http://evolve.elsevier.com/Hatrick/materials.
Ceramics were introduced into dentistry over a hundred years ago with the advent of porcelain jacket crowns and inlays (1886, developed by Charles H. Land). These are very esthetic materials but are prone to fracture because they are brittle and weak when used in high-function areas of the mouth. For the first half of the twentieth century, amalgam and gold were the primary restorative materials for posterior teeth. Some anterior teeth also had metal in the form of gold margins of three-quarter crowns, class III gold foils, or class V inlays or amalgams that were visible when the patient smiled. In the latter half of the twentieth century, various direct-placement tooth-colored restorative materials such as composite resins and glass ionomer cements were introduced. Within the past three decades all-ceramic materials have been introduced that are much stronger than the original porcelains, and with some improvements in esthetics. As a result, the use of all-ceramic restorations has dramatically increased. At present, ceramic materials are used for a variety of restorations, such as crowns, bridges, inlays, onlays, and veneers. Selection of the type of material to be used depends, in part, on the extent of damage to the tooth, the stresses that will be placed on the restoration, and the esthetic requirements of the patient.
By enhancing the ability to bond restorative materials to metal and tooth structure, advances in esthetic materials and techniques have assisted the dental team in delivering the esthetic results that patients demand. The dental team must keep current with the rapid changes that occur in materials and techniques. Good listening skills are needed to determine the types of esthetic services the patient is requesting, so that the dental team and the patient are working in concert toward the same goal. Esthetic materials must be carefully selected, so that their properties are compatible with the patient’s oral condition and occlusion. Dental hygienists and dental assistants must understand the properties of these materials, so that as important members of the dental team, they can help the dentist to assess the performance of the restorations and alert the dentist when they perceive that a restoration may be failing. They need to be familiar with the physical properties of materials, so that they do not damage the restorations during routine oral hygiene, coronal polishing, and preventive procedures. Dental assistants need to know the handling characteristics of esthetic materials, so that they can either assist the dentist in their placement or perform steps in their placement as permitted by state dental practice acts. In addition, they will be called on to assist in shade taking for the restorations.
This chapter describes the physical and mechanical properties, processing methods including computer-assisted design/computer-assisted machining (CAD/CAM) technology, clinical applications, attributes, and shortcomings of esthetic ceramic materials. The rationale for the selection of ceramic materials for various clinical applications is presented. The principles for adjusting, finishing, polishing, and cementation of ceramic restorations are reviewed. Guidelines for selection of the shade of these materials to obtain satisfactory cosmetic results also are discussed.
Dental Ceramics
The general term ceramics is used to describe porcelain and a variety of materials that are similar in appearance to porcelain but vary in their composition, mode of fabrication, and physical and mechanical properties. Dental ceramics can be classified in a variety of ways based on their composition, processing method, fusing temperature, microstructure, translucency, fracture resistance, and abrasiveness.
Glass and Nonglass Ceramics
To simplify the understanding of dental ceramics they will be classified in this chapter into two broad categories according to their composition: glass (silica)-based and non–glass (crystalline)-based materials. The glass-based ceramics have silica as a main component and have a glassy matrix. They include feldspathic porcelains, leucite-reinforced ceramics, and lithium disilicate ceramics. The non–glass-based ceramics are composed of simple or complex oxides with no glassy matrix. They include alumina and zirconia.
Advantages and Disadvantages of Ceramic Restorations
Esthetic restorations can be made from composite resin, ceramics with a metal substructure (core), or entirely ceramics. The primary advantage of all-ceramic restorations is their esthetics, because there is no metal substructure to hide. Other advantages over direct-placement restorations such as composite resin, glass ionomer cement, or amalgam include their biocompatibility, wear resistance under function, stain resistance, and the ability to precisely place contacts and contours of the restorations. Disadvantages of all-ceramic restorations compared with direct-placement restorations include their brittleness (can lead to fracture), wear of the opposing enamel or restorations, difficulty or inability to repair them in the mouth, the need for two appointments (except for chairside CAD/CAM restorations), and the difficulty of polishing them in the mouth.
