Introduction
Light curing has become increasingly popular for orthodontic bonding, partly as a result of improvements in light-curing unit technology and higher light intensities. The aim of this study was to determine orthodontists’ knowledge of dental light-curing units, their safety aspects, and the possible effects on color perception.
Methods
Questionnaires were administered to 120 specialists or trainees to assess their knowledge of light curing and safety issues. In addition, 15 orthodontists and 15 nonorthodontists were asked to complete the Farnsworth Munsell 100 hue test to assess color perception.
Results
One hundred four questionnaires were returned, giving a response rate of 86.6%. Light-emitting diode lights were the most popular (73.4%), followed by quartz-halogen (9.2%) and plasma lights (5.5%); 11.9% were unsure of the type of light used, 84% did not know the intensity, and 67% did not know the wavelength of the lights. Although most used safety equipment—eg, paddles—7% used no safety measures. Seventy-six percent were either unsure or took no precautions during light curing for staff or patients who had previous cataract surgery, and up to 99% were either unsure or took no precautions during light curing for staff or patients taking photosensitizing medications. With the Farnsworth Munsell test, 28 participants had average color discrimination, with 2 demonstrating superior discrimination. There were no differences between the orthodontists and the controls, or between men and women.
Conclusions
Orthodontists’ knowledge of dental light-curing units and hazards is poor. Although potential risks are associated with the long-term use of these light-curing units, no effect on color discrimination was detected.
With modern high-intensity dental light-curing units, there is the potential for optical radiation injury to both the eyes and the skin. Whereas thermal injuries require an intense exposure over a short time to have an effect, photochemical injuries depend on dose rate and exposure duration. This means that photochemical injury to the retina can result from viewing either a high-intensity light for a short time or a lower-intensity light for a longer time. To guard against such injuries, there are natural built-in protective mechanisms such as the aversion response to bright light, squinting, and skin tanning. In dentistry, additional protective measures can be used, including protective orange spectacles or paddles.
The precise wavelength of what can be considered visible light varies among persons but, on average, is within the range of 400 to 700 nm. Light entering the eye passes through the conjunctiva, the anterior chamber, the lens, the posterior chamber, and finally focuses on the retina. At each stage, some filtering occurs, and, with age, the degree of spectral transmission changes.
As a result of the focusing effect of the lens, light that might otherwise have insufficient intensity to produce skin damage could be sufficient to cause injury to the eye. This will be affected by factors such as the direction of the gaze, the diameter of the pupil, whether the pupil is obscured by the eyelids, and also whether the subject has responded with an aversion reflex.
In dentistry, blue light is used to cure dental materials; it is also essential for retinal physiology and control of the circadian rhythm. Despite this, blue light is also the most hazardous component of the visible spectrum because it is a high-energy, short-wavelength radiation that can lead to the production of free radicals that react freely with lipids, proteins, carbohydrates, and nucleic acids. This can not only lead to cell damage but also create further free radicals.
In normal vision, light absorption by visual pigments leads to splitting or conversion of the pigment and bleaching of the photoreceptor cells of the retina. In the case of blue light, this process is thought to be mediated by rhodopsin, the visual pigment found in the rods. Phototransduction (the process by which light is converted into electrical signals) is triggered by the conversion of 11-cis retinal to the intermediate all-trans retinal in rhodopsin. On a cellular level, blue-light rhodopsin activation can induce oxidant injury in both the inner and outer segments of the rods. The degree of damage is proportional to the amount of light absorbed. When the photoreceptor cell is bleached, it is unavailable for light absorption until the visual pigment is reformed through a metabolic process called the visual cycle. However, blue light can bypass the visual cycle and restore rhodopsin from its bleached state through a process termed photoreversal. This enables rhodopsin molecules to absorb even more blue light, greatly increasing the potential for retinal damage. The retinal pigment epithelium protein 65 is an important determinant for rhodopsin regeneration, because it has been found that blue light has no effect on retinas when rhodopsin regeneration is inhibited by the depletion of retinal pigment epithelium protein 65 in mice.
