Introduction
We investigated whether careful interdental enamel reduction (using extrafine diamond disks with air cooling, followed by contouring with triangular diamond burs and polishing) leads to increased caries risk in premolars and first molars.
Methods
Our subjects were 43 consecutive patients from 19 to 71 years of age who had received mesiodistal enamel reduction of anterior and posterior teeth 4 to 6 years previously. Dental caries were assessed on standardized bite-wing radiographs according to a 5-grade scale and with a fine-tip explorer catch. The incidence of interproximal caries was compared between reproximated and unground contralateral surfaces in the same patient. Patients were asked about their toothbrushing habits, use of dental floss and toothpicks, and regular fluoride supplementation after the orthodontic appliances were removed.
Results
The overall clinical impression generally showed healthy dentitions with excellent occlusion. Only 7 (2.5%) new caries lesions (all grade 1) were found among 278 reproximated mesial or distal surfaces, in 3 patients. Among 84 contralateral unground reference tooth surfaces, 2 lesions (2.4%) were seen. On nonpaired premolars and molars that had not been ground, 23 surfaces had to be referred for caries treatment (grade 3 or occlusal caries). Eleven of these occurred in 1 patient. None of the 43 patients reported increased sensitivity to temperature variations.
Conclusions
Interdental enamel reduction with this protocol did not result in increased caries risk in posterior teeth. We found no evidence that proper mesiodistal enamel reduction within recognized limits and in appropriate situations will cause harm to the teeth and supporting structures.
Interproximal enamel reduction (IER; reproximation or simply interdental stripping) offers an attractive alternative to overcome difficulties with premolar extraction cases and the instability of overexpansion in nonextraction cases. It significantly reduces treatment time and allows transverse arch dimensions and anterior inclinations to be maintained. An obvious advantage of stripping is that it will prevent or reduce interdental gingival papilla retraction —ie, the development of black triangles between teeth. Optimal gingival fill in is, of course, particularly important when treating adult orthodontic patients.
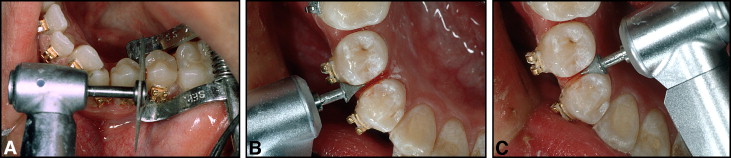
Various methods for IER have been tested over the years and progressively improved. The 3 most common techniques at present are (1) the air-rotor stripping (ARS) technique with fine tungsten-carbide or diamond burs and diamond-coated strips (primarily in the posterior segments), (2) hand-piece or contra-angle-mounted diamond-coated stripping disks ( Fig 1 ), and (3) handheld or motor-driven abrasive strips. It is generally assumed that the finer the grain size used for removing enamel, the easier and less time-consuming the subsequent polishing. If adequate polishing is not performed, scratches and furrows remain in the enamel surface. These promote the adherence of plaque bacteria and potentially increase susceptibility to dental caries. Also, unintentionally produced interproximal steps during stripping can cause future cavities.
It is obvious that fixed orthodontic appliances can create an environment favorable to caries. Whether the caries risk is further enhanced by stripping associated with the orthodontic treatment is still a matter of debate. However, so far, no convincing evidence has demonstrated that the roughness produced by IER is a predisposing factor to caries.
