Radiographic images have always been an important part of orthodontic diagnosis and treatment planning. We have been limited by the two-dimensional nature of these radiographs as we pursue tooth movement in a three-dimensional fashion. This article shows the current and future uses and advantages of cone-beam CT in the practice of orthodontics. The use of this technology in the near future will change the way records are taken and treatment is rendered. With this added diagnostic knowledge, orthodontic treatment will assuredly become not only more high tech but also higher quality.
Orthodontists have routinely treated patients’ malocclusions by applying forces in all three planes of space. The movement of alveolar bone may be accomplished in two directions: in a transverse direction, using a rapid maxillary expansion appliance, or in a sagittal direction, using a headgear or Herbst appliance. Tooth movement alone may also be accomplished using archwires and elastics, as evidenced by the vertical movement of teeth using vertical or box interarch elastics. For years, these three-dimensional (3D) movements have been diagnosed and treatment planned based on two-dimensional (2D) imaging. Cephalometric, panoramic, and periapical radiographs are a few of the 2D radiographs routinely used in orthodontic planning. Although these images have been the standard of care and are useful in assessing skeletal and dental relationships, their 2D diagnostic information can leave some questions unanswered in selected cases. This article discusses the application of cone-beam CT (CBCT) in various orthodontic tasks, from simple to more advanced. It also takes a glimpse into the future to determine how CBCT may become a normal part of high-tech orthodontic treatment.
Common diagnostic radiographs
Cephalometric radiology was introduced to orthodontics in 1931 by Broadbent in the United States and Hofrath in Germany. They developed standardized methods for obtaining these radiographs using cephalostats to facilitate reproducible head positioning for films taken at different time points . These cephalometric radiographs are heavily relied on by orthodontists today to measure angular and linear dimensions using various anatomic landmarks. “Cephalometric” images constructed from CBCT scans have been shown to be as accurate as, or in some cases more accurate than, conventional 2D lateral cephalometric radiographs . Additionally, lateral cephalometric radiographs constructed from the CBCT scans can use the information from the right and/or left half of the skull. Constructing these images using one half of the skull can overcome the problem faced with superimposition of the right and left ramus, body, molars, and mandibular condyles.
The panoramic radiograph was first proposed and experimented with in the 1930s by Dr. H. Numata of Japan. In the mid-1940s, the father of panoramic radiography, Dr. Yrjo Veli Paatero of Finland, refined the panoramic technique . Since then, 2D panoramic radiography has been further refined and brought to a level previously unattained. The images made with these modern digital panoramic machines are clear and diagnostic; however, positioning errors and arch and teeth variations may have an effect on diagnostic efficacy. CBCT scans allow an infinite number of focal troughs to be specified and reformatted, compensating for arch variations. Also, separate “panoramic” radiographs can be obtained from the CBCT data, focusing on the maxillary arch and the mandible. Linear and angular dimensions have been shown to be more accurate using the CBCT panoramic images, compared with traditional panoramic radiographs, which is also true when viewing the condyles .
Several other views, projectional and tomographic, are used in orthodontics, but not as frequently. Most of these images can be reconstructed from the CBCT data if a CBCT scan has been acquired.
The contribution of CBCT in various diagnostic tasks is discussed in the following paragraphs.
Impacted canines
Possibly the most recognized need for CBCT imaging in orthodontics is that of impacted canine evaluation. The prevalence of impacted maxillary canines is approximately 0.9% to 3.0% . The ratio of palatal to labial impactions has been shown to be as high as 9:1 . Studies have been carried out relating the position of the impacted canine to the success of uncovery and orthodontic traction .
In the past, orthodontists have used the tube shift technique to compare two periapical radiographs taken at different beam angles to determine the facial/lingual position of the impacted canine. This same lingual, opposite buccal rule is helpful in determining whether the impacted canine is labial or lingual to the incisor roots; however, the degree of displacement is difficult to determine. CBCT imaging is precise in determining not only the labial/lingual relationship but also a more exact angulation of the impacted canine. These 3D images are beneficial in determining the proximity of adjacent incisor and premolar roots, which can be invaluable in determining the ease of uncovering and bonding and the vector of force that should be used to move the tooth into the arch with a lesser chance of adjacent root resorption.
A standard periapical radiograph of an impacted maxillary left canine (#11) is shown in Fig. 1 A . This single film gives limited information about canine position or possible adjacent root resorption. The palatal location of the canine is obvious in the axial view of the CBCT scan using Dolphin 3D (Dolphin Imaging and Management Solutions, Chatsworth, California), in Fig. 1 B. A view of the proximity of the canine to the central incisor (#9) is shown in the CBCT sagittal transparent hard tissue image in Fig. 1 C. The two teeth are not in contact with one another, and no resorption is evident on the central incisor. A different type of image using the same Dolphin 3D software and CBCT data package is seen in Fig. 1 D. This view shows the much closer relationship of the same canine to the adjacent lateral incisor (#10). No root resorption is obvious in the images. The uncovery, bonding, and direction of force vector for #11 is enhanced significantly by the knowledge supplied to the oral surgeon and orthodontist.