Other retinal molecules are also thought to be implicated in mediating the phototoxicity of blue light: eg, cytochrome oxidase, a key enzyme in the respiration. Although there are antioxidative mechanisms present, by middle age, many of these are less effective, increasing the susceptibility of the retina to blue-light damage, deterioration, and the possible development of age-related macular degeneration. Retinal pigment epithelium cells are also lost with increasing age, particularly in the macular center, and the workload of these lost cells must then be assumed by neighboring retinal pigment epithelium cells to compensate for functional loss. Melanosomes in the retinal pigment epithelium play an important role in the scavenging of free radicals and the absorption of stray light in the eye. With age, the density of the melanosomes also decreases, reducing their photoprotective role. Blue light can also lead to melanosome damage.
Retinal cones contain 3 light-sensitive pigments that are maximally sensitive to either short (blue), medium (green), or long (red) wavelengths. Colors are detected when the 3 photo pigments are stimulated to differing degrees; white and gray are recognized when all 3 photo pigments are stimulated equally. Deficiencies in color perception can be congenital or acquired, and the latter can be due to ocular pathology, intracranial injury, or prolonged use of therapeutic drugs. It has been shown that repeated exposure to blue argon light can slowly cause small losses of color contrast sensitivity in ophthalmologists, with a correlation between the number of years of laser experience and a chronic reduction in tritan color-contrast sensitivity. It is currently unknown whether the same color deficiency might occur in orthodontists after repeated and prolonged use of high-intensity dental curing lights in everyday practice.
The aims of this study were therefore 2-fold: to determine the current knowledge of orthodontists with respect to their curing lights and safety implications, and to test the color perception of a group of orthodontists who frequently use high-intensity curing lights and compare the results with the color perception of a group of nonorthodontists.
Material and methods
This study was divided into 2 parts. The first part was a self-administered questionnaire to determine the knowledge of a group of orthodontists about their curing lights and, in particular, the safety aspects. The second part was a color discrimination test with the Farnsworth Munsell 100 hue test.
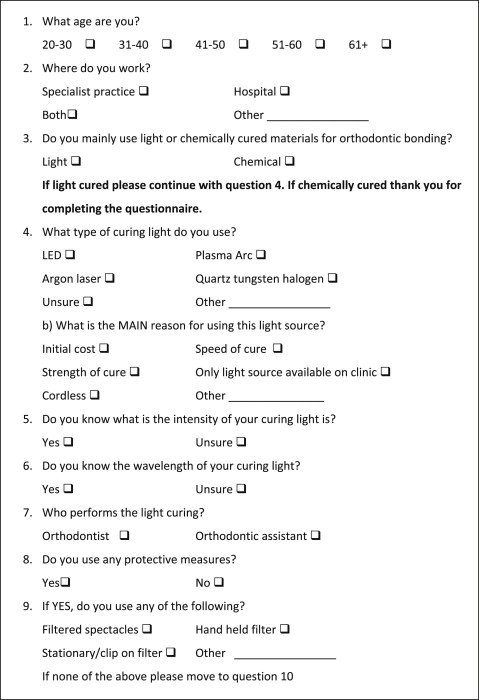
The self-administered questionnaire was designed to assess the profiles of the orthodontists, the procedures used for light curing, their knowledge of visible light-curing units, and safety aspects.
An initial pilot study was carried out with 3 orthodontists (2 consultants, 1 registrar); after feedback, modifications were made to produce the final questionnaire ( Fig 1 ). The National Research Ethics Service leaflet, Defining research , categorized this part of the study as a service evaluation that did not require ethical committee approval. A total of 120 questionnaires were distributed at 3 orthodontic meetings to specialist registrars and specialist orthodontists in 2009 and 2010. They were collected at the end of each meeting; 104 responses were obtained from a total of 120 questionnaires distributed, for a response rate of 86.6%.
