Current concepts and recommended treatment for temporomandibular disorders (TMDs) and temporomandibular joint pain and dysfunction have evolved over time. This article attempts to distill the current information for this often confusing topic into relevant clinical issues that will allow the general dental practitioner to be better able to diagnose and interpret clinical findings, and institute a therapeutic regimen that will provide needed relief to patients suffering from TMD dysfunction. Current management methods, both surgical and nonsurgical, are reviewed and discussed.
Temoporomandibular disorders (TMDs) are defined as clinical problems involving the masticatory musculature, the temoporomandibular joints (TMJs) and associated structures, or both. The abbreviation MPD (myofascial pain dysfunction) has been used to describe those disorders that involve only the muscles of mastication and associated fascia, which are the result of excessive muscle activity causing muscle pain.
TMD is considered the most common musculoskeletal disorder that causes orofacial pain. The cardinal presenting signs of TMD that the patient may present with include the following:
- 1.
Limitation of jaw opening or function
- 2.
Pain with jaw opening or function
- 3.
Joint sounds.
TMDs occur disproportionately in women of childbearing age in a female to male ratio of between 4:1 and 6:1; the prevalence drops off significantly for males and females after age 55 years. One study has estimated that approximately 12% of the adult population in the United States suffers from temoporomandibular symptoms every 6 months.
Current concepts and recommended treatment for TMDs and TMJ pain and dysfunction have evolved over time. This article attempts to distill the current information for this often confusing topic into relevant clinical issues that will allow the general dental practitioner to be better able to diagnose and interpret clinical findings, and institute a therapeutic regimen that will provide needed relief to patients suffering from TMD dysfunction. A review of some basic TMJ anatomy and physiology is needed to better understand the current treatment philosophy and objectives.
Relevant TMJ anatomy
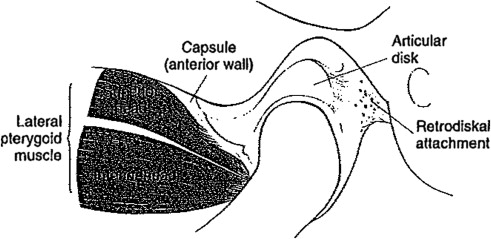
The mandible and cranium make up the craniomandibular articulation, made up of a mandibular condyle below and the temporal bone above. The articular space of the TMJ inside the glenoid fossa is divided into upper and lower quadrants by an avascular fibrous disc ( Fig. 1 ). The disc condyle complex and the mandibular fossa are enclosed within a temoporomandibular ligament. The lateral pterygoid muscle attaches to the disc, and the disc is firmly attached to the medial and lateral poles of the mandibular condyle and moves in tandem with the lower jaw bone.