Fig. 16.1
(a) A female patient with intravenous bisphosphonate (zoledronate) with minimum area of exposed bone (arrow) after sore spots of her denture (b). She complained about sore spots 2 months ago. The blood spot was provoked by probing with a blunt probe

Fig. 16.2
Purulent fistula of the left upper jaw of a patient with breast cancer and denosumab therapy. Non restorable teeth were extracted before denosumab therapy. The patient complained about a non-fitting prosthesis. The patient was free of complaints and the fistula was discovered at a recall appointment

Fig. 16.3
Small ONJ lesion caused by a pressure sore (arrow) at typical site in the lower jaw. This patient with metastatic prostate cancer received zoledronate intravenously. The exposed bone is located at the lingual boarder of the removable prosthesis
Generally spoken, ill-fitting dentures and sore spots are the second most mentioned reasons for MRONJ by opening a pathway for the oral flora to the bone [11] because of the injury of the oral mucosa [12]. Additionally, they contribute to MRONJ through the observed inhibitory or toxic effects on keratinocytes that impair the habitual mucous repair mechanisms and later lead to MRONJ [19, 20]. After this tissue breakdown, the damaged mucosa and the underlying bone are in danger to be infected by the local oral flora [21]. MRONJ could manifest thereafter.
The typical location of the mucosal lesions is similar to sore spots caused by any denture base in any patient. Therefore, it is found either underneath the denture base in the nonmobile oral mucosa or at the base margin where the mucosa is mobile during functional movement of the oral muscles [22]. A decubital lesion in BP patients is usually round or oval with a diameter of 1–8 mm. A deep red color typifies a moderate case, whereas a grayish or white lesion surrounded by a reddish inflammation is characteristic of more serious cases. Persistent lesions which led to the exposed bone can be very pale without any reddish inflammation around and not easy to spot (Fig. 16.1a). A blunt probe is therefore a useful instrument.
Even simple measurements like forced probing of the periodontal ligament are reported to have a certain risk of MRONJ. Gallego et al. described an MRONJ caused by a rubber dam clasp [10].
-
Surgical extraction of teeth is regarded to be the most frequent trigger event for MRONJ.
-
Sore spots of denture bases are important prosthodontic risk factors for MRONJ.
-
Every injury or damage to the soft tissues (mucosa) close to bone could cause MRONJ.
Prosthetic Techniques and Recommendations
Guidelines for bisphosphonate-related osteonecrosis (BRONJ) define three levels of risk [8]. In this classification, considerations regarding denosumab were added in brackets:
-
Low risk: Oral bisphosphonate medication or intravenous bisphosphonate once a year (or subcutaneous denosumab) for primary osteoporosis
-
Medium risk: Intravenous bisphosphonate (or subcutaneous denosumab) medication twice a year for secondary osteoporosis (therapy-induced osteoporosis)
-
High risk: Intravenous bisphosphonate (or subcutaneous denosumab) medications monthly for oncological reasons
It should be stated that orally administered antiresorptive medication for more than 3–4 years, as well as concomitant chronic long-term steroid therapy or immunosuppressives like methotrexate may rise the risk [23] to a higher (risk) group. For those patients receiving once-a-year intravenous dose of zoledronate, the risk of necrosis could be higher after 3 years of treatment. In assessing these patients, it is important that oral bisphosphonates before intravenous BP or denosumab therapy should be taken into account estimating the risk [23].
Metastatic cancer patients and patients with multiple myeloma usually receive antiresorptive medications for a long time. These patients could be staged as “high-risk” patients at the beginning of their antiresorptives therapy. This implements that the dental status should be sound and the oral health is in good condition. If decayed teeth have to be removed, generally spoken, if these patients have the need of dentoalveolar surgery, these surgeries should be performed before antiresorptive treatment starts. The start of the antiresorptive therapy should be delayed, if possible, until the dental health is optimized, especially, non-restorable teeth and those with poor prognosis are extracted. Antiresorptive therapy can be started after a stable wound situation is reached. In general, a 10–14-day delay after surgery should be considered as adequate for wound healing [23]. However, every therapy not compromising the gingiva close to the bone can be performed during antiresorptives therapy.
So far, only a few references in literature with a low impact of evidence are available regarding evidence-based treatment guidelines/recommendations for bisphosphonate or denosumab patients.
The following guidelines are suggested by the available literature and the personal experience of the authors (including personal communications) and therefore must be critically reviewed. Principally, these guidelines are referred to patients with a high MRONJ risk:
-
“Long-term successfully worn” dentures with no history of sore spots should not be changed, if possible.Although relining or renewal of existing dentures are thought to improve occlusion, stability, retention, and facial support [24, 25], replacement should be evaluated critically especially when dealing with elderly patients who have worn their removable dentures successfully over a long time. Normally with new dentures, patients perceive an enhanced oral health-related quality of life [25], but new dentures require that patients adapt to its new function and they are also known to have problems with sore spots after prosthesis delivery: Kivovics et al. observed denture-induced mucosal injuries in 87 % in the first, 50 % in the second, and 7 % in the third week after placement of complete dentures [22]. Therefore, there might be an elevated risk for MRONJ development.
-
If new dentures or prosthesis with gingival support have to be inserted, a soft lining could be considered.Most authors recommend a soft lining technique to reduce sore spots (Fig. 16.4a, d). They also line the surface of dentures to dissipate and distribute forces by their cushioning effect [24, 26]. Soft lining materials are principally applied temporarily to the underling denture base to distribute the pressure uniformly on the supporting tissues under the denture. The viscoelastic properties of these materials are important for their cushioning effect, which allows a more homogeny pressure distribution, and maintaining the shape of the materials [27–29].