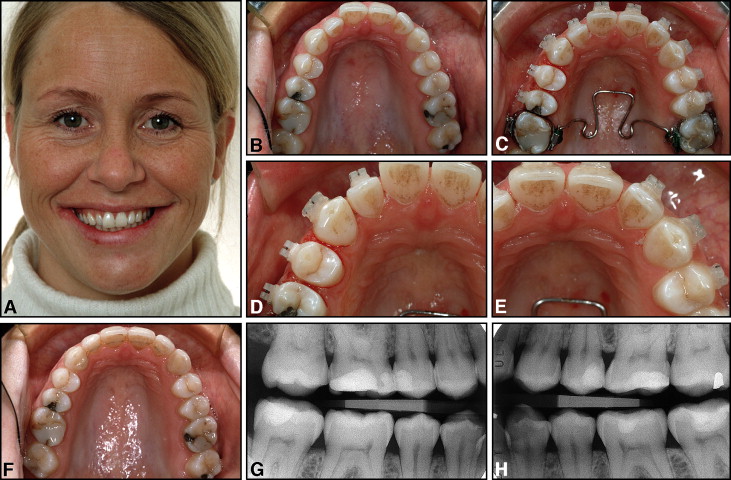
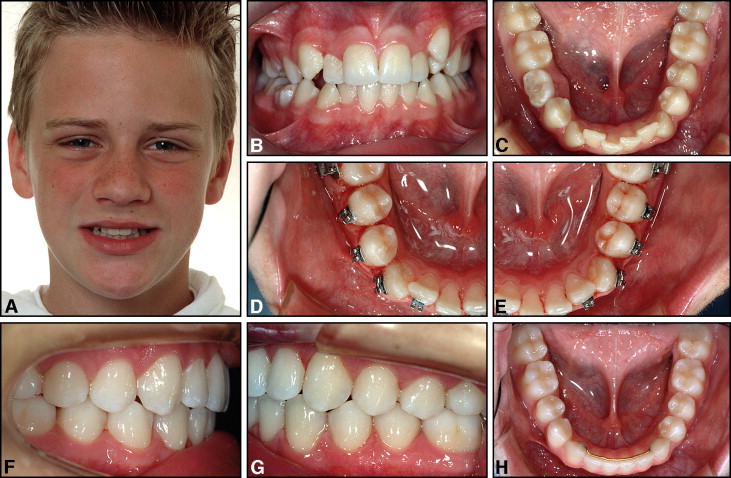
An earlier follow-up study showed that careful IER in the mandibular anterior region (the most common site for IER) produced healthy dentitions with intact periodontal soft-tissue contours in the long term (>10 years after treatment). The reproximated surfaces were no more susceptible to caries and periodontal disease than unaltered surfaces. Although caries development in the mandibular incisor area is relatively rare, extending the stripping procedure posteriorly into areas that are generally more prone to caries might lead to increased caries susceptibility ( Fig 2 ). Both the maxillary and mandibular posterior regions (premolars and first molars) have now become included with increasing frequency in our stripping protocol. Therefore, it appeared prudent to expand our interest in the long-term dental health after stripping to include the premolar and first molar regions. The purpose of our study was therefore to assess the caries risk in the maxillary and mandibular first premolar to first molar areas in a group of adolescent and adult orthodontic patients who had received extensive interdental stripping with a careful technique in the anterior and posterior regions as part of their orthodontic treatment.