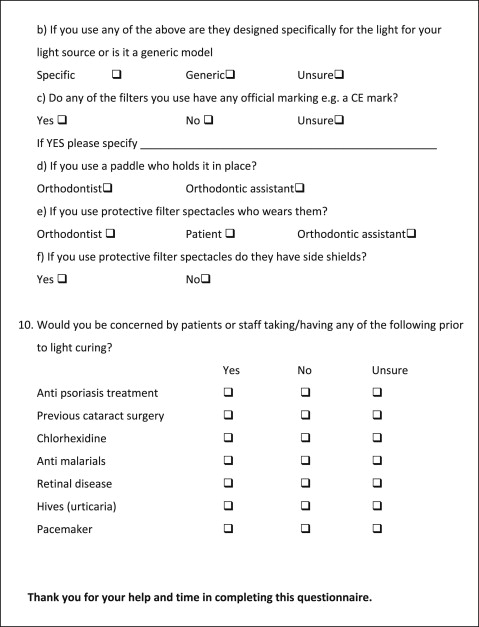
The color perception test in this pilot study involved the use of the Farnsworth Munsell 100 hue test. This is a simple method of testing color discrimination comprising 4 boxes with a total of 93 colored caps ( Fig 2 ). Each box relates to 1 part of the color spectrum. There are 2 fixed caps in each box representing the range of the respective spectrum. The remaining caps are removable and randomly arranged, and participants are asked to rearrange the caps into the correct order in the box so that the colors are graded (ordered) between the 2 fixed colored caps. This part of the study received ethical committee approval from the South West 4 REC, Bristol, United Kingdom (10/H0102/65).

An e-mail was sent to the staff of the Bristol Dental Hospital requesting volunteers. An information leaflet was attached to each e-mail explaining the aims of the project, and providing information on the Farnsworth Munsell 100 hue test and details of the inclusion and exclusion criteria. The principal exclusion criteria were previous or current eye diseases or operations, color blindness, and diabetes. Diabetes is a risk factor for macular degeneration and could contribute to changes in color discrimination. Eye diseases or operations could also lead to similar problems and affect the results.
In total, 15 orthodontists and 15 nonorthodontists were recruited for this pilot study. Each participant was given a unique identification number and a questionnaire that asked age, how long (years), and how frequently (hours per week) that they estimated their use of dental curing lights.
The primary outcome measure for this test was the total error score, which helps to determine the level of color discrimination. In the reference population for the test, 16% of the subjects had superior ability (<17 errors), 68% had average ability (20-100 errors), and 16% had low ability (>100 errors).
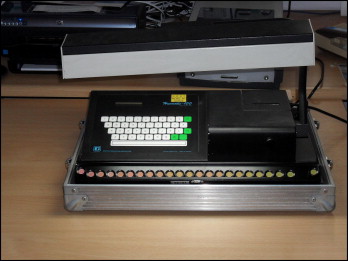
Each participant was instructed in the use of the Farnsworth Munsell 100 hue test and then asked to complete it once. It was decided not to do retests; the manual accompanying the test equipment states that there is an average reduction of 30% in total error score between the first test and a retest. It also states that if the first test demonstrates that a participant has no gross color deficiency, there is little point in retesting. The test took place in a room at the Bristol Dental Hospital with a standardized light box designed for the Farnsworth Munsell 100 hue test to ensure that the background lighting was the same for each participant ( Fig 3 ). The ambient light in the room was minimized by closing the blinds and turning off the indoor fluorescent lighting. This was the same for each test.
The scores from the tests were entered into analysis software (Farnsworth Munsell 100 software; Haag-Streit, Harlow, Essex, United Kingdom) to determine whether there were any significant differences between the 2 groups.
Results
Of 120 questionnaires distributed, 104 were returned, for a response rate of 86.6%. Of the respondents, 31 (29.8%) were 21 to 30 years old, 47 (45.2%) were 31 to 40 years, 20 (19.2%) were 41 to 50 years, and 6 (5.8%) were 51 to 60 years. Thirty-two (30.8%) worked as specialists in primary care, 60 (57.7%) worked as specialists in secondary care (hospital), and 12 (11.5%) worked in both. One hundred respondents (96.2%) used mainly light-cured materials for orthodontic bonding, with only 4 (3.8%) using mainly chemically cured materials. Of the 100 respondents who used dental curing lights, 9 used more than 1 type of curing light (giving in effect 109 responses). Eighty (73.4%) used light-emitting diode lights, 6 (5.5%) used plasma lights, 10 (9.2%) used quartz-tungsten-halogen lights, and 13 (11.9%) were unsure of the type of light they used. When asked whether they knew the intensity or wavelength of the light produced by their curing lights, 84 (84%) did not know the intensity of the light, and 67 (67%) did not know the wavelength.
