Chief complaint
Complaint in patient’s own words
Medical history
Medical causes of symptoms
Medical condition: complexity in managing a patient
Psychological condition: complexity in managing a patient
Undiagnosed medical condition
Dental history
Recent dental treatment
Dental trauma
Patient history
Pain scale
Characterization
Temperature sensitive
Percussion sensitive
Reproducible
Location
Duration
2.3 Chief Complaint
A chief complaint is the reason a patient seeks care. It is important for the patients to express this in their own words and for this to be recorded. A clear understanding of a patient’s motivation for seeking care and of their expectations will help alleviate confusion and avoid breakdown in the dentist–patient relationship. It should be noted that a patient could possibly have additional dental disease that they are not seeking care for at that particular appointment. Once a patient’s chief complaint has been managed, it is incumbent upon the dentist to make a patient aware of the potential for additional problems.
2.4 History of the Chief Complaint
Several important aspects of the diagnostic process can be elicited from the history of a patient’s chief complaint. As the Victorian physician Sir William Osler once said, “If you listen to your patients, they will tell you their diagnosis.” While it is essential to have the patient complete a written medical questionnaire, it is important to follow this up with an oral interview. A study has indicated that the questionnaire medical history was significantly deficient in 4.25 % of cases [2].
There are three principle components to the history of a chief complaint:
-
Dental history
-
Medical history
-
Pain history
With regard to the pain history, this aspect of the interview should be directed at identifying the presence or absence of pain, the nature (constant or intermittent pain) and quality of pain if present, and the region of the pain. A thorough assessment of pain is essential in differentiating between odontogenic and non-odontogenic pain. Various pain qualities and characteristics can help delineate between these two origins of pain. Thus, information that relates to pain is essential. It should include the ability to localize to a specific tooth; spontaneous pain; provoking factors (tenderness to hot, cold, sweet, sour, chewing); interference with sleep; relieving factors (use and effect of drugs; ice water); character of pain (sharp, dull, throbbing, irradiating); duration of pain; referred or radiating pain; a feeling that the tooth is extruded; presence of swelling and possible relationship to pain; fever; malaise; presence of pus; impaired mouth opening. A visual analog pain scale or a pain rating scale is useful in establishing a patient’s level of pain. It is also valuable in establishing a baseline that can subsequently be used to refer back to in assessing the degree to which the pain has been alleviated. It should be recalled that pain of pulpal origin is more likely to be described as sharp and lingering whereas pain from the periradicular origin is more frequently described as dull pain.
2.5 Dental History
It important to enquire if a patient has had any recent dental treatment or injuries. A “broken tooth” as a result of caries can frequently result in a near pulp exposure or pulpal exposure proper.
2.6 Medical History
There are no medical conditions that are contraindicatory to the provision of endodontic treatment. There are, however, conditions that require consultation with the patient’s other health care providers and additional management during endodontic treatment. The major purpose of a medical history is fourfold:
-
To rule out possible systemic or medical causes for the patients symptoms.
-
To identify medical conditions that might increase the complexity of managing a patient.
-
To identify a psychological condition that might increase the complexity in managing a patient.
-
To potentially identify undiagnosed medical conditions that would increase the complexity of the treatment.
A patient medical history should be updated regularly and include a patient’s vital signs and a review of systems. This is considered standard of care.
2.7 Odontogenic Versus Non-odontogenic Pain
It is important for the clinician to identify developing non-odontogenic pain as early as possible in the development of the process. Frequently, such pain will become chronic and debilitating in nature. Furthermore, this pain can be further exacerbated by incorrect or unnecessary treatments, often resulting in the establishment of chronic pain pathways. The site of pain is where the patient feels the pain and this can differ dramatically from the source of pain. The source is the structure from which the pain actually originates. Pain with distinctive sites and sources of pain are known as heterotopic pain [3]. Heterotopic pain can be separated into three types [4]:
-
Central pain
-
Projected pain
-
Referred pain
Two aspects are thus important in the management of these conditions: one is to establish a correct diagnosis as soon as possible and the second is the importance of avoiding unnecessary treatment. The aim, from the perspective of this chapter, is not to establish a diagnostic schematic for all pain in the facial region, but rather to provide the practicing clinician with an approach to the diagnostic process that will facilitate two things. Firstly, it allows the clinician to differentiate between odontogenic and non-odontogenic pain. Secondly, if it is odontogenic in origin, it provides the clinician with a process to either establish the pain as endodontic in origin; that is, pulpal pathology or secondary to pulpal pathology with additional periradicular pathology (Box 2.2). It is important to realize that pain of endodontic origin can at times be extremely intense and debilitating; it is typically short in duration (weeks as opposed to months or years) that will either become focused on a particular tooth or dissipate only to return at a later date.