Glass-Based Ceramics
Porcelains
Porcelain is a term that has been used in dentistry for many years to describe the class of tooth-colored dental materials that are composed of feldspar, silica or quartz, and kaolin and are glasslike. Ceramic materials that are high in glass content are very esthetic, because their optical properties mimic those of enamel and dentin. However, they are brittle and more prone to fracture than newer low-glass, reinforced glass, or nonglass ceramics.
Feldspathic Porcelain
Until the recent advances in ceramic materials were made, the dental ceramic material most commonly used was feldspathic porcelain manufactured from fine crystalline powders of alumina, feldspar, and silica oxide (or quartz, 44% to 66%) mixed with a flux of sodium or lithium carbonate. As the powder is heated to certain critical temperatures, the porcelain particles fuse together (sinter) to form a type of glass. Examples of feldspathic porcelain include Ceramco 3 (Dentsply), EX-3 (Noritake), Halo (Shofu), and VITA VM13 (Vident/VITA).
Alumina Porcelain
Alumina porcelain was developed in 1965 by J.W. McLean and T.H. Hughes to enhance (about double) the fracture resistance compared with conventional feldspathic porcelain. It is also a glassy type of porcelain that is about half aluminum oxide by weight in a melted glass (silica) matrix. It is fabricated by first dry-pressing it on a refractory die(die capable of withstanding high temperatures), then sintering it at high temperature.
Uses of Porcelain
Porcelain is manufactured in a variety of colors that are produced by the addition of metal oxides to create the different colors (shades) that will match the teeth. The laboratory technician selects powders based on the shade prescription provided by the dentist. These porcelains were initially used for all-porcelain jacket crowns. These jacket crowns were very esthetically pleasing but had a high fracture rate. At present, the feldspathic porcelains are used in conjunction with a cast metal substructure to produce porcelain-fused-to-metal (PFM) crowns or are used to make porcelain veneers. The porcelain becomes more fracture resistant once it is bonded to a substrate (metal in a PFM crown or enamel as with a veneer).
Fusing Temperatures
Porcelains can be classified according to their fusing temperature as high fusing (1294 °C to 1371 °C, or 2360 °F to 2500 °F), medium fusing (1093 °C to 1260 °C, or 2000 °F to 2300 °F), and low fusing (871 °C to 1066 °C, or 1600 °F to 1950 °F). High-fusing porcelain is used most often for the manufacture of denture teeth (see Chapter 17 [Polymers for Prosthetic Dentistry], Figure 17-10).
Reinforced Ceramics
Because the porcelains were prone to fracture, stronger ceramic materials were developed. The most common of these stronger glass-based ceramics are leucite-reinforced ceramics (IPS Empress; Ivoclar Vivadent) and lithium disilicate ceramics (IPS e.max and IPS Empress II; Ivoclar Vivadent). Reinforcing the material with leucite crystals or lithium oxide has more than tripled their fracture resistance.
Lithium Disilicate
Lithium disilicate ceramic is composed of quartz, lithium dioxide, alumina, phosphor oxide, potassium oxide, and small amounts of other components. The resulting glass ceramic has high strength, good marginal integrity, and biocompatibility and, unlike porcelain, can be used in both the anterior and posterior parts of the mouth. It is a very esthetic material because of its high translucency, caused by the low refractive index of the lithium disilicate crystals (the crystals let light pass through rather than dispersing it). Because of its favorable properties lithium disilicate ceramic has become very popular for veneers and esthetic anterior and posterior crowns. It also can be used for short-span fixed bridges as well if not subjected to excessive forces, as with people who grind their teeth (bruxers). It has high flexural strength (300 megapascals [MPa]), and heat-pressing (pressing a molten ingot into a mold) makes it more resistant to crack propagation. It is manufactured in a variety of shades and comes as ingots for the heat-pressed (890 to 920 °C, or 1634 °F to 1688 °F) technique or ceramic blocks for CAD/CAM milling.
Non–Glass-Based Ceramics
Non–glass-based ceramics are crystalline-based with no glass matrix and are composed of oxides of alumina and/or zirconia with minor amounts of other components to improve their properties.
Alumina
Alumina was developed as an alternative to the PFM crown and the first product was In-Ceram (Vident/VITA). Instead of a glass matrix it has a crystalline matrix composed of alumina and an alumina/magnesia or alumina/zirconia mixture called spinel. The alumina matrix is then infiltrated with a glass that flows readily at high temperature. An alternative alumina material is solid sintered alumina (Procera; Nobel Biocare). The resulting ceramic material has very high flexural strength, about three times that of the glass-based materials.
