Introduction
The clinical efficiency of a bonding material relies on its bond strength and debonding characteristics; the depth of resin penetration into enamel affects both of these factors. The depth of resin penetration has been previously studied by researchers using laborious, indirect methods, including the scanning electron microscope and the optical microscope.
Methods
We used a more direct method, confocal microscopy, to visualize the resin tags in enamel. Thirty maxillary first premolars were selected and divided into 3 groups. In group A, the buccal enamel surfaces were conditioned with 37% phosphoric acid; in group B, a self-etching primer was used; and group C was treated with air abrasion. Transbond XT adhesive (3M Unitek, Monrovia, Calif) was used to bond a modified bracket. Transbond XT primer (3M Unitek) mixed with rhodamine B fluorescent dye (Chennai Chemicals, Chennai, India) was applied in groups A and C. In group B, rhodamine was mixed with self-etching primer. After curing, the brackets were debonded, and the teeth were visualized under the fluorescent channel of the confocal microscope.
Results
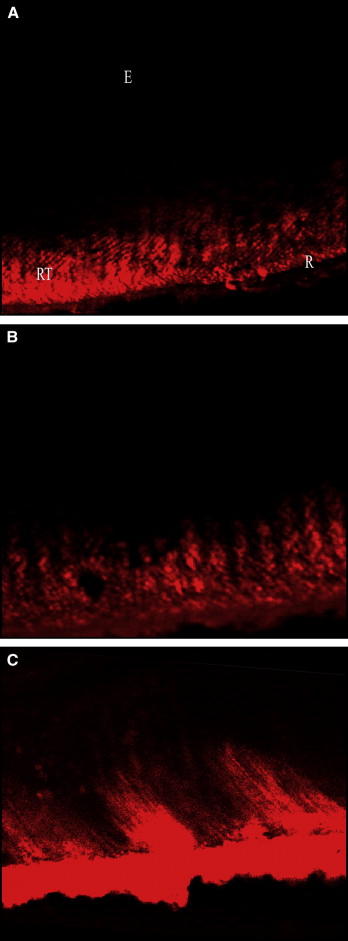
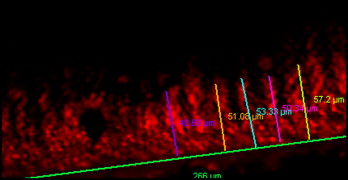
Maximal resin penetration of 53.9 μm was observed in group A, followed by group B at 40.5 μm and group C at 39.9 μm.
Conclusions
Confocal microscope evaluation showed that enamel conditioning with 37% phosphoric acid produced greater depths of resin penetration than did self-etching primer or air abrasion.
An ideal bonding system depends on a number of variables related to bonding materials and clinical technique. This ensures fewer bond failure rates, efficient chair-side time, and minimum damage to enamel during bonding and debonding procedures.
Bond strength and adhesive remnant index scores are, however, parameters of clinical significance influenced by 3 factors: mesh base design, adhesive system, and enamel conditioning methods.
Enamel conditioning methods have a direct influence on the adhesion of adhesive to the tooth structure by creating microporosity and increasing surface energy that promotes adhesion, and by permitting penetration of the resin into enamel as resin tags affording mechanical retention.
The advent of acid etching of enamel by Buonocore in 1955 has made the process a mandatory procedure in restorative and esthetic dentistry and orthodontic bonding. Since then, many studies have been done to standardize the concentration of acid and the duration of application.
The newer self-etching primers, which combine etching and priming into a single step, reduce chair-side time and cause fewer irreversible changes to enamel.
Apart from using acids to condition the enamel, a nonmechanical method with micrometer-sized particles was introduced by Black in 1945.
The depth of resin penetration was first studied by Sheykholeslam and Buonocore. Since then, there have been many studies with an optical microscope, a scanning electron microscope, and photo micrography, but only a few studies have used the confocal laser scanning microscope.
The confocal laser scanning microscope is midway between the optical and electron microscopes. It can produce nondestructive examinations of layers up to 100 μ below the surface and high-resolution images on semitransparent biologic tissues without penetration into the specimen; also a 3-dimensional reconstruction of the specimen is possible. The confocal laser scanning microscope also has the capability of real-time assessment of demineralization and remineralization of enamel and dentin, and can focus into sound enamel. Also, the confocal laser scanning microscope can be used in vivo in dentistry to study the enamel structure, biomaterial interactions, and wound healing.
Although the literature includes many studies of the depth of resin penetration, a direct evaluation (using confocal laser scanning microscope) of the commonly used orthodontic adhesive, Transbond XT, and self-etching primer, Transbond Plus (both, 3M Unitek, Monrovia, Calif), was yet to be conducted. Hence, we intended to study the depth of penetration of Transbond XT adhesive with 3 types of enamel conditioning methods: 37% phosphoric acid, self-etching primer, and air abrasion.
Material and methods
Thirty maxillary first premolars were visually examined to be devoid of caries, enamel cracks, fluorosis, or abrasion. They were extracted for orthodontic reasons, and informed consent was obtained for their use in this study. They were washed in water and stored in 0.1% thymol solution before bonding procedures to prevent dehydration and bacterial growth.
The teeth were divided into 3 groups of 10 each based on the method of enamel conditioning. The teeth in group A received 37% phosphoric acid (Scotchbond etchant, 3M ESPE, St Paul, Minn) and Transbond XT primer. The teeth in group B received the self-etching primer (Transbond Plus), and those in group C had air abrasion (50-μm particle size, Microblaster Standard; Bio-Art, São Carlos, Brazil) and Transbond XT primer.