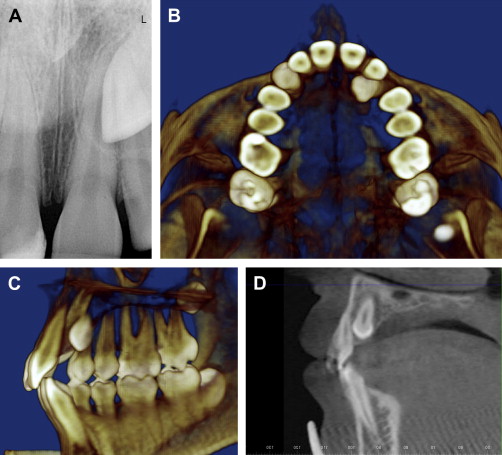
One should note that the four views in Fig. 1 are all static images made from a 3D CBCT scan. Using software like Dolphin 3D, the doctor can rotate the 3D skull, allowing for cuts at various angles to aid in visualization. The plane of view can be moved through the entire skull in all three axes of space. Some clinicians are now suggesting that tissue and bony uncovery of the significantly palatally displaced and impacted canines without orthodontic traction would allow these teeth to drift into the oral cavity spontaneously; they then may be bonded some months later by the orthodontist . The enhanced knowledge of canine position supplied by the CBCT scans will aid the orthodontist as he or she determines whether to simply uncover the palatally impacted canine or apply immediate traction.
Impacted canines
Possibly the most recognized need for CBCT imaging in orthodontics is that of impacted canine evaluation. The prevalence of impacted maxillary canines is approximately 0.9% to 3.0% . The ratio of palatal to labial impactions has been shown to be as high as 9:1 . Studies have been carried out relating the position of the impacted canine to the success of uncovery and orthodontic traction .
In the past, orthodontists have used the tube shift technique to compare two periapical radiographs taken at different beam angles to determine the facial/lingual position of the impacted canine. This same lingual, opposite buccal rule is helpful in determining whether the impacted canine is labial or lingual to the incisor roots; however, the degree of displacement is difficult to determine. CBCT imaging is precise in determining not only the labial/lingual relationship but also a more exact angulation of the impacted canine. These 3D images are beneficial in determining the proximity of adjacent incisor and premolar roots, which can be invaluable in determining the ease of uncovering and bonding and the vector of force that should be used to move the tooth into the arch with a lesser chance of adjacent root resorption.
A standard periapical radiograph of an impacted maxillary left canine (#11) is shown in Fig. 1 A . This single film gives limited information about canine position or possible adjacent root resorption. The palatal location of the canine is obvious in the axial view of the CBCT scan using Dolphin 3D (Dolphin Imaging and Management Solutions, Chatsworth, California), in Fig. 1 B. A view of the proximity of the canine to the central incisor (#9) is shown in the CBCT sagittal transparent hard tissue image in Fig. 1 C. The two teeth are not in contact with one another, and no resorption is evident on the central incisor. A different type of image using the same Dolphin 3D software and CBCT data package is seen in Fig. 1 D. This view shows the much closer relationship of the same canine to the adjacent lateral incisor (#10). No root resorption is obvious in the images. The uncovery, bonding, and direction of force vector for #11 is enhanced significantly by the knowledge supplied to the oral surgeon and orthodontist.
One should note that the four views in Fig. 1 are all static images made from a 3D CBCT scan. Using software like Dolphin 3D, the doctor can rotate the 3D skull, allowing for cuts at various angles to aid in visualization. The plane of view can be moved through the entire skull in all three axes of space. Some clinicians are now suggesting that tissue and bony uncovery of the significantly palatally displaced and impacted canines without orthodontic traction would allow these teeth to drift into the oral cavity spontaneously; they then may be bonded some months later by the orthodontist . The enhanced knowledge of canine position supplied by the CBCT scans will aid the orthodontist as he or she determines whether to simply uncover the palatally impacted canine or apply immediate traction.
Other impacted teeth
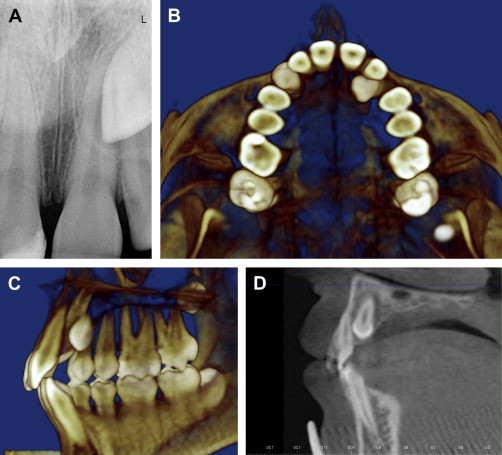
Various other teeth become impacted less often than canines but still pose a significant orthodontic challenge. Maxillary central incisors can be impacted and displaced subsequent to the presence of a mesiodens. Fig. 2 shows a CBCT image of an impacted tooth # 9 subsequent to such a mesiodens. Never before have we been able to determine such an exact position of these displaced and impacted central incisors. The position of these teeth and the root and crown morphology can be evaluated. This knowledge can help determine the desirability of retaining and placing traction on these impacted teeth. Many times, the orthodontist is the first to recognize the presence of supernumerary teeth or odontomas in the young patient. Two-dimensional radiographs, especially panoramic ones, can make definitive diagnosis of an early-forming supernumerary