Zirconia
Zirconia (zirconium oxide) ceramics are the strongest ceramic materials currently used in dentistry. They have the highest flexural strength (Table 9-1) and fracture toughness, at least twice as strong as the alumina-based ceramics. Like lithium disilicate they can be heat-pressed or machined. Common brand names include Lava (3M ESPE), Cercon (Dentsply), and VITA YZ (Vident/VITA). Zirconia can be used in the anterior and posterior parts of the mouth for single-unit crowns or as cores for three-unit bridges.
Cementation
Because of their high strength, zirconia crowns can be cemented either with resin cement or conventional cements. Zirconia restorations are not etched or silanated before cementation. They do not respond to acid etchants like the glass-based ceramics, and attempts at etching might produce a powdery residue on the interior of the crown that is difficult to remove. Several manufacturers have developed primers (Metal/Zirconia Primer [Ivoclar Vivadent]; Z-PRIME Plus [BISCO]; Clearfil Ceramic Primer [Kuraray America]) for preparing the interior of the crown for use with resin cements.
Improving the Esthetics of Zirconia
Zirconia is a much more opaque ceramic than lithium disilicate ceramic. To achieve better esthetics, a layer of veneering porcelain can be added to the zirconium core. If the crown fractures, it is usually caused by a fracture of the porcelain veneer or a separation of the porcelain from the zirconia. An alternative to the layering of porcelain is to heat-press a fluorapatite glass-ceramic material onto the zirconia core. A more recent development is a high-translucency zirconia (Lava Plus; 3M ESPE) that can be used as an all-zirconia crown without the need for porcelain layering in many posterior applications.
Physical and Mechanical Properties
Ceramic materials are stiff and brittle, and these properties contributed to the fracture of weak feldspathic porcelains in early clinical applications. Newer ceramic materials are much stronger. Although ceramic materials are generally stronger when compressive forces are applied, it is their flexural strength that is more important for resisting fracture. Glass-based ceramic materials such as the porcelains have relatively low flexural strength. Lithium disilicate has the highest flexural strength of these glassy materials. The non–glass-based (crystalline) ceramic materials have very high flexural strengths. Zirconia has the highest flexural strength of the crystalline materials and also has the highest fracture toughness. See Table 9-1 for a comparison of material strengths.
Thermal Properties
Ceramic materials act as insulators in that they do not conduct heat or cold readily, as do metallic restorations. They will, however, expand or contract when subjected to temperature changes. The degree to which they expand or contract is called the coefficient of thermal expansion (CTE). The higher the CTE the more the ceramic expands or contracts with temperature changes. This change in dimension is not critically important with a restoration made from a single material. However, when two ceramic materials are used jointly in a restoration, as with a porcelain veneer of a zirconia core or porcelain bonded to a metal core (as with a PFM crown), the two materials must have compatible CTEs. Otherwise, the veneering ceramic material may fracture.
Optical Properties
Translucency
Translucent materials allow light to pass through the surface and into the body of the material; some of the light is reflected back out, unlike a transparent material that allows light to pass all the way through it. Glass-based ceramic materials are more translucent than nonglass ceramics and as a result mimic enamel better.
Reflectance
The surface of a ceramic material may reflect light that hits it. How much light is reflected is influenced by the surface polish and the basic structure of the ceramic material. The portion of the light that is not reflected passes into the ceramic and is either absorbed or passed through it.
Opacity
Opaque ceramic materials do not allow light to pass through them. The light is absorbed or reflected. Nonglass (crystalline) ceramic materials are the most opaque. These materials are the least esthetic of the ceramic materials and must be veneered with more translucent, glassy materials to be used for anterior restorations.
Vitality
Glass-based ceramic crowns have a more lifelike appearance (sometimes called vitality) than PFM crowns. They appear vital (similar to natural teeth) because they are fluorescent, that is, they emit light in the visible wave spectrum when ultraviolet light hits them. They are also opalescent because they take on a bluish tinge when light reflects off of them, and an orange-yellow tinge when light passes through them.