Box 2.2: Characterization of Pain
|
Tooth pain
|
Non-tooth pain
|
|---|---|
|
Temperature sensitivity
|
Chronic
|
|
Percussion tender
|
Stabbing
|
|
Deep
|
Shooting
|
|
Dull
|
Burning
|
|
Aching
|
Multiple locations
|
|
Sharp
|
Absent of obvious pathology
|
|
Specific
|
Headache
|
|
Throbbing
|
Trigger points/zones
|
|
Reproducible
|
Altered by psychological stress
|
|
Unilateral
|
Pain, when present, is obviously an indicator of some form of disease. Pain in the mid and lower facial regions can be confusing for patients and they are often unsure as to whether they should consult a doctor or dentist. By far, one of most common causes of pain in the mid and lower face is pain of dental origin. Epidemiologic studies indicate that toothache is the prevalent form of pain in the orofacial region, with approximately 12–14 % of the population reporting a history of toothache in the preceding 6-month period [5]. Odontogenic pain usually results from either one of two structures associated with the tooth; the pulpal or periodontal tissues. Analysis of patients attending dental practices and hospitals for emergency treatment of pain in the facial region show that the more common causes of this pain are acute periapical periodontitis, irreversible pulpitis, reversible pulpitis, pericoronitis, and dentine hypersensitivity [6]. These disorders of the teeth typically cause toothache and/or pain in the orofacial region. Classic headache, as such, is an infrequent symptom associated with tooth pathology. However, pain from the teeth can be referred and can cause a diffuse type headache. Klausen et al. [1] reported a particular combination of signs and symptoms that are distinctly associated with pulpal degeneration in approximately 85 % of cases. The signs and symptoms included constant pain, sensitivity to temperature changes, an extruded feeling in the tooth, impaired mouth opening, mobility, and tenderness to palpation in the apical area. These signs and symptoms in various combinations were highly accurate predictors of odontogenic disease. Temperature sensitivity was highly indicative of pulpitis; on the other hand, pain due to apical periodontitis is often associated with digital pressure or percussion tenderness. In a similar study using a descriptor survey, patients could be correctly classified into one of three diagnostic categories in approximately 90 % of cases [6]. The important keys to differentiating between odontogenic and non-odontogenic pain are severity, location, quality, and duration. Notably, pain of pulpal or periradicular pathology secondary to pulpal pathology should resolve completely with local anesthesia. Pain that does not resolve following the administration of local anesthetic should raise a very strong suspicion of pain of non-odontogenic origin.
One of the hallmarks in differentiating odontogenic and non-odontogenic pain is its chronicity. It should be noted that few dental causes of pain are truly chronic in nature. However, given its high prevalence, it needs to be considered in all patients who report a history of chronic pain or who report a change in their symptoms of chronic pain, which are not expected from the main condition. Chronic orofacial pain patients will frequently have seen several health care providers in an effort to treat their pain. In 100 consecutive patients referred to oral and maxillofacial surgeons for pain assessment that was not due to odontogenic causes, patients had frequently seen more than three practitioners in an effort to resolve their symptoms; 44 % had either extractions or endodontic treatment in an unsuccessful attempt to treat their orofacial pain [7]. In patients referred to an endodontic specialty practice, 88 % of patients had solely an endodontic problem, 9 % had an endodontic problem plus a separate orofacial pain problem, and 2.2 % primarily had a non-tooth-related problem [7]. It was concluded that tooth pain is the most common type of orofacial pain for which patients seek dental treatment.
It is useful for the individual dentist to develop a system or checklist [8] to help with the diagnostic process. One approach is to attempt to classify craniofacial pain into one of several categories. These include neurovascular, neuropathic, muscular, intracranial pathology, referred from other pathological conditions, local pathology, and those that do not fit into the preceding categories. Understanding the types of pain in these categories will help eliminate them as a possible etiology. Furthermore, by identifying a possible etiological category, the clinician is able to direct the patient to the appropriate specialty to provide a definitive diagnosis. For an extensive review of non-odontogenic orofacial pain, the reader is referred to one of several texts, including Orofacial Pain: Guidelines for Assessment, Diagnosis and Management [4, 9, 10]. What follows is a description of the more common cause of non-odontogenic toothache [3].
2.8 Common Source of Non-odontogenic Toothache
2.8.1 Muscular
Temporomandibular pain and muscle disorder pain is reported in approximately 10–15 % adults [11]. Approximately 7 % of cases referred for endodontic treatment have a myofascial “toothache” [12]. Furthermore, 37 % of patients diagnosed with muscular orofacial pain have previously undergone endodontic treatment or tooth extraction in an effort to relieve their pain [7]. Myofascial pain that mimics a toothache is typically described as diffuse, deep, dull, nonpulsating, aching pain that occurs more continuously than pulpal pain. Many of these qualities are, however, similar to pulpal or periradicular pain. Chewing can also exacerbate the symptoms, which may confuse the diagnostic process. Key to differentiating the origin of the pain here is that palpation of the musculature should reproduce pain of myofascial origin while percussion of the teeth should elicit a normal response. Additionally, pulp testing will be normal or fail to reproduce the reported symptoms. Radiographically, the lamina dura may be thickened and the PDL space widened due to increased bruxism and clenching. Typically, muscles that refer pain to the teeth include the masseter, temporalis, medial pterygoid, lateral pterygoid, and the anterior digastric. It can also be associated with emotional stressors.