Material and methods
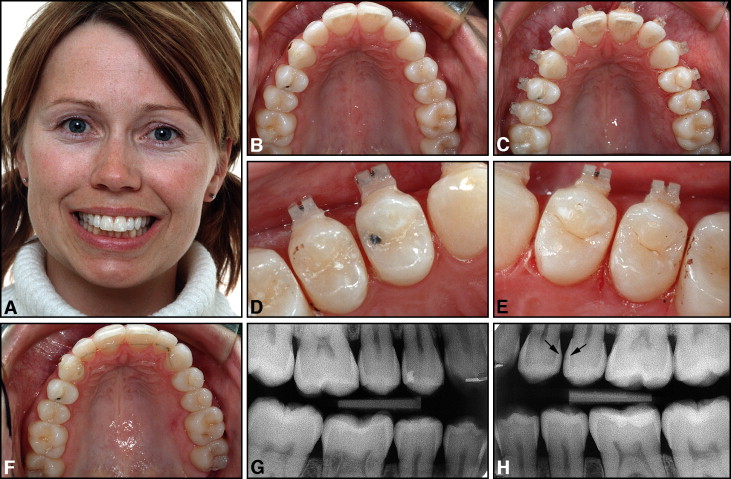
The material for this study was collected from the private practice of the first author (B.U.Z.). The sample included all patients in a consecutive series of 80 who had had stripping of several maxillary and mandibular teeth in the anterior and posterior regions at least 4 years before the clinical examination. These patients were contacted by mail or telephone and invited to participate in a follow-up study. All had been treated by the first author, using maxillary and mandibular fixed edgewise appliances (.018 × .025-in attachment slots). Brackets were bonded to all teeth in both dental arches, except for the maxillary for first molars that were banded ( Figs 3-5 ). According to clinical and radiographic screening, all patients were considered caries-free when their orthodontic appliances were placed. The study was approved by the Regional Committees for Medical and Health Research Ethics, Norwegian Social Science Data Services. Because of difficulties in locating and contacting some patients, only 43 subjects (54%) appeared for the clinical follow-up examination. Thirty-five persons could not be traced, 9 lived in remote parts of Norway or abroad, 2 did not want further examination, and 1 did not attend. The study group included 29 women and 14 men, from 19 to 71 years of age. Six patients were less than 20 years, 23 were between 20 and 50 years, and 14 were older than 50. The time interval between debonding and follow-up was more than 6 years in 9 patients, between 4 and 6 years in 32 patients, and 3.5 to 4 years in 2 patients.
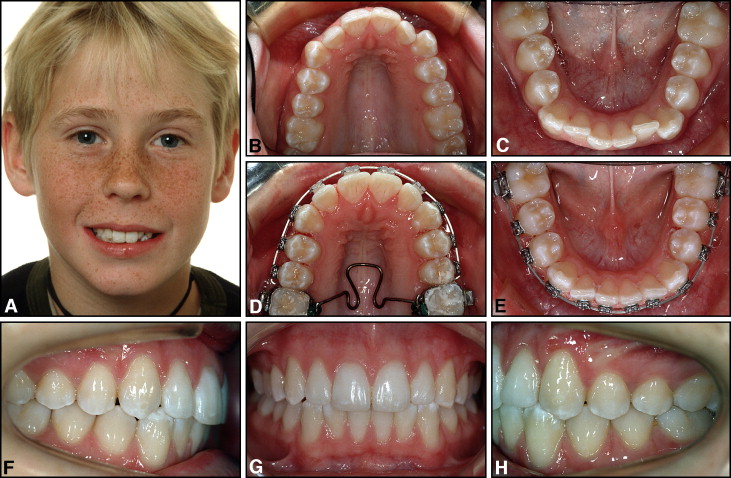
New perforated diamond-coated stripping disks (Komet 8934A.220, Brasseler, Lemgo, Germany) were mounted on a contra-angle hand piece (Kavo, Biberach, Germany), and the enamel reduction was done with a modified Tuverson technique. 14 The stripping disk was double-coated with extrafine diamond grit (8-10 μm) and used at medium speed (about 30,000 rpm) ( Fig 1 ). A 4-handed approach was used. An assistant kept the patient’s tongue away with a mouth mirror and, at the same time, blew a stream of air from a 3-way syringe to cool the teeth to be ground. The interproximal “corners” were rounded off by using friction-grip, cone-shaped triangular diamond burs (Komet 8833, Brasseler) ( Fig 1 , B and C ). Polishing was made with fine Sof-lex disks (3M, St. Paul, Minn). As a general rule, the stripping was performed at the beginning of treatment after an initial leveling phase of the teeth for 1 or 2 months. Access to the interproximal surfaces of crowded teeth was improved by the use of an Elliott anterior straight separator (Benco Dental, Wilkes-Barre, Pa) ( Fig 1 , A ).