Biocompatibility
Ceramic materials are considered to be among the most biocompatible of the restorative dental materials. Clinical studies have not shown an adverse tissue response to these materials. Glass-based ceramic materials will leach some components in minute amounts over time; much less so than alloys or resins. Lithium disilicate shows some initial toxicity in cell cultures that fades with time. Nonglass ceramics have shown no toxicity to date, and zirconia has been successfully used as implant fixtures.
Processing Techniques
A variety of techniques may be used to fabricate all-ceramic restorations, depending on the type of ceramic material that will be used. Ceramic restorations can be made by sintering, slip-casting, heat-pressing, or computer-aided machining.
Sintering
Sintering occurs when ceramic particles are heated to the point that they melt and fuse to adjacent particles at their borders. Methods such as firing the ceramic in a vacuum are needed to reduce porosity and in turn produce a stronger material. To achieve the desired match to the natural tooth, other ceramic materials called stains and glazes are added and fired to join with the previous layer of ceramic. Alumina-based ceramic and feldspathic porcelain that has been reinforced with leucite are the most commonly used materials for the sintering process. Both of these materials have higher flexural and compressive strength compared with traditional feldspathic porcelain. As ceramic processing techniques advance, sintered all-ceramics are being used less, in favor of heat-pressed or computer-aided machined ceramics.
Slip-casting
Slip-casting is a processing technique whereby the ceramic powder is mixed with a water-based liquid to form a mass or slip and pressed onto a porous refractory die that soaks up much of the water. This mass is then fired at high temperature (1150 °C, or 2102 °F ) to create a porous ceramic core. This core is then infiltrated with molten glass by capillary action to make a dense strong core to which conventional porcelains can be added to develop the desired color and degree of translucency or opacity. The slip-casting technique can be used with zirconia-based, spinel-based (magnesium aluminum oxide), or alumina-based ceramic materials. Zirconia-based ceramics have the highest flexural strength of these materials and are several times stronger than the ceramic cores made from aluminum oxide that were introduced in the 1960s. They also have fewer defects from processing.
Heat-Pressing
Heat-pressing uses the lost wax technique, similar to that used to cast gold crowns into an investment mold developed from a wax pattern that was burned out in an oven (the lost wax technique is discussed in Chapter 16 [Gypsum and Wax Products]). Ceramic of the selected shade is pressed into the mold at high temperature (about 1160 °C, or 2120 °F) and pressure (0.4 MPa), making a denser core. Conventional porcelain can be layered on the core to complete the color and contour, or surface stains can be added. A leucite-based ceramic has been used for this process since the 1990s. Commonly known brands are IPS Empress (Ivoclar Vivadent) and Finesse (Dentsply International). An improvement in strength was made with the introduction of a lithium silicate–based ceramic (IPS Empress II and later versions called IPS e.max; Ivoclar Vivadent).
Computer-Aided Machining
Various preprocessed ceramic materials are available in blocks for use with CAD/CAM technology. An optical impression of the prepared tooth is made and either used in the dental office or transmitted to the dental laboratory. A computer software program is used to design the restoration to establish the contours, proximal contacts, occlusal contacts, and margins. A block of the ceramic material in the appropriate shade is selected and placed into a milling machine. A computer, using the design created, instructs the milling device to cut out the restoration. Depending on the material selected, heat processing may be required to complete the firing of the ceramic material. Custom staining and glazing of the restoration may be done to achieve maximal esthetics.
CAD/CAM Technology
Advances in technology over the past three decades have led to the development of sophisticated computer-aided design and computer-aided machining (CAD/CAM) for general industry and for dental applications. Acceptance is growing rapidly for the application of this technology to crown and bridge techniques.
In 1986 the CEREC (Chairside Economical Restoration of Esthetic Ceramic) system was the first to be introduced to dentistry. The manufacturer (Sirona Dental Systems, Long Island City, NY) has continually improved the system (Figure 9-1). At present, there are two chairside CAD/CAM systems commercially available: CEREC and the E4D Dental System (E4D Technologies).
Basic Components of CAD/CAM Systems
CAD/CAM systems have three basic components: (1) an optical scanner, (2) a computer with design software, and (3) a milling device. The optical scanner can make “impressions” (digital images) of tooth preparations and opposing teeth (for details on digital impressions see Chapter 15). The computer software then designs the restoration to fit the preparation, establishes proper contours and contacts, and shapes the restoration to fit the opposing occlusion. The dentist, hygienist, or assistant can modify the design as needed, using the design tools provided. The design is fed into a computer-controlled machine that uses diamond instruments to mill an all-ceramic restoration from a block of ceramic material.
