A 6-year-old boy, diagnosed with Crouzon syndrome, had moderate exorbitism, a concave profile, an anterior crossbite of −4.0 mm, and a skeletal Class III jaw-base relationship caused by midfacial hypoplasia. At age 8 years 9 months, a LeFort III osteotomy was performed, and distraction osteogenesis was immediately started with the rigid external distractor system. The midface was advanced approximately 10.0 mm for 6 days, including overcorrection. After the distraction, a reverse headgear was used for 6 years to prevent relapse and to accelerate expected growth. At age 16 years 5 months, after extraction of the maxillary first premolars and mandibular third molars, 0.022-in preadjusted edgewise brackets were placed to treat the edge-to-edge incisor relationship and minor crowding. After 13 months of treatment, the facial profile was significantly improved, and an acceptable occlusion was achieved. During the 9-year observation period after the distraction, acceptable facial growth occurred, and no relapse of the maxillary advancement was observed. However, syndrome-specific growth and methodologically induced relapse should be considered when planning a LeFort III distraction in children for the treatment of Crouzon syndrome.
Crouzon syndrome is an autosomal dominant condition characterized by craniosynostosis with associated dentofacial anomalies. Especially, exorbitism and midfacial hypoplasia are known as pathognomonic symptoms. Patients with Crouzon syndrome often require orthodontic or orthopedic treatment, because of their esthetic and functional problems, such as a Class III malocclusion and midfacial hypoplasia. For several decades, severe cases of Crouzon syndrome were treated mainly by maxillofacial advancement with LeFort III osteotomy, and this surgical procedure provides good treatment results with long-term stability.
Recently, distraction osteogenesis has evolved as a new mainstream surgical technique for patients with jaw deformities since the first application of mandibular lengthening was reported in 1992. Distraction osteogenesis for maxillary advancement started in 1993 and is now widely used in patients with skeletal Class III malocclusion caused by maxillary hypoplasia. Two types of distraction devices have been used for maxillary advancement: internal and external. The rigid external distraction system, first reported in 1997 by Polley and Figueroa, consists of the external distraction devices that have been used for a decade. This approach allows management of patients from childhood to adulthood, with excellent and predictable functional and esthetic outcomes.
For the treatment of craniosynostosis, distraction osteogenesis is currently popular; several reports show the acceptable consequences of midfacial advancement. A 1-year follow-up cephalometric study showed adequate stability of midfacial advancement with distraction osteogenesis in craniofacial dysostosis. Fearon also reported that the maxilla remained stable after LeFort III halo distraction without relapse for up to 5 years postoperatively. However, there are few reports of long-term detailed observation after LeFort III distraction in patients with Crouzon syndrome, and the prognosis of LeFort III distraction performed in childhood is still unclear.
This article demonstrates good prognosis for LeFort III distraction with the rigid external distractor system performed in the mixed dentition in a patient with Crouzon syndrome.
Diagnosis and etiology
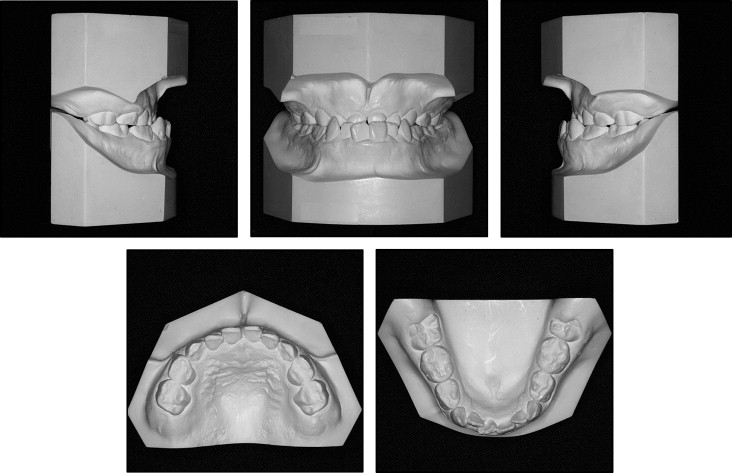
A boy, aged 6 years 8 months, had a chief complaint of anterior crossbite. He was diagnosed with Crouzon syndrome at Tokushima University Hospital in Japan, and his mother also has the same syndrome. He was suspected of having obstructive sleep apnea syndrome, since he had chronic nasal obstruction and significant snoring during sleep. Moderate exorbitism and a concave profile from midfacial hypoplasia were noted ( Fig 1 ). An anterior crossbite of −4.0 mm was observed, and the terminal plane occlusion was a mesial-step type on both sides ( Fig 2 ).
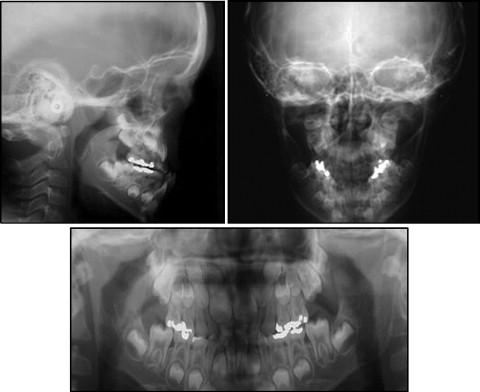
The cephalometric analysis, when compared with the Japanese norm, showed a skeletal Class III jaw-base relationship (ANB, −4.2°) because of a severe maxillary deficiency (SNA, 71.8°). The body length and the ramus height of the mandible were almost in the normal range, but the facial convexity was significantly increased ( Fig 3 , Table ).
| Variables | After DO | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mean, Japanese male ∗ | Pretreatment | Before DO | 1 week | 3 years | 6 years | 9 years † | ||||
| 8 y | SD | Adult | SD | 6 y 9 mo | 8 y 3 mo | 8 y 9 mo | 11 y 5 mo | 14 y 5 mo | 17 y 6 mo | |
| Angle (°) | ||||||||||
| ANB | 4.9 | 1.9 | 3.2 | 2.4 | −4.2 | −4.0 | 3.1 | 2.9 | 2.7 | 3.1 |
| SNA | 81.8 | 3.7 | 81.5 | 3.3 | 71.8 | 71.9 | 76.5 | 77.1 | 76.8 | 76.8 |
| SNB | 76.9 | 3.4 | 78.2 | 4.0 | 76.0 | 75.9 | 73.4 | 74.2 | 74.1 | 73.7 |
| MP-SN | 37.6 | 4.2 | 34.5 | 6.1 | 33.4 | 31.8 | 32.9 | 31.5 | 34.9 | 37.0 |
| Gonial angle | 126.9 | 5.2 | 120.9 | 6.5 | 129.7 | 129.4 | 129.2 | 129.8 | 127.4 | 123.5 |
| U1-SN | 100.8 | 5.0 | 106.0 | 7.5 | 99.4 | 104.5 | 111.3 | 105.5 | 107.2 | 108.5 |
| L1-MP | 91.9 | 7.3 | 95.2 | 6.2 | 85.5 | 76.0 | 85.9 | 88.6 | 92.0 | 86.2 |
| Convexity | 168.3 | 4.2 | 173.2 | 5.5 | 200.3 | 203.7 | 184.0 | 182.0 | 185.7 | 182.7 |
| Interincisal angle | 129.4 | 9.7 | 124.2 | 8.6 | 141.7 | 147.7 | 130.0 | 134.5 | 125.9 | 128.3 |
| Occlusal plane | 20.5 | 3.0 | 15.5 | 4.2 | 11.7 | 12.9 | 12.4 | 11.6 | 10.2 | 12.1 |
| Linear (mm) | ||||||||||
| Point A to VRP | – | – | 45.5 | 46.8 | 55.8 | 59.0 | 59.3 | 57.6 | ||
| Pog to VRP | – | – | 44.0 | 45.3 | 42.3 | 44.6 | 45.7 | 42.5 | ||
| S-N | 65.2 | 2.5 | 72.2 | 3.3 | 65.1 | 68.8 | 70.8 | 73.5 | 75.6 | 75.7 |
| N-Me | 111.4 | 4.0 | 135.7 | 4.0 | 107.1 | 112.3 | 114.4 | 119.6 | 129.8 | 140.9 |
| N/palatal plane | 48.9 | 1.8 | 60.0 | 1.8 | 43.3 | 45.9 | 48.9 | 50.0 | 53.5 | 60.4 |
| Me/palatal plane | 60.2 | 3.1 | 74.6 | 3.0 | 63.8 | 66.4 | 65.5 | 69.6 | 76.3 | 80.5 |
| Ar-Go | 40.4 | 2.2 | 53.2 | 5.7 | 43.3 | 45.1 | 44.7 | 46.5 | 48.6 | 53.3 |
| Ar-Me | 93.0 | 2.9 | 115.6 | 6.8 | 93.4 | 97.3 | 98.3 | 102.7 | 107.9 | 111.6 |
| Go-Me | 61.6 | 2.7 | 76.6 | 4.4 | 58.3 | 60.5 | 62.3 | 65.5 | 69.6 | 70.5 |
| Overjet | 2.8 | 1.4 | 3.3 | 1.0 | −4.0 | −3.5 | 5.9 | 3.0 | 0.5 | 2.1 |
| Overbite | 3.2 | 2.5 | 3.3 | 1.7 | 2.5 | 5.7 | 2.5 | 3.0 | 0.5 | 1.7 |
Treatment objectives
The patient was diagnosed as having a Class III malocclusion, with a skeletal Class III jaw-base relationship caused by midfacial hypoplasia. The treatment objectives were to (1) correct the midfacial hypoplasia and the concave facial appearance, (2) correct the anterior crossbite and establish ideal overjet and overbite, (3) achieve an acceptable occlusion with a good functional Class I occlusion, and (4) improve the tendency for sleep apnea with chronic nasal obstruction and significant snoring. Since the cause of the anterior crossbite, the prognathic profile, and the tendency of sleep apnea was suggested to have been the midfacial deficiency, we planned to advance the midface with distraction osteogenesis and LeFort III osteotomy after complete eruption of the maxillary incisors and first molars.
Treatment objectives
The patient was diagnosed as having a Class III malocclusion, with a skeletal Class III jaw-base relationship caused by midfacial hypoplasia. The treatment objectives were to (1) correct the midfacial hypoplasia and the concave facial appearance, (2) correct the anterior crossbite and establish ideal overjet and overbite, (3) achieve an acceptable occlusion with a good functional Class I occlusion, and (4) improve the tendency for sleep apnea with chronic nasal obstruction and significant snoring. Since the cause of the anterior crossbite, the prognathic profile, and the tendency of sleep apnea was suggested to have been the midfacial deficiency, we planned to advance the midface with distraction osteogenesis and LeFort III osteotomy after complete eruption of the maxillary incisors and first molars.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


