronbach’s alpha, 92.4% for 180° and 97% for 360°).
Conclusions
Based on the results of this study, the 180° CBCT acquisition protocol can detect small and large arthritic lesions with high reliability and is comparable with the 360° spin acquisition.
Highlights
- •
We evaluated the diagnostic efficacy of 2 CBCT protocols for degenerative changes in the TMJ.
- •
The skulls were scanned by using 180° spin and 360° spin protocols.
- •
The 180° protocol detected small and large arthritic lesions with high reliability.
The temporomandibular joint (TMJ) is a diarthrodial joint, comprising the mandibular condyle, temporal bone, and articular disc, and is regarded as one of the most complex joints in the body. TMJ disorders (TMDs), or temporomandibular dysfunction, is a collective term; these disorders may affect the masticatory muscles, the TMJ and its associated structures, or both. It has been estimated that as many as 10 million people in the United States suffer from TMDs, which are a major health problem.
Degenerative diseases of the mandibular condylar cartilage are the most frequent pathologic conditions that affect the TMJ. Osteoarthritis of the TMJ is characterized by erosion of cartilage that has become soft, frayed, and thinned, resulting in eburnation of the subchondral bone and outgrowth of marginal osteophytes. TMJ bony changes result in flattening of the articular surfaces and subchondral sclerosis, and these changes are commonly seen in the mandibular condylar cartilage during initial and advanced degenerative diseases.
Clinical examination of TMDs is insufficient to fully assess the osseous and soft-tissue changes in the mandibular condylar cartilage, and the need for TMJ imaging is usually determined at an individual level after a thorough history and clinical examination. The goals of TMJ radiography are to assess the extent and monitor the progression of degenerative changes, and to evaluate the response to treatment. Panoramic radiography, conventional linear or complex motion tomography, and computed tomography (CT) are usually used to assess the osseous components of the joints, whereas magnetic resonance imaging is used to assess the soft-tissue components (discs). CT has been found to be superior to plain films and magnetic resonance imaging, with 87% to 96% accuracy in detecting early degenerative changes in the mandibular condylar cartilage. For the radiologic diagnosis of degenerative changes of the mandibular condylar cartilage, reliability is poor for panoramic radiography, fair for magnetic resonance imaging, and excellent for CT.
Cone beam CT (CBCT) provides high-resolution multiplanar images and delivers a substantially lower radiation dose than multislice CT. CBCT allows examination of TMJ anatomy without superimposition and distortion to facilitate analysis of joint morphology, joint space, and dynamic function in all 3 dimensions. CBCT provides a definitive advantage over other radiation techniques because of its low radiation dose to the patient and its ability to provide multiplanar reformation and 3-dimensional (3D) images.
The radiation dose is an important factor when ordering a scan for a patient, especially in the head and neck region. Compared with panoramic radiography, multislice CT and CBCT radiation dosages vary widely between modality, equipment, exposure, and field-of-view parameters. The radiation dose varies from 3.85 to 38 μSv for panoramic radiography, from 429.7 to 1160 μSv for multislice CT, and from 27 to 674 μSv for CBCT. Different imaging parameters influence the radiation dose, but using a smaller volume size generally reduces it and should always be chosen if the smaller volume will answer the clinical question.
Typically, a CBCT scan is acquired with a 360° rotation of the x-ray source and detector combination around the area of interest. During the rotation, the scanner acquires multiple basis projections of the area of interest. At postprocessing, the reconstruction puts together this information using convoluted algorithms such as the Feldkemp algorithm to reconstruct a 3D image. Although the basis projections are developed from acquiring information by going around in 360°, a similar image data set can be developed using “filtered back projection,” where the data can be gathered with a 180° rotation around the area of interest. With radiation dosage a major factor to be considered in a diagnostic test and its efficacy, we conducted this study to compare the efficacy of a 180° rotation with that of a 360° rotation in diagnosing early arthritic changes such as those in the mandibular condylar cartilage of the TMJ. We hypothesized that by decreasing the scan rotation from 360° to 180° we could maintain acceptable diagnostic accuracy of the TMJ’s bony structures and achieve a significant dose reduction. Currently, a 360° rotation is the gold standard and provides excellent visualization of the different components of the TMJ, but it exposes the patient to about twice the radiation of a 180° rotation. In addition, a 180° scan cuts the acquisition and processing times as well as the size of the scans, and it is an option that is available already in most of commercially available CBCT scanners.
Material and methods
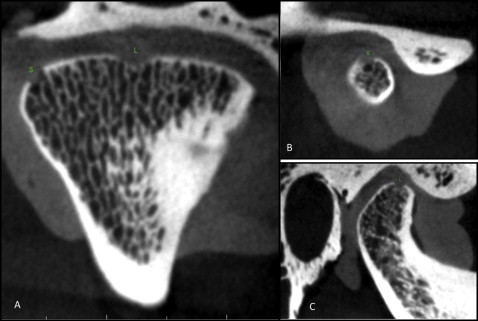
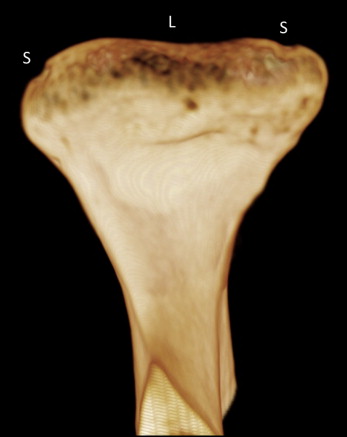
Thirty-four TMJs, from 17 dry human skulls, were obtained from the anatomy department at the University of Connecticut School of Medicine and Dental Medicine. The sample consisted of complete dentate and partially dentate skulls with no identifiable markers such as age, sex, or ethnicity. Since most early arthritic osseous changes occur on the condyle of the mandible, defects were designed to simulate erosive, saucer-shaped lesions similar to those of early arthritic changes ( Fig 1 ). The mandibular condyles were randomly assigned a defect on 3 possible surfaces: medial pole, articulating surface, and lateral pole of the condyle. On each surface, we either made a small or a large lesion or left it intact as the control ( Fig 1 ). A skilled orthodontist (S.Y.) using a dental drill with a round bur made all the lesions. The lesions were classified as small at 1 to 2 mm in diameter and 0.1 to 0.5 mm in depth, or as large with a diameter between 1.5 and 3 mm and a depth between 0.5 and 1.5 mm. To simulate the soft-tissue anatomy in the area and to diminish the contrast, white utility wax was used. The wax was placed between the glenoid fossa and the condyle as well as around the joint. A small piece of dental rubber dam was laid on top of the condyle to prevent the wax from filling in the lesions. Latex gloves filled with water were also placed in the brain cavity of each skull to simulate brain tissue and to provide more tissue attenuation. The condyles were laid in the appropriate position guided by the natural occlusion of the teeth by aligning the mandibular and maxillary teeth and the application of light force. For each skull, 2 CBCT scans were made with a large field of view (140 × 40 mm): one with a 180° rotation and one with a 360° rotation (34 scans). The 180° and 360° scans were taken at the same time using the same setup; the only thing that changed was the rotation of the scanner, to keep the 2 images controlled. The CBCT scans were taken with a 3D Accuitomo CBCT scanner (J. Morita Corp, Kyoto, Japan). The scans were obtained at 80 Kvp and 5 mA with a focal spot size of 0.5 mm. The image acquisition times were 17.5 seconds for the 360° scans and 9.0 seconds for the 180° scans. The images were randomly assigned numbers, and an oral and maxillofacial radiologist (A.T.) and an orthodontist (S.Y.) blindly evaluated the images. The images were viewed using the i-Dixel (J. Morita Corp) acquisition program. The examiners initially reviewed 10 scans and were calibrated in terms of interexaminer reliability. Upon analysis, each analyst viewed the images independently and marked whether there was a lesion. If a lesion was present, the analysts also marked its size by the scans, although the effect of correct size detection had no major clinical relevance. These results were then compared with the original documents of the known lesions and subjected to statistical analysis.
Statistical analysis
Statistical analysis was conducted using a Web-based program from Social Sciences Statistics (J. Morita Corp; www.morita.com ) to compare the statistical significance of our results that were not due to chance alone. The interexaminer reliability was calculated using the Cronbach alpha test. The sensitivity and specificity of the 2 scanning protocols for small and large lesions were recorded as percentages and compared with the McNemar test. The difference between the gold standard (as initially created) and the 2 acquisition protocols as well as between the 180° and 360° protocols was calculated using the 2-tailed Student t test.
Results
Of the 102 possible sites for examination that were randomly selected, 39 had large defects, 33 had small defects, and 30 were free of defects ( Fig 1 ). The overall interexaminer reliability values were over 90% for both imaging protocols (Cronbach’s alpha, 92.4% for 180° and 97% for 360°). The overall sensitivity values for the total number of defects were 96.5% and 98.6% for the 180° and 360° protocols, respectively ( Figs 2-4 , Table ). The specificity for both acquisition protocols was 100% ( Table ). The Table summarizes the sensitivity and specificity values for the 180° and 360° acquisition protocols in all areas. Although the average detection rate for the small defects was significantly lower than that for the large defects, there was no marked difference between the 180° and 360° protocols ( P = 0.749). Our findings were further confirmed with the McNemar test ( P = 0.25) ( Fig 1 ).