Incorporating CAD/CAM Technology into Private Practice
Benefits of Chairside CAD/CAM Systems
There are a number of benefits that dental practices can derive from using the chairside CAD/CAM systems:
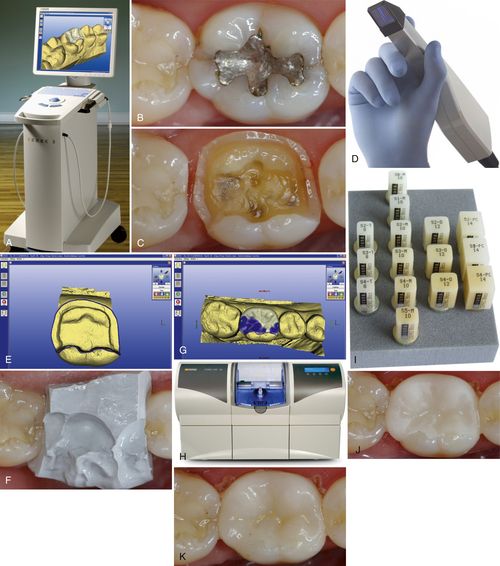
FIGURE 9-1 CAD/CAM in-office system for making all-ceramic restorations.
A, CAD/CAM in-office control unit with attached camera captures and stores images of the prepared teeth and bite relationship. Software designs the restoration and directs the milling unit on how to sculpt the restoration. B, Cracked lower first molar needing restoration. C, Cracked molar prepared for a ceramic onlay. D, Camera captures images of the prepared molar. E, The image of the molar and the margins marked in blue. F, Bite registration placed over the prepared molar. Its image will be captured, and computer software will configure the occlusal relationship with the ceramic onlay. G, Computer-generated occlusal contacts (blue) made from the bite registration. H, Milling unit that will sculpt the ceramic onlay from a ceramic block of the selected shade. I, Ceramic blocks in a variety of shades and sizes. J, Unpolished ceramic onlay tried on the molar to confirm its fit. K, Ceramic onlay after it has been polished and cemented. (Courtesy of Sirona Dental Systems, LLC and Todd Ehrlich [private practice in Bee Cave, TX] for clinical photographs.)
• The opposing teeth can be view in occlusion with the designed restoration and measurements of the restoration thickness can be made before milling, Thickness of the ceramic can be increased or decreased as needed and contours can be modified with the design software.
• The impression procedure is simplified because no cord packing or impression material is needed. Many potential sources of error are eliminated.
• The completed design of the restoration can be viewed and approved before milling is started.
• Machining eliminates the human error sometimes seen with processing steps done by a laboratory technician.
• Perhaps the most attractive feature is that dental offices that have these systems can prepare and deliver the restoration in the same visit. Patients like this convenience, and this can be a practice-building feature. This improves office efficiency and greatly speeds up the process. The patient needs to be given anesthesia for only one visit; digital scanning of the preparation speeds the “impression” process and no impression materials are needed; no die needs to be poured; no temporary crown is needed; and one cycle of breakdown and setup of the operatory with disposable supplies is eliminated. There is no laboratory fee, so with all of the areas of cost savings the system eventually pays for itself.
The very basics for operating a CAD/CAM system can be learned in a 2-day course. However, to become proficient and apply all of the features the systems offer, additional training and practice will be needed. Scheduling for restorative procedures that will use the system will need to be altered to accommodate the one-appointment mode. Initially longer appointments will be needed until the dentist and the staff become proficient with the system. Consideration will need to be made that at the same visit both preparation and cementation will take place as well as the steps needed to finish, polish, stain, and glaze the restoration.
Role of the Assistant/Hygienist: Many of the steps can be delegated by the dentist to her/his team members who also have undergone training. Training courses are available that are geared specifically for assistants or hygienists. Trained assistants or hygienists are capable of using the optical scanner to capture images of the prepared and adjacent teeth and the opposing occlusion. They can mark the location of the margins and design the restoration. They can initiate milling of the restoration, polish it, stain and glaze it if necessary, and prepare the restoration for bonding or conventional cementation as dictated by the material selected.