When asked who performed the light curing, 70 (70%) of the orthodontists questioned performed the light curing themselves, 18 (18%) had the light curing performed by an orthodontic assistant, and in 12% of cases both the orthodontist and the assistant performed the light curing. Of concern, 7 (7%) of those questioned used no safety procedures during light curing. The remainder did use safety equipment, and some used more than 1 type. Twenty-five (26.9%) used filtered spectacles, 69 (74.2%) used a hand-held filter or paddle, and 37 (39.8%) used a stationary or clip-on filter. Of these, 40 (43.0%) stated that the equipment was generic, 26 (28.0%) said the safety equipment was specifically designed for the lights used, and 27 (29.0%) were unsure whether the equipment was specific or generic. Eighty-six (92.5%) respondents were either unsure (85.0%) or did not know (7.5%) whether the safety equipment had an official marking–eg, a CE mark (Conformité Euroéenne or European Conformity). When asked what type of safety equipment they used, 69 respondents used hand-held filters or paddles, with the orthodontic assistant holding the paddle in 60 (87.0%) cases, whereas only 5 (7.2%) orthodontists held the filter themselves. Four (5.8%) respondents stated that both the orthodontist and the assistant might hold the paddle. In the case of safety glasses, of those who reported they were used during bonding, in 18 (72%) cases, it was the orthodontic patient who wore the glasses, in 12 (48%) cases the orthodontist, and in 5 (20%) cases the orthodontic assistant. In 18 cases (72%), the protective glasses had side shields, but in 7 cases (28%) they did not.
The 100 orthodontists who used curing lights were also asked about their knowledge of known photosensitizing medications. Seventy-six (76%) respondents were either unsure about, or did not take, precautions during light curing for staff or patients who had previous cataract surgery. The number for retinal disease, 73 (73%), was similar. Certain antimalarial drugs, antipsoriasis treatments, and chlorhexidine are also known to be photosensitizing medications. Ninety-nine (99%) respondents were either unsure about, or did not take, precautions for patients taking antimalarial drugs. Similar results were found for chlorhexidine (98%) and antipsoriasis treatments (97%).
Thirty participants were recruited from the Bristol Dental Hospital. Fifteen were orthodontists who routinely used light-curing units, and 15 were a control group of nonclinical staff (receptionists and secretaries), who do not use light-curing units. The participants were asked to complete the Farnsworth Munsell 100 hue test, and each participant was given a unique identification number and a questionnaire, which asked their age, how long (years), and how frequently (hours per week) they used dental curing lights.
Tables I and II give the results for both the orthodontists and the controls. The primary outcome measure for the Farnsworth Munsell 100 test was the total error score. This helps to determine the level of color discrimination. In the reference population for this test, 16% had superior ability (<17 errors), 68% had average ability (20-100 errors), and 16% had low ability (>100 errors). Of the subjects in this study, 100% of the orthodontic group had average color discrimination. Two (13.3%) controls had superior discrimination, and the rest (86.7%) had average discrimination. The mean error scores were 50.67 for the orthodontic group and 48.27 for the controls.
| Orthodontist | Age (y) | Sex | Light use? (y) | Hours per week | Time (min) | Error score | Classification |
|---|---|---|---|---|---|---|---|
| 1 | 20-30 | M | 7 | 0.5 | 8 | 72 | Average |
| 2 | 31-40 | M | 18 | 0.5 | 11 | 44 | Average |
| 3 | 31-40 | M | 15 | 1 | 16 | 32 | Average |
| 4 | 31-40 | F | 10 | 3 | 13 | 68 | Average |
| 5 | 31-40 | F | 8 | 2 | 9 | 32 | Average |
| 6 | 51-60 | F | 20 | 1.5 | 7 | 92 | Average |
| 7 | 20-30 | F | 8 | 2 | 7 | 88 | Average |
| 8 | 31-40 | F | 15 | 3 | 8 | 68 | Average |
| 9 | 31-40 | F | 13 | 1 | 9 | 28 | Average |
| 10 | 41-50 | F | 22 | 1 | 8 | 24 | Average |
| 11 | 20-30 | M | 11 | 0.75 | 14 | 36 | Average |
| 12 | 31-40 | M | 12 | 2 | 13 | 48 | Average |
| 13 | 61+ | M | 15 | 0.25 | 11 | 52 | Average |
| 14 | 31-40 | M | 11 | 1 | 9 | 52 | Average |
| 15 | 31-40 | M | 11 | 1 | 14 | 24 | Average |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