The principle of the IER technique was to reshape the premolars, canines, and incisors (and when necessary, also the mesial surfaces of the first molars) with abnormal morphology in both dental arches toward a more ideal anatomy. Care was taken to prevent proclination of the mandibular incisors if they were in front of the A-pogonion plane at the start of treatment and to maintain normal (24-26 mm) intercanine widths and mandibular arch forms ( Figs 3 and 6 ). The original maxillary arch forms were also preserved and not expanded laterally but were generally rounded off during treatment ( Figs 3-5 ). A custom-designed transpalatal arch was used to derotate the maxillary first molars and control the arch forms ( Figs 3, D , and 5, C ). The total amount of enamel removed from each patient depended on how much the mesiodistal tooth shapes deviated from optimal morphology and, of course, on the arch length deficiency in each case. In particular, oval premolars in both arches were reproximated to more round shapes ( Figs 1 and 3-6 ), and triangular incisors were recontoured to obtain more parallel sides ( Figs 3, 5, and 6 ). By recontouring posterior and anterior teeth in both dental arches, the space gained was sufficient to completely correct the crowding in all patients. Topical fluoride agents were not applied to the ground tooth surfaces, but all patients were routinely instructed to use 0.05% neutral sodium fluoride mouth rinses once daily and fluoridated toothpastes. If increased sensitivity developed after the stripping procedure, the patients were instructed to rinse with fluoride twice daily for 1 to 2 weeks.
The retention appliance used in the mandibular anterior region was either a fixed .0215-in 5-stranded gold-coated Penta-One wire (Gold’n Braces, Palm Harbor, Fla) direct-bonded to all 6 anterior teeth in 30 patients (70%) or a .030-in gold-coated (Gold’n Braces) wire bonded to the canines only ( Fig 6 ) in 11 patients. In 2 subjects, the premolar was also included in the retainer. The maxillary retention regimen generally consisted of a .0215-in gold-coated wire bonded to 4 (15 subjects) or 6 (19 subjects) teeth ( Fig 4 ). In 2 subjects, the premolar was also included, and, in 7 subjects, no maxillary bonded retainer was used. All patients also used a removable plate for full-time or nighttime wear.
The clinical and radiographic assessments and measurements were performed by a dentist (L.M.), blinded with regard to which teeth and surfaces had been ground. The examination consisted of 1 session when 2 standardized posterior bite-wing radiographs were taken with the quick-bite technique ( Figs 4 and 5 ). The intraoral caries diagnosis was made with a fine-tip explorer catch, with the operative light as the source of illumination. The patients were questioned about their toothbrushing habits, whether they were using dental floss or toothpicks regularly, and whether they continued to use fluoride mouth rinses after the appliances were removed. Notes were also taken about their use of medications.
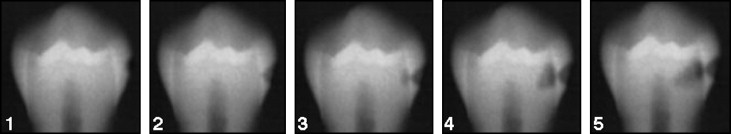
Interproximal caries on each surface was recorded according to a 5-level scale, routinely used in the Department of Pedodontics at the University of Oslo ( Fig 2 ): grade 1, caries in the outer half of the enamel; grade 2, caries in the inner half of the enamel; grade 3, caries in the outer half of the dentin; grade 4, caries in the inner half of the dentin; and grade 5, caries lesions reaching the pulp. The radiographs were examined against a light screen and under a magnifying glass. All teeth were examined, and all carious interproximal surfaces were recorded. Patients with carious attacks graded 3 to 5 were referred for dental treatment.
The incidence of interproximal caries was compared between reproximated and contralateral unground surfaces in the same patient used as the control. The study was limited to contralateral pairs of maxillary and mandibular first and second premolars and the mesial aspects of the first molars in which some teeth on at least 1 side had been reproximated. The remaining unground premolars and molars were also examined for caries. The surface from which enamel was removed will hereafter be called the reproximated surface, and the opposite contralateral unground surface will be called the intact surface. When the contralateral tooth surface had also been reproximated, no further reference surface was used, and both ground surfaces in those patients were assessed as reproximated surfaces.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