There are approximately 15,000 chairside CAD/CAM systems in use in the United States. That represents about 10% of general practices. Dentists who have the optical scanner but do not have the milling machine in their offices can electronically transmit digital images to a commercial laboratory using the CAD/CAM equipment to have a crown made. For those offices without a scanner or milling device, a conventional impression is made of the prepared teeth and sent to the laboratory, where the technician scans a die made from the impression, designs the restoration, and feeds the information to the milling machine. The technician can apply custom stain, polish, and glaze the restoration and, if needed, stack or press porcelain to high-strength cores.
Drawbacks of Introducing Chairside CAD/CAM into the Practice
Introducing a new technology to the practice is not without certain drawbacks:
• There is the initial expense of the system, periodic software updates, and routine maintenance. The dentist must determine how many of the esthetic restorations are typically done in the practice or will be done once the new equipment is installed. Is this going to be a cost-effective purchase or will it sit in a corner and collect dust?
• There is a significant learning curve that must be accommodated in the practice schedule. As a result there may be an initial loss of production. Patients may have extended time in the office waiting for new learners to use the system and process the restorations in a single visit. When things do not go as planned both the staff and the patient can get frustrated. So, the patient should be informed ahead of time that the appointment may be a long one.
• To provide good color matching of the restoration to the dentition, custom staining may be needed. This will require additional training and the purchase of a glazing oven.
• There are certain clinical scenarios in which an optical scanner will not be effective, such as preparations with deep subgingival margins. These situations may need cord placement or soft tissue modification with a laser or electrosurgery to expose the margins.
CAD/CAM Restorations
CAD/CAM technology can be used to produce monolithic (all the same material) single-unit inlays, onlays, crowns, and veneers. In addition, it can be used to make ceramic cores for crowns and bridges that are subsequently veneered with porcelain or other ceramic material. Implant abutments and metal partial denture frameworks can also be milled. Properly designed restorations made using CAD/CAM technology require fewer remakes; shorter seating time and adjustments; and better contours, contacts, and occlusion. Restorations have good marginal integrity that falls within the 50-micron (μm) parameter established by the American Dental Association.
Ceramic CAD/CAM Materials
Ceramic blocks made for CAD/CAM use have been produced under well-controlled conditions so that they are uniformly dense with no porosity. Porosities are weak points in the material that lead to the development of small cracks that propagate and eventually cause fracture of the restoration. In general, monolithic restorations are stronger than veneered restorations. Veneered restorations have the potential to chip or separate at the junction of the veneer material and the core material (called delamination).
Glass-Based CAD/CAM Materials
Machinable blocks of glass-based ceramic materials are available for fabrication of inlays, onlays, crowns, and veneers. Blocks of feldspathic porcelain include VITABLOCS Mark II (Vident/VITA) and ProCAD (Ivoclar Vivadent). Glass-based ceramic blocks are available as monochromatic (all one color) or multicolored layers (examples are VITABLOCS TriLuxe [Vident/VITA] or IPS Empress CAD Multi [Ivoclar Vivadent]). The resulting restorations are very esthetic and relatively strong once they are bonded. Lithium disilicate blocks (IPS e.max CAD; Ivoclar Vivadent) produce strong restorations that can be used for posterior crowns and three-unit fixed bridges (from premolars to anterior).
Nonglass Ceramic CAD/CAM Materials
Nonglass (crystalline) ceramics are used mostly as machinable blocks. These include aluminum oxide–based ceramics such as Procera AllCeram (Nobel Biocare), In-Ceram AL Block (Vident/VITA), and inCoris AL (Sirona) and zirconia-based ceramics such as Lava (3M ESPE), In-Ceram YZ (Vident/VITA), and IPS e.max ZirCAD (Ivoclar Vivadent). They have very high flexural strength (750 to 1200 MPa) and high fracture toughness. They are not very esthetic and must be veneered with more esthetic ceramics to be used in the anterior or visible areas in the posterior part of the mouth. They serve well as high-strength cores for crowns and bridges (Figure 9-2). To overcome the opacity of zirconia restorations 3M ESPE has developed a high-translucency zirconia material (Lava Plus) that is matched to the VITA shade guides. This should reduce the need for veneering to achieve esthetics in many applications.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses