Tooth agenesis is one of the most common developmental dental anomalies. Successful and satisfying dental treatment is always the goal for patients and dental practitioners, meaning that a patient’s needs are solved in a functional and esthetic way. Patients and dentists have to find the best way to reach their common goal of satisfaction. The authors introduce and provide examples of different approaches to solve the problem of congenitally missing lateral incisors. This article discusses the restorative approach, the approach using implants, and the orthodontic approach. In most cases, an interdisciplinary treatment plan has to be worked out and executed.
Tooth agenesis is one of the most common developmental dental anomalies in humans. Hypodontia describes the absence of 1 to 6 teeth, excluding the third molars. Oligodontia refers to the absence of more than 6 teeth, excluding the third molars, whereas anodontia represents the loss of all the teeth. The permanent dentition is more frequently affected than the primary dentition. There are large discrepancies in the prevalence of dental agenesis between different races. Tooth agenesis may appear as part of a recognized genetic syndrome or as a nonsyndrome, familial form, which occurs as an isolated trait. Recent genetic studies provide information regarding many genes related to both syndrome and nonsyndrome forms of human dental agenesis.
The causes of the most common hypodontia, third molars and incisor-premolar type, are still unknown. An association between PAX9 promoter polymorphisms and hypodontia has been reported, so there may be other promoter polymorphisms in genes involved in tooth organogenesis with these types of hypodontia. It is likely that other specific hypodontia genes still exist and will be identified eventually through contributions of molecular genetic research.
Successful and, therefore, satisfying dental treatment is always the goal for both patients and dental practitioners. What does this successful and satisfying treatment mean? It means that a patient’s needs are solved in a functional and, more importantly, an esthetic way. This is especially so in the anterior region, where patients react more negatively if the esthetic outcome is not perfect. But the problem dentists are facing is that each patient is an individual, with different parameters according to the smile, smile lines, biotypes according to the gingival tissue and health of the periodontium, habits, and sometimes parafunctional habits. Patients and dentists often face different approaches to achieve the final goal and together they have to find the best way to reach their common goal of satisfaction.
The authors’ aim in this article is to introduce and provide examples of different approaches to solve the problem of congenitally missing lateral incisors. Patients with congenitally missing lateral incisors face a problem that is in the middle of the esthetic zone and, therefore, crucial for their biosocial life. Maxillary lateral incisors are congenitally missing in approximately 1% to 2% of the population. They are the third most common congenitally missing teeth, after third molars and lower second premolars. This article discusses the restorative approach, the approach using implants, and the orthodontic approach. Even for the restorative and implant approaches, adjunctive orthodontic treatment is often required to redistribute and/or create the require spaces accordingly. Even if the spaces are closed with orthodontics, restorations may be needed to finish with an esthetic pleasant outcome. In most cases, an interdisciplinary treatment plan has to be worked out and executed. At the end of this article, a fourth approach is touched on, the autotransplantation of teeth. This is a complex interdisciplinary and technique-sensitive approach, but if experienced and skilled specialists are executing it, it can have terrific outcomes not only for congenitally missing lateral incisor cases but also for all sorts of missing teeth in the esthetic zone.
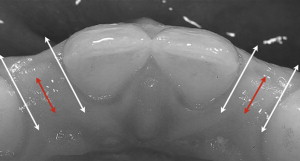
What is the clinical scenario? Imagine that a patient comes into an office and presents with congenitally missing lateral incisors ( Fig. 1 ). The patient is then confronted with the option of closing the spaces with canine substitutions or, alternatively, opening up the spaces for an implant or a restoration, such as an acid-etched retained bridge. All options are possible, but the patient is curious as to which one is the most esthetic? Which one is the most esthetic in the long term? What to tell this patient? Are there any established studies that compare the esthetic results of different methods of restoring the missing lateral incisors? Are there certain indications for one type of treatment plan over another when considering the malocclusion, smile line, and esthetics of natural teeth? This article aims to provide answers to these questions.

Orthodontic approach
The orthodontic approach is, in the authors’ opinion, the most conservative approach and is favorable if a patient meets certain requirements. These requirements are (1) malocclusion and (2) size, shape, and color of the canines.
According to Kokich and Kinzer there are two malocclusions that permit canine substitution (canine repositioning at the site of the lateral incisor). These are an Angle class II malocclusion, with no crowding in the mandibular arch, or an Angle class I malocclusion, with severe crowding in the lower arch where it is necessary to execute extractions. The final occlusion of both variants should end up in an anterior group function in lateral excursive movements.
When evaluating the size, shape, and color of the canine carefully, it can be predicted if recontouring alone is enough for an esthetic result or if the orthodontic treatment has to be combined with subsequent restorative treatment. The ideal canine for substitution has similar proportions in width and convexity as the lateral it should replace. Also, the color should be similar to the color of the central incisor. To establish the proper width, either contralateral incisor may be taken as a reference or some proportional calculations can be made. The authors favors Chu’s approach with the formula
Central incisor = width in mm = X
Lateral incisor = X − 2 mm
Canine = X − 1 mm
According to this formula by Chu, the canine that substitutes the lateral is approximately 1 mm too wide. That means that 0.5 mm of recontouring mesially and distally would have to be done to get the desired width. The convexity of the lateral incisor is more subtle than the convexity of the canine. Also, the canine normally shows in two planes mesiodistally whereas the lateral incisor has just one. It is also necessary to reshape the lingual surface of the canine to achieve a proper overjet and overbite relation, and the cusp tip of the canine needs enameloplasty as well.
If all this recontouring requires a significant amount of reduction of enamel, problems may occur. One of the problems that can be faced is that a patient experiences dental hypersensitivity, although Zacchrison and Mjör has shown that if all these reductions are performed using diamond instruments with abundant water spray cooling on young teeth, there are no long-term changes in tooth sensitivity. If dentin is exposed, an adjunctive restoration may be necessary.
Another problem that occurs is the color of the canine. Usually the canines are one to two shades darker than the central incisor. This problem can get even worse if a lot of reduction has to be performed to flatten a canine with a prominent labial convexity. As the enamel of the canine becomes thinner, the dentin starts to show through the translucent enamel and as a result the tooth appears even darker. One solution for the difference in color is single tooth bleaching, but with thinning the enamel the risk of sensitivity after bleaching increases. Another option is adjunctive restorative treatment.
The bracket placement in canine substitution cases is different. The bracket is not placed with the incisal edge of the canine as a reference but with the gingival margin as the guide. The gingival zeniths of the lateral incisors should be 0.5 to 1 mm lower than the central incisors, so the canine bracket has to be placed accordingly.
To make the final decision if a patient is suitable for the orthodontic approach and to anticipate if additional restorations may be necessary, the authors strongly suggest a carefully executed treatment plan. This treatment plan should include
-
Full radiographic work-up
-
Cephalometric analysis
-
Full esthetic work-up (esthetic evaluation form)
-
Model analysis for Angle classification and Bolton discrepancies
-
Model set-up, including the recontoured canine to predict the esthetic and functional result and the amount of reduction (width, labial convexity, incisal, and lingual eminence) necessary to achieve the result.
-
Advantages
-
If carefully planned and executed, the orthodontic approach is the most conservative approach ( Figs. 2 and 3 )

Fig. 2 Orthodontic approach during treatment.
Fig. 3 Orthodontic approach during treatment. -
Long-term esthetic results
-
Superior esthetic outcome compared with implants and Maryland bridge according to cohort study
-
Psychological comfort that the patient has no missing teeth.
-
-
Disadvantages
Implant approach
A second option for replacing congenitally missing lateral incisors is to use implant-retained prostheses. In particular, in cases of adjacent teeth devoid of any fillings or color or size issues, placing a single tooth implant may be regarded as the most conservative approach. In addition, various studies have proved that single tooth implants have an excellent long-term result regarding osseointegration and function. This is not the case for esthetics, however, because attainment of esthetic rehabilitations with dental implants in the anterior area is currently one of the leading challenges in modern dentistry. The main treatment goals are intact papillae and harmonious gingival contours without any recession of the buccal soft tissue. The height of the peri-implant papillae for single tooth implants is not determined by the peri-implant bone level but rather the bone level of the adjacent teeth. Therefore, an optimal 3-D implant placement should include at least 1.5 mm of distance between the implant and the adjoining teeth ( Fig. 6 ). Additionally, as in most cases, soft and hard tissue structure is missing; augmentative procedures have to be performed at the time of implant placement or at the time of abutment connection.
Several criteria have to be considered before placing a single tooth implant in adolescents:
- 1.
Time of implant placement
- 2.
Development of a proper implant site
- 3.
Space needed coronally
- 4.
Space needed apically
- 5.
Height of gingiva
- 6.
Retention of space needed before implant placement.
Time of Implant Placement
It is of major importance when considering implant-retained prostheses to evaluate if the skeletal growth of a patient is still active. Studies have demonstrated that craniofacial growth continues on average until age 17 for women and 21 for men. A more precise estimation of the individual growth pattern of an implant patient can be performed, however, with hand-wrist radiographs. A second option is to use the cervical vertebral maturation developed by Baccetti and colleagues, who produced diagrammatic drawings and descriptions of 6 stages of cervical vertebral maturation. They evaluated the cervical maturation by the changes in the concavity of the lower border, height, and shape of the vertebral body. When considering implant placement, deep concavities have to be observed on the second, third, and fourth cervical vertebrae, and the vertebral bodies display a greater vertical than horizontal dimension (completion phase). This information can be retrieved from a lateral cephalometric radiograph, which is routinely obtained by an orthodontist. The most precise instrument to assess the completion of the facial growth is superimpositions of lateral cephalometric radiographs. These radiographs should be obtained 6 months to 1 year apart. The facial growth can be regarded as complete if the distance from nasion to menton is stable within 1 year.
Development of a Proper Implant Site
To achieve a predictable and esthetically satisfying implant outcome, it is crucial to have a properly developed implant site ( Fig. 7 ). The buccolingual dimension of the alveolar ridge has to be wide enough to allow a surgeon to place the implant in a correct 3-D position.