2.8.2 Sinus or Nasal Structures
Pathology of the nasal and sinus mucosa can frequently present as a toothache emanating typically from the posterior maxillary teeth. About 10 % of maxillary sinusitis cases have been diagnosed as having an odontogenic origin [13]. They may or may not be accompanied by additional symptoms consistent with sinus involvement such as nasal congestion or drainage. The hallmarks that generally differentiate these conditions from tooth pain include increased pain sensation when a patient touches their toes, several teeth in the same side in the maxilla that are tender to percussion, pulp testing that have normal responses to thermal or electric pulp tests,; and a lack of radiographic evidence of periradicular pathology.
2.8.3 Neurovascular
Pain of this origin can have qualities of intensity and pulsation comparable to pulpal pain. The patient will frequently complain of “headache” symptoms with “toothache” being a secondary complaint. Three types of headaches fall into this category, migraines, cluster headaches, and tension headaches. The typical referral pattern of neurovascular headache is to the maxillary anterior and premolar teeth. The temporal nature of these types of headaches is also a key factor in differentiating them from tooth pain. The pain is frequently very intense for 4–72 h followed by periods of complete remission. The symptoms are not typically provoked by the usual stimuli of toothache such as hot, cold, and chewing. Thus, pulp testing would typically produce a normal response. Furthermore, radiographic analysis of the teeth in the region of the pain would reveal no obvious pathological change. The use of local anesthetic as a diagnostic aid can be misleading in these patients. The periods of intense headache pain are often associated with photophobia or phonophobia occurring in approximately 60 % of patients. This tends to be unilateral. Nausea and vomiting has also been reported in approximately 30 % of patients. It has been reported that 36 % of patients have had teeth extracted in an attempt to treat the pain [14]. Additionally, the pain may switch from one side to the other between attacks or cluster periods and this is particularly uncommon in pain of tooth origin. However, the short duration of attacks, recurrences, excruciating intensity and pulsatile pain quality found in neurovascular headache make it possible to mistake this source of pain for pulpitis [15]. Approximately, 42 % of cluster headache patients have received some form of irreversible dental procedure in an attempt to alleviate their pain [15]. It should be noted that the prevalence of migraine headaches affects about 12.5 % of the general population in the United States. It is also the most widespread cause for disability from headache.
2.8.4 Neural
Neuropathic pain is caused as a result of abnormalities associated with the actual neural structure and not from the tissues that are innervated by those neural structures. Thus, there is typically no structural pathology evident. Neuropathic pain that is felt in teeth can be either episodic or continuous. Clinically, episodic neuropathic toothache presents as a severe, shooting, electric-like pain that lasts only a few seconds. Continuous neuropathic pain usually presents as constant, ongoing, and unremitting pain. It can have periods of high and low intensity, but none of total remission [3]. In patients with continuous neuropathic pain, 79 % had undergone dental treatment that failed to resolve their pain [16]. Several different forms of neuropathic pain exist and these include neuralgia, neuritis, and neuropathy. The more common types include trigeminal neuralgia, herpetic neuritis, and neuropathy secondary to injury or sensitization of the neural structures.
The classic type of neuralgic pain in the orofacial region is trigeminal neuralgia. Trigeminal neuralgia is characterized by episodic intense sharp shooting unilateral pain. Stimulating a trigger zone, typically with light touch or airflow, can reproduce the pain. The duration of the pain is up to several minutes and does not occur again until the trigger zone is re-stimulated. A trigger zone can be in any region of the distribution of the nerve and so may be extraoral or intraoral. Demographically, trigeminal neural is usually present in patients 50 years or older; it is also more common in females than males. Although neuralgic pains may closely mimic acute toothache of pulpal origin, pulpal and periradicular testing is normal or not definitively conclusive. There is also a lack of dental pathology present. Additionally, neuralgias rarely wake patients once they are asleep.
Herpetic neuritis typically is not a diagnostic challenge once the skin or mucosal vesicular outbreak occurs. However, prior to vesicular eruption or if the viral infection involves deep neural branch, diagnosis can be more difficult. Key to diagnosis is a history of herpes zoster infection. Additionally, the pain quality is also described as aching, dull, and burning. It should be recalled that burning is not a common descriptor used for pain of tooth origin. Pulpal and periradicular testing is usually normal or not definitively conclusive. There is also a lack of dental pathology. Patients may also exhibit a decreased threshold response to non-noxious stimulation.
2.8.5 Cardiac
Classic cardiac pain usually originates in the sub-sternal region and radiates to the left neck, shoulder, arm, and left mandible. Angina pain can occasionally also mimic dental pain in the left mandible. Patients with pain of a cardiac origin reported the descriptor of “pressure” more often when compared to other pain sources [17]. Critically, this pain will not be intensified by local stimulation of the teeth. Furthermore, pulpal and periradicular tests will be normal and radiographic findings negative. Local anesthesia of the left mandible will not reduce the symptoms. Craniofacial pain is the only symptom in approximately 6 % of patient that have cardiac ischemia. One study also reported that bilateral referred craniofacial pain was also observed approximately six times more often than unilateral pain [18]. Additionally, a patient may not necessarily report a medical history of cardiac disease.
2.8.6 Neoplasia
Orofacial pain may be the initial symptom of oral cancer or metastatic disease. According to the National Institute of Health in the United States, approximately 10.5 adults per 100,000 will develop oral cancer [19]. A retrospective case series found that pain was the first clinical sign of oral cancer in 19.2 % of cases [6]. A study of neoplasia of the tongue reported that two-thirds of patients with oral cancer reported oral pain within the preceding 6 months of diagnosis [20]. Systemic cancers such as lymphoma and leukemia can have an intraoral presentation that mimics toothache symptoms. Metastatic neoplasia to the jaw is rare with 1–3 % of all malignant oral neoplasias being metastatic. The common primary sources for the metastases to the oral region are the breast, lung, and kidney. The mandible is the most common location of the metastases, with the molar region being more commonly involved [21]. Although rare, patients with multiple myeloma can develop osseous osteolytic lesions adjacent to teeth. When this occurs, odontogenic pain is common and presents a radiologic diagnostic challenge [22]. In metastatic disease of the jawbones, pain has been reported in 39 % and paresthesias in 23 % of patients [23]. A retrospective case series of metastatic disease in the jaws reported that in 60 % of patients, oral signs and symptoms from a metastatic lesion in the jaw were the first indication of an undiscovered primary malignancy at a distant site [24].
2.8.7 Non-somatoform
The mental health of a patient is important in assessing facial pain. Chronic facial pain can affect a patient’s mental health or can lead to an increase in the severity of pain experienced by the patient. Mental health conditions such as depression and anxiety can have a significant effect on their pain experience [11]. Neural markers for fear and anxiety have been shown to increase with chronic pain. Mentally overwhelmed patients show an increased distress and disability from pain. Additionally, a number of studies intimate a significant role of psychological factors such as anxiety and depressive disorders in inexplicable somatic symptoms. The prevalence of nonspecific somatoform symptoms is higher in psychologically distressed patients than in the general population. True psychogenic or somatoform pain is rare and is typically arrived at as a diagnosis by a process of elimination. This is cognitively perceived pain that has no verifiable corporeal basis. The key features of this type of pain are chronic pain from multiple locations that may not be anatomically connected, pain that does not follow anatomical distribution of the peripheral nerves, pain with no identifiable etiology and pain that frequently changes in character. In patients where such a condition is suspected, referral to a psychiatrist should be made.
2.9 Clinical Exam
Broadly speaking, the clinical exam is comprised of an extraoral exam and an intraoral exam.
2.9.1 Extraoral Exam (Box 2.3)
Box 2.3: Extraoral Exam
|
Asymmetry
|
|
Eyes
|
|
Cognizant
|
|
Facial paralysis
|
|
Lymph nodes
|
|
Joint sounds
|
|
Muscle palpation
|
|
Range of opening
|
|
Soft tissue damage
|
|
Swelling
|
The extraoral exam should begin with a basic observation of the patient during the initial introductory conversation. Several important pieces of information can be gleaned during this time, much of which we do during the course of a conversation with any individual. In the dental setting, however, they become more critical. Firstly, patients should be cognizant of their surroundings, fluent in their speech, and be able to understand and make the choices that they are likely to encounter during the examination. Secondly, the patient should be evaluated for any apparent asymmetry, facial paralysis, or facial soft tissue damage including changes in skin tone, discoloration, redness, scarring, or ulceration. If any of these abnormalities exist, they should be pursued with the patient for further clarification. A classic example of this would be an extraoral sinus tract of odontogenic origin. In cases like this, a patient might present a history of unsuccessful medical treatments that can range from drug therapy to surgical intervention.
Palpation of the extraoral soft tissues is useful in determining the extent of the facial swelling and the involvement of lymph nodes. If the initial history is indicative of pain of a muscular origin, then palpation of the muscle of mastication to identify trigger points is appropriate. All patients should be observed for range of motion in jaw opening, joint sounds, and deviation of the mandible to the left or right during opening. A limited jaw opening might not only be indicative of non-odontogenic source of pain, but also could increase the degree of difficulty in delivering endodontic treatment.
The clinician should also be cognizant of nonverbal cues for pain. These include the obvious signs such as crying, facial grimacing; but also include subtler signs such as a clenched jaw, positioning the face or head to avoid stimulating the symptoms. A classic example of this would be the patient that enters the office with a container of ice-cold water that they continue to periodically sip to relieve tooth pain.
2.9.2 Intraoral Exam (Box 2.4)
Box 2.4: Intraoral Exam
|
Soft tissue assessment
|
Narrow angle probing
|
|
Mobility
|
|
|
Periodontal probing
|
|
|
Periodontal pocketing
|
|
|
Gingival recession
|
|
|
Bleeding on probing
|
|
|
Hard tissue assessment
|
Cuspal biting
|
|
Caries
|
|
|
Defective restoration
|
|
|
Excessive wear
|
|
|
Fractured tooth
|
|
|
Stained tooth
|
|
|
Palpation test
|
Apex of teeth
|
|
Muscle of mastication
|
|
|
Pulp test
|
Cold
|
|
EPT
|
|
|
Heat
|
|
|
Periradicular test
|
Percussion
|
|
Central fossa biting
|
|
|
Radiographic assessment
|
The intraoral exam should take the approach of all clinical examinations moving from an initial broad examination that gradually becomes more focused on a specific region or problem. This approach will ensure that several important aspects of the clinical exam are not overlooked. It guarantees that the patient’s general oral health is assessed and key elements of the diagnostic process are not neglected. An examination of the patient’s hard and soft tissue structures should be made and any abnormalities noted. Once the dentist has ruled out the presence of any serious pathology not related to the patient’s chief complaint that requires immediate attention, the intraoral exam can begin to focus on the problem as defined in the patient’s chief complaint. This should include an assessment of the immediately adjacent soft and hard tissues, presence of decay, tooth restorability, periodontal apparatus status, and specific tests related to periradicular and pulpal assessment.
2.10 Restorability
It can be said that root canal therapy can be performed on just about any tooth. However, subsequent restoration of the tooth to an ideal form and function is much less certain. Careful consideration should be given to the final restoration as part of the diagnosis and treatment planning steps. It is frustrating for all involved if an endodontically treated tooth is subsequently deemed nonrestorable.
Studies have suggested that the long-term prognosis for an endodontically treated tooth is more dependent on the coronal restoration than on the quality of the endodontic treatment itself [25]. Moreover, it has been demonstrated that loss of the coronal seal will result in a rapid recontamination of the root-canal-treated tooth [26].
In recent years, there has been a major change in philosophy regarding the restoration of endodontically treated teeth (see also Chap. 7 in this book). Researchers and clinicians have begun to realize the importance of respecting the preservation of tooth tissue and the biological properties of the components of the tooth, namely enamel, dentin, and cementum. It can be argued that this pendulum of change may have swung a little too far in the opposite direction with the move toward minimalist canal preparations. In an ideal world, minimal tooth tissue would be removed while achieving all of the goals of debridement, disinfection, and obturation. Four variables could improve the survival rate of endodontically treated teeth [27]. These are:
-
Provision of crown restoration after endodontic treatment.
-
Maintenance or replacement of mesial and distal proximal contacts.
-
That the tooth itself is not an abutment for either a fixed or removable partial denture.
-
That the tooth is not a molar tooth.
Before commencing endodontic treatment, the clinician must consider a number of factors regarding the restoration of the tooth.
-
Altered physical properties of tooth tissues following endodontic treatment.
-
How much dentin will remain following caries and/or restoration removal and access cavity preparation.
-
The existence of a fracture/crack and the extent of the fracture/crack.
-
What functional demands will be placed on the restored tooth.
-
Will it be feasible to ensure that the biologic width can be respected when the new restoration is placed.
-
Can an ideal embrasure space and emergence profile be restored or maintained.
Much has been written about the structural integrity and strength of the endodontically treated tooth. It is widely believed that endodontically treated molar teeth are more prone to fracture for a number of reasons:
-
Weakening of the tooth due to loss of tooth tissue (especially loss of marginal and transverse ridges) [28]. Photoelastic and finite element analysis studies have demonstrated this fact repeatedly.
-
Alteration in the physical properties of the tooth due to the effects of caustic irrigants such as hypochlorite and ethylene diamine tetraacetic acid [16]. It is believed that up to 30 % of the ultimate tensile strength of the dentin is provided by the collagen, which undergoes significant changes after root canal treatment.
-
Microbial factors: effects of bacteria–dentin interactions [29].
-
Restorative factors: effect of post-core restorations.
-
Age factors: effect of age changes on dentin [29].
Historically it was believed that the lack of pulpal blood supply renders dentin more brittle due to drying out; however, studies have relegated these theories to the realms of unsound mistaken beliefs [30, 31]. Instead, the structural integrity of the tooth is compromised as soon as any tooth tissue is removed [32]. In addition, intracanal irrigants, medicaments, and obturation materials may also play a role in influencing the physical and mechanical properties of dentin.
Endodontically treated molar teeth present the clinician with their own unique set of difficulties. The same principles, which govern the restoration of any tooth, also apply to the restoration of endodontically treated teeth. It is, however, especially important to preserve as much of the remaining tooth tissue and to design the restoration in a way that distributes stress in the most favorable manner. Traumatic occlusion is also well recognized as a source of endodontic failure and steps must be taken to minimize occlusal stresses [33].
It often happens that the tooth requiring endodontic treatment is severely broken down resulting in occlusal and proximal loss of space. This problem can sometimes be addressed by orthodontic treatment, intrusion of the opposing tooth, or recontouring adjacent restorations. A lack of coronal tooth tissue can be managed in a number of ways. If it is possible to encompass the tooth with a cast restoration extending onto solid tooth structure by at least 2 mms then the longevity of the restoration is more predictable; this is called the ferrule effect [34]. In some cases it may be necessary to crown lengthen the tooth in order to achieve this effect. In the absence of sufficient coronal tooth tissue, it may be possible to gain retention from the root. This tends to be more favorable in molar teeth than in other teeth due to the morphology of the teeth. Provision of posts or dowels cannot be routinely recommended especially in molars; rather, the use of the pulp chamber to retain a core is preferable. Further discussion of the techniques and materials will be discussed in the chapter on restoration in this book.
2.11 Endodontic–Periodontic Relationship
It is not surprising that pulpal and periodontal disease processes are closely related considering the close embryological relationship between the tissues. Both tissues are derived from a common mesodermal source. The pulpal precursor, the dental papilla, is separated from the periodontal tissue precursors by the Hertwig’s epithelial root sheath. Both diseases have their terminal effects in the periodontal tissues [35]. Simring and Goldberg [36] first described this relationship and coined the term “endo-perio.” Simon et al. then attempted to codify the nature of the diseases and described five distinct categories [37]:
-
The primary endodontic lesion
-
The primary endodontic lesion with secondary periodontic involvement
-
The primary periodontic lesion
-
The primary periodontic lesion with secondary endodontic involvement
-
The true combined lesion (both lesions present and have joined in periradicular tissues)
Belk and Gutmann [38] suggested a sixth category and called this the “concomitant lesion.” This describes the situation where both endodontic and periodontal lesions exist but are wholly independent of each other. Establishment of the correct diagnosis is crucial to provision of the correct treatment. This is frequently difficult to establish but especially so in multirooted teeth for a number of reasons. Molar teeth are morphologically complex and are often difficult to image due to their locations and surrounding structures such as the zygomatic arch on upper teeth and mandibular tori on the lower. They have multiple canal spaces complicating vitality testing; some canal spaces may maintain vitality while others become necrotic. They are associated with more vertical root fractures than anterior and premolar teeth. In addition, molars are frequently heavily restored making interpretation of testing and radiographs more difficult.
A diagnosis is based on taking a thorough history and full clinical exam as stated earlier. When a clinician suspects a possible endodontic–periodontal lesion a complete assessment of the pulpal and periodontal status of the tooth must be established. The essential components of this assessment include:
-
History of periodontal symptoms both locally and generally (bleeding, mobility, infections)
-
History of dentinal, pulpal, or periapical pain
-
Signs and symptoms of pulp/periapical disease
-
Periodontal charting
-
Radiographic pattern of marginal and periradicular bone loss
Collecting the necessary information at the clinical exam necessitates using the full array of investigative methods and techniques including radiographic examination, vitality testing, periodontal probing, sinus tract tracing, fiber-optic illumination, percussion and palpation, and mobility determination.
Harrington emphasized the importance of detailed diagnostic periodontal probing [39]. His assertion was that a lesion of periodontal origin demonstrates a generalized gradual change in probings as opposed to one of endodontic origin that usually manifests as a precipitous drop or narrow-based probing. Accurate pulpal assessment is essential when periodontal disease is involved. The status of the pulp is crucial in establishing the correct diagnosis in the endo–perio scenario. If the pulp is healthy, then the lesion is totally periodontal in origin. If the pulp is necrotic, the periodontal apparatus has the capacity to regenerate following root canal treatment.
2.12 Sinus Tract
Whenever present, a sinus tract should be traced, especially if the sinus opening is distant from any obvious pathology. The simplest method for tracing a sinus is to utilize a gutta-percha cone, typically a size #30 or greater to avoid buckling of the cone within the tract and giving erroneous impressions of the source (Fig. 2.1). The opening of the sinus tract and gutta-percha cone can be coated with topical anesthetic and introduced into the sinus tract opening or stoma. The gutta-percha cone will progress into the sinus tract toward the offending region of pathology. In the majority of cases a coating of topical anesthetic will be sufficient to trace the sinus tract; only occasionally a patient may have to be anesthetized to achieve a successful tracing.
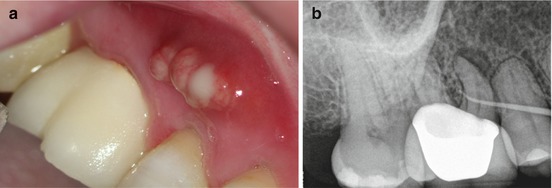
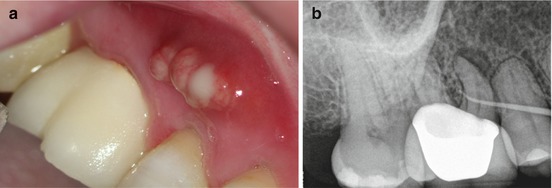
Fig. 2.1
(a) Clinical photography of a sinus tract adjacent to the maxillary second premolar tooth. (b) Radiograph of the same area showing the presence of a gutta-percha tracer in the sinus tract leading toward the periradicular radiolucency associated with the mesial root of the first molar tooth
2.13 Diagnostic Tests
Prior to initiating any specific diagnostic tests, it is critical to inform the patient of the nature of the test, what to expect, and how to respond. All diagnostic tests should also be carried out in an order that establishes a base line level of a normal response for each patient. This is best done by first testing a “normal” contralateral tooth. The teeth on either side of the tooth that is primarily expected to be the source of the symptoms should then be tested. Finally, the tooth that is suspected as being the offending tooth should be tested last. As stated, it is imperative that the dentist and patient fully understand how to communicate the results of the test before commencing testing. In the case of thermal testing, a system of defined hand signals is often the most effective method for a patient to communicate their response. Typically, a patient would be directed to raise their hand when they feel the sensation from the stimulus in the tooth, to keep their hand up as long as this sensation lingers, and to lower their hand when the sensation ceases. It is important to advise a patient on differentiating between feeling a thermal change in their mouth and a sensation (pain) in their tooth. The authors feel that there is no place for the use of “test cavities” to determine vitality of a tooth.
2.14 Sensibility Testing: Pulpal Testing
Sensibility testing (thermal and electric) is central to the establishment of a correct pulpal diagnosis. However, all pulp tests have limitations and these must be recognized [40]. A positive response to pulp testing, thermal or electric, only confirms the existence of functional neural tissue. Conventional pulp testing does not indicate the presence of normal healthy pulpal tissue with a normal blood flow. Furthermore, pulp tests are even less likely able to indicate the degree of health of the pulp. Thus, most pulp tests are only assessing the pulp sensitivity, rather than pulp vitality. Histological studies (specifically silver staining histological studies) have demonstrated that the neural component of the pulp is the last component of the pulp to undergo necrosis. Thus, false positive and false negative responses can and do occur. In general, cold and electric tests appear to be more dependable tests than heat. As a rule, it is important to use a test that will reproduce the patient’s symptoms. Thus, if eating or drinking cold food produces or escalates the symptom, then a cold test should be used. Likewise, if hot foods produce or escalate the symptom, then a heat test should be used. Teeth should then be tested in an order that establishes a base line level of a normal response for each patient as described above. Teeth should be tested approximately 15 seconds (s)apart. This gives time for the tooth to respond and allows for a delayed response from a given tooth. In some instances, more time may be needed between testing of individual teeth and waiting to see if symptoms occur in a delayed manner. To perform a pulp test on any given tooth, it should be dried of saliva and the soft tissue retracted with the aid of cotton rolls or a dental mirror. The stimulus should then be applied to the buccal aspect of the mesial cusp or to the cervical region. Teeth that do not respond on the occlusal area respond approximately 14 % of the time when stimulated in cervical area [41]. It is important to compare the immediacy, the intensity, and duration of the response from different teeth within the same patient.
2.15 Thermal Testing
The pulp tissue contains neural fibers along with blood and lymphatic vessels, extracellular matrix, ground substance, and all of the other components of a normal connective tissue. These fibers are either of the A or C type; A (Aβ or Aδ) are well-developed myelinated fibers that are fast conducting and operate in the normal healthy pulp tissue. On the other hand, the C fibers are more primitive, non-myelinated slow-conducting fibers located in the core of the pulp that tend to be active only in inflamed pulp. The C fibers are slow to respond to stimulation, but once they begin to respond, they tend to continue to send impulses to higher cortical centers. Clinically, application of cold or heat that provokes a long-lasting response is one that is stimulating the C fibers, indicating the presence of active C fibers in inflamed tissue. This, therefore, determines a pulpal diagnosis of irreversible pulpitis. Additionally, thermal stimuli cause contraction or expansion of fluids inside the dentinal tubules. The hydrodynamic forces generated act on the Aδ nerve mechanoreceptors of the pulp, causing a short sharp pain indicative of a normal pulp. The results obtained with the use of thermal stimulation (heat or cold) are particularly important because of its ability to reproduce the patient’s chief complaint. A response that lingers for more than 15–20 s after the thermal stimulus has been removed is frequently interpreted as indicating an irreversibly inflamed pulp. No response from the patient to a thermal stimulation can be regarded as an indication of a necrotic pulp. Obviously a diagnosis should not be accomplished on the basis of a single test. Selecting between cold and heat testing is based on a patient symptomology; a complaint of heat sensitivity would indicate a heat test should be preformed. In a patient that does not report a history of thermal pain, a cold test should be used first due to its simplicity and reliability. Some teeth with irreversible pulpitis may need repetitive stimuli to achieve the threshold that causes pain. It is also important to recognize that once a tooth has been stimulated thermally, there can be a refractory period of several minutes before a second cold or heat stimulation can provoke the same response.
2.15.1 Cold
Cold testing is technically the simplest pulpal test to perform. It can be accomplished by using one of several different cold stimulus including ice sticks (~0 °C), ethyl chloride (~ −5 °C), frozen carbon dioxide (~ −75 °C), or a pressurized refrigerant spray containing either 1,1,1,2 tetrafluorethane, or dichlorodifluoromethane (~ −26 °C). Although all of these methods have been successfully demonstrated, refrigerant spray applied to a small cotton pellet is the best at achieving a predictable low temperature in a convenient and efficient manner. It is also significantly more effective than either an ice stick or ethyl chloride. Cold stimulus should be applied to a tooth until the patient definitively responds or for a maximum of 15 s.
In some instances, cold can relieve a patient’s pain. Typically, these patients will present with a container of ice-cold liquid that they will periodically sip to relieve their pain. In these patients, application of cold to the individual offending tooth will eliminate the pain, thus allowing the dentist to make a diagnosis of irreversible pulpitis. Concerns about potential damage done to porcelain restorations or enamel have been dismissed [42].
2.15.2 Heat
Heat testing is not typically the first test performed; however, it may be indicated if a patient reports heat sensitivity as part of their chief complaint or when other tests fail to establish enough information to make an accurate diagnosis. The simplest and most practical way of performing a heat test is to use gutta-percha softened in a flame or with an electric heat carrier. The application of the heat stimulus to a tooth should not last for more than 5 s in order to prevent permanent pulpal damage. From this perspective, it is important to use a separating medium, such as Vaseline, so that the heated gutta-percha does not stick to the tooth being tested. Alternatively, a rubber dam can be applied to each tooth to be tested individually and hot water can be flowed around the tooth. This allows for isolated testing of individual teeth.
2.16 Electrical Pulp Test
Electric pulp testing (EPT) is based on the stimulation of sensory nerve fibers within the pulp. Electric pulp testing does not give any information on the degree of health or disease of a pulp. A positive response is merely an approximate indicator of the presence of vital neural fibers in the pulp. It entails a subjective evaluation from the patient. The basic principle of the electric pulp tester is to deliver a high-frequency direct electric current through the tooth. The electrical stimulus, like other pulp testing techniques, is best applied to the enamel of the buccal surface of the mesiobuccal cusp. A small amount of a conducting agent such as toothpaste should be applied to the tip of the testing probe. When the probe is applied to the tooth, the level of electric current transmitted through the tooth gradually increases. The operator sets the rate at which the current increases. The electrical circuit needs to be completed by placing the connecting sensor in contact with the patients’ soft tissue. This can be accomplished by either placing the sensor on the patient’s bottom lip or by having them hold the sensor. Having the patient hold the connecting sensor to discontinue the EPT circuit gives the patient more control over the process and may result in more reproducible test results. It can be difficult to use on crowned teeth; an additional smaller probe may be required to stimulate the tooth structure apical to the crown margin. Care must also be taken not to stimulate the soft tissues in this situation. The EPT is useful in older patient or in teeth that have undergone pulp canal obliteration/mineralization where cold stimulus may be insufficient to provoke the remaining neural tissue [43].
The use of EPT in patients with surgically implanted pacemakers has been controversial; early animal studies indicated that EPT could cause interference in the pacemaker [44]. Since the time of this study, pacemakers have continued to undergo development. In vitro studies carried out in the 1980s and 1990s have indicated no interaction between pacemakers and EPTs [45–47]. In a 2006 study in patients with implanted cardiac pacemakers or cardioverter/defibrillators, the use of a simulated EPT did not produce any interference effects [48].
2.17 Pulpal Testing Accuracy
In considering the accuracy of a pulpal test, it is important to have an understanding of the rate of disease with the general population. The prevalence of non-endodontically treated teeth with periradicular disease in the general population as defined by the presence of periradicular radiolucency is approximately 2 % of all teeth [49]. Additionally, 5.4 % of the patients reporting to an emergency room presented with a dental problem not associated with trauma [50]. The presence of frequent pain in the region of the mouth in the general population is approximately 5–14 % [51]. The prevalence of pulp disease in patients seeking treatment for pain in the facial region in an endodontic specialty practice has been shown to be as high as 88 %.
Traditionally, terms used to describe the accuracy of a diagnostic test (pulp testing) are sensitivity and specificity. Sensitivity (true positive rate) is the rate at which a test correctly predicates a diseased state; that is, the number of diseased pulps as indicated by a test divided by the actual total number of diseased pulps. Specificity (true negative rate) is the rate at which a test correctly predicates a healthy state; that is, the number of healthy pulps as indicated by a test divided by the actual total number of healthy pulps. Thus, a test can have four predicative results: true positive: diseased pulps correctly diagnosed as diseased pulps; false positive: healthy pulps incorrectly identified as diseased pulps; true negative: healthy pulps correctly identified as healthy pulps; and false negative: diseased pulps incorrectly identified as healthy. Part of the difficulty in accessing accuracy of pulp testing is that the same test is used to identify several different states of health and disease of the pulpal tissue. The fact that thermal tests and EPT results report no response to the test as positive can also be confusing. Furthermore, the literature reports the results in terms of categories of vital and nonvital or pulp necrosis. The confusion then is that a tooth can test for a disease state that is irreversible pulpitis and still be in the vital category. Thus, in terms of sensitivity, specificity, and predictive value, much of what is reported is in reference to differentiating between no pulp and some pulp present in the tooth.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