Before conditioning the enamel, the buccal surfaces were cleaned with a rubber cup and pumice slurry to remove plaque and extrinsic stains. We used Begg brackets (TP Orthodontics, LaPorte, Ind), customized by welding the bracket base to an anterior band material (0.125 × 0.003 in, Rocky Mountain Orthodontics, Denver, Colo) so that the bracket bases had no undercuts ( Fig 1 ). The brackets were bonded on the buccal surfaces according to manufacturer’s instructions.

In group A, the area where the bracket was to be bonded was etched with 37% phosphoric acid for 30 seconds and then rinsed thoroughly with water. The teeth were dried with compressed oil-free air for 5 seconds until a frosted appearance was seen on the enamel surface. Transbond XT primer mixed with rhodamine B dye (Chennai Chemicals, Chennai, India) at a concentration of 0.1 mmol/L was applied as a thin film to the etched enamel surface and cured for 20 seconds. Rhodamine B is an inert dye used to facilitate visualization of the resin tags under the confocal microscope. Transbond XT paste was applied to the bracket base and pressed firmly onto the tooth. The adhesive was cured for 40 seconds by using a light-curing unit (400 mW/cm 2 ; Starlight-P, Mectron s.p.a., Carasco [GE], Italia).
In group B, self-etching primer mixed with rhodamine B at a concentration of 0.1 mmol/L was applied to the enamel for 3 seconds, and air thinning was done for 5 seconds according to manufacturer’s instructions. The bracket was bonded immediately with Transbond XT adhesive as in group A.
In group C, the teeth were air abraded with aluminum oxide powder with 50-μm particles at 160 psi for 3 seconds at a distance of 6 mm. The teeth were then rinsed with water spray for 30 seconds and dried with compressed oil-free air for 20 seconds. Transbond XT primer mixed with rhodamine B dye at a concentration of 0.1 mmol/L was applied and cured for 20 seconds. The bracket was bonded with Transbond XT adhesive as in group A.
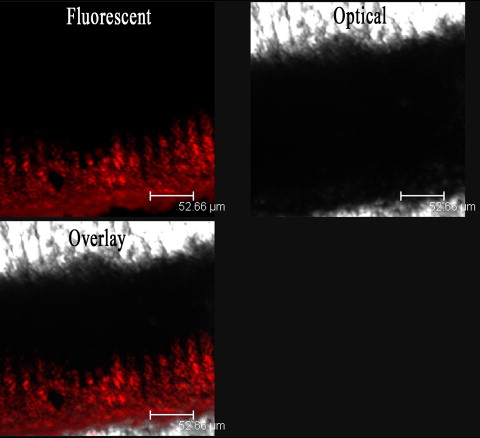
The teeth were then sectioned labiolingually parallel to the long axis of crown by using a hard-tissue microtome (SP 1600; Leica Biosystems Nussloch GmbH, Nussloch, Germany). The microtome was set so that each section was 300 μ thick ( Fig 2 ). The sectioning was done to reduce the amount of time spent in optical sectioning of the tooth with the confocal microscope. The sliced disks were stored dry in amber-colored bottles until microscopic evaluation. The cut surface provided a flat surface for mounting on the microscope.

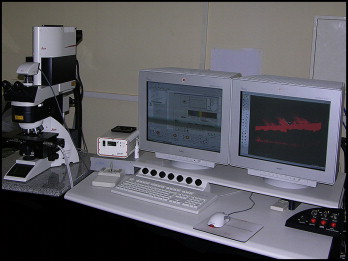
A laser scanning confocal microscope (TSP-2, Leica), which receives illumination from an argon ion laser ( Fig 3 ) was used in this study. The excitation wavelength range for rhodamine B was between 535 and 560 μm. The emission wavelength that was to be collected ranged between 570 and 640 μm.
Since the area of interest in this study was closer to the facial axis of the clinical crown of the tooth, only the hard-tissue disks sectioned close to this, with an intact resin layer, were used for observation.
The sliced disks were viewed by using a 63-times oil immersion lens, and optical sectioning was done uniformly for the 200-μm depth, sparing the superficial 50 μm, which could be scratched from the hard-tissue microtome. The optical sectioning was done with a slice thickness of 1 μ.
From the optical slicing, 5 resin tags in each tooth (which were distinct and continuous from the surface of the enamel extending into the tooth and showed the deepest penetration depth in the same frame) were taken into account and measured. The images obtained ( Figs 4 and 5 ) were processed by using confocal software (2004, Leica) to capture a snapshot of the image and to render the series of images into a 3-dimensional animation. Quantification was done by an examiner (R.K.) using the quantification tool of the confocal software ( Fig 6 ) and repeated for all disks.
Statistical analysis
Descriptive statistics included means, standard deviations, standard errors, and maximum and minimum values of depth of penetration for all 3 groups ( Table I ). Nonparametric analysis was done ( Table II ) to determine significance. When a statistically significant difference was noted, the Mann-Whitney U test was done ( Table III ) to identify which groups were different at P <0.05. Coefficient of variation was done ( Table IV ) to determine the consistency of the results in the groups.
| Group | n | Mean (μm) | SD | SE | Maximum (μm) | Minimum (μm) |
|---|---|---|---|---|---|---|
| A | 10 | 53.9754 | 6.85734 | 2.16848 | 64.082 | 44.576 |
| B | 10 | 40.5510 | 3.8515 | 1.21796 | 48.954 | 35.106 |
| C | 10 | 39.91860 | 7.14243 | 2.25864 | 48.624 | 25.200 |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