If the buccolingual dimension is insufficient, a bone graft may be necessary. An ideal method to develop a proper width of the alveolar ridge can be achieved if the canine erupts next to the central incisor. The buccolingual width of the canine creates a sufficient width of the ridge when erupting. After eruption, the canine can be distalized orthodontically and, therefore, establish a proper buccopalatal width of the alveolar ridge. Studies have demonstrated that if an implant site is developed with this kind of orthodontic guided tooth movement, the buccopalatal width remains stable. Distalizing may need to be done with bodily movement to develop adequate space between the roots. If a panoramic radiograph reveals that the permanent canine is apical to the primary canine, the extraction of the primary lateral incisor may be considered to guide the eruption of the permanent canine toward the central incisor. This (as explained previously) is favorable for developing a proper implant site. Otherwise, it may not be possible to guide the eruption of the canine near the central incisor, the osseous ridge will not fully develop, and the buccopalatal width will be insufficient for a proper implant placement. In these cases, it is necessary to perform a bone graft before or at the time of implant placement to achieve a sufficient dimension of the alveolar ridge.
Space Needed Coronally
The assessment of the space available mesiodistally is crucial to evaluate the diameter of the implant. In unilateral congenitally missing lateral incisor cases, the contralateral lateral incisor may be used for assessing the proper mesiodistal space needed. In cases of peg-shaped contralateral lateral incisors or when both lateral incisors are congenitally missing, other tools have to be used. One of these tools may be a formula initiated by Chu :
Central incisor = X
Lateral incisor = X − 2 mm
Canine = X − 1 mm
Another way to estimate the correct dimension of the lateral incisiors is to use the Bolton analysis. By this means, the mesiodistal widths of the arches can be compared to achieve an ideal occlusal relationship. It is an easy and efficient way to mathematically calculate the proper width of the missing lateral incisor. The best tool, however, for assessing the ideal width of the missing lateral incisor is a diagnostic wax-up. In particular, for multidisciplinary cases, it facilitates an overview for both the orthodontist and the restorative dentist. Another advantage is the visualization for patients so that the final outcome can be imagined and patients can provide input into alterations of the esthetic outcome.
Attention has to be given to the minimal mesiodistal width that is needed for the implant per se. A minimum of 5.5 mm is required. There should be at least 1 mm distance between the implant and the adjacent teeth; otherwise, the interproximal bone could be jeopardized, and the space for the papilla between the implant crown and adjacent teeth is constricted and appears much shorter than the papillae on the contralateral side. A disagreeable esthetic outcome would be the result.
Space Needed Apically
Careful attention has to be paid to the distance of the apical roots between central incisor and canine. A minimum of 5 mm is required generally to provide sufficient space for a 3.5-mm implant. This space has to be provided by an orthodontist, who controls the mesiodistal root angulation when creating space for an implant. During this process of creating space, the mesiodistal space coronally is achieved earlier due to a so-called tipping movement, followed by a change of the mesiodistal angulation of the roots. It is crucial not to rely on the appearance of the mesiodistal distance of the coronal aspect, which is achieved earlier than the proper mesiodistal distance of the roots. Not paying attention to this aspect leads to too early removal of the orthodontic appliances and, therefore, insufficient space between the roots. To prevent this mistake, radiographs of this particular area should be made to make sure that sufficient interradicular space is created before removal of orthodontic appliances.
Height of Gingival Margins
In most implant systems, the distance between the head of the implant and the future gingival margin has to be 4 mm ( Figs. 8 and 9 ). In adolescents, many times the alveolar bone is at the level of the cementoenamel junction of the adjacent teeth. In comparison, in adults, the alveolar bone is 2 mm apical to the cementoenamel junction. Thus it is sometimes necessary in adolescent patients to perform gingival surgeries, including or excluding bone removal, before the implant placement can be done.


Another aspect of the gingival papillae is that when teeth are moved in adults during space opening, the papilla remains stationary and the adjacent sulci are averted. The nonkeratinized gingiva appears red at first and keratinizes over time; just the papilla itself does not move. The good news is that most patients are treated during adolescence; thus, this phenomenon of a stationary papilla does not occur with them. Therefore, there are no esthetic issues with the papillae adjacent to the lateral incisor implant in adolescents.
Retention of Space Needed Before Implant Placement
As discussed previously, as a general guide, implants can be placed in women at approximately age 17 and in men at approximately age 21. At these ages, craniofacial growth is generally completed. Treatment of these patients should start before this age because development of the alveolar ridge has to be achieved and coronal space and interradicular space has to be created. That leads to a period of time when space maintenance may have to be provided for a patient, if craniofacial growth is not yet completed. The temporization and stabilization depends on the waiting time until the implant may be placed. If patients are ready for implant placement in a couple of months, a removable retainer, such as a Hawley retainer or an Essix retainer with a built-in prosthetic tooth, can be used. If patients have to wait 1 or 2 years before completion of growth is achieved, a temporary resin-bonded bridge is the more favorable option.
-
Advantages of implant approach
-
No adjacent teeth have to be prepared (see Figs. 7–9; Fig. 10 )
-