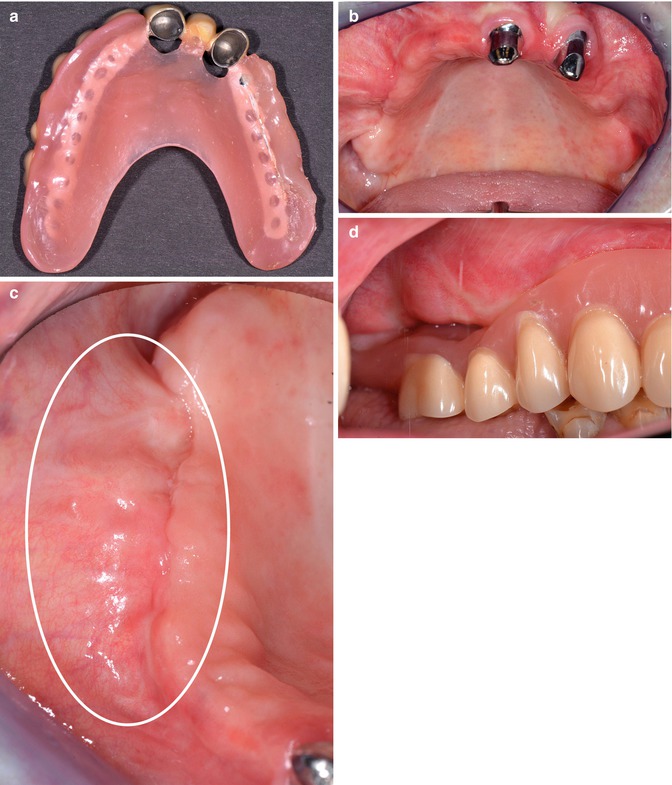 Fig. 16.4(a) New overdenture of a female patient with multiple myeloma and successful MRONJ treatment (surgical resection). Shortly after therapy, zoledronate was restarted combined with lenalidomide (chemotherapy). The intra-oral situation (b) shows a prominent buccal flap covering the defect at the right alveolar jaw. No sign of fistula or exposed bone. Detail (c) of this region (photo taken with mirror). The area (c) with vulnerable, thin, and non-fixed gingival is marked. This area is very sensitive to sore spots and therefore at risk for a relapse of MRONJ. Special attention was drawn to this area with the prostheses (d). A soft lining material covers the vulnerable area. The gap is resulting from retraction of the buccal tissue flap. To reduce the pressure forces, only the first molar was lined upSoft lining materials are very sensitive to contamination with candida or other microorganisms. Soft linings should be controlled regularly and renewed if contamination with candida or other microorganism is obvious [26, 30, 31]. Soft liners should remain for 3 years maximum but usually have to be exchanged earlier [30]. A minimum thickness of 1.5–2 mm is necessary to distribute the pressure to the supporting tissues underneath the denture base [28]; some authors even claim 3 mm [27, 29].On the other hand, some authors observed additional irritations of the mucosa with soft liners leading to ulcers [32].
Fig. 16.4(a) New overdenture of a female patient with multiple myeloma and successful MRONJ treatment (surgical resection). Shortly after therapy, zoledronate was restarted combined with lenalidomide (chemotherapy). The intra-oral situation (b) shows a prominent buccal flap covering the defect at the right alveolar jaw. No sign of fistula or exposed bone. Detail (c) of this region (photo taken with mirror). The area (c) with vulnerable, thin, and non-fixed gingival is marked. This area is very sensitive to sore spots and therefore at risk for a relapse of MRONJ. Special attention was drawn to this area with the prostheses (d). A soft lining material covers the vulnerable area. The gap is resulting from retraction of the buccal tissue flap. To reduce the pressure forces, only the first molar was lined upSoft lining materials are very sensitive to contamination with candida or other microorganisms. Soft linings should be controlled regularly and renewed if contamination with candida or other microorganism is obvious [26, 30, 31]. Soft liners should remain for 3 years maximum but usually have to be exchanged earlier [30]. A minimum thickness of 1.5–2 mm is necessary to distribute the pressure to the supporting tissues underneath the denture base [28]; some authors even claim 3 mm [27, 29].On the other hand, some authors observed additional irritations of the mucosa with soft liners leading to ulcers [32]. -
For less stress transference to the bone and reduction of undesirable horizontal forces, acrylic cuspless/monoplane teeth were recommended in dentures [24].
-
Preprosthetic surgery should be performed, if possible, before any antiresorptive treatment, in order to remove any bony spikes and spicules, which act as foci of stress concentration during denture function [24].
-
If crowns (regardless whether they support fixed or removable partial dentures) are insufficient, rescue fillings should be considered, if the prostheses are functional.
-
Fixed partial dentures seem to be associated with a lower MRONJ risk when compared to removable partial ones with mucosal support.
-
Mucosal support should be avoided in critical areas of vulnerable tissues or areas of healed MRONJ or lately extraction sites (Fig. 16.4c).
-
High water design of bridge pontics enables the possibility to control the mucosa underneath, especially if a tooth was extracted under BP medication in this area previously. The bridge could also be inserted temporarily to control this area before using a permanent luting agent. An esthetic loss should be considered.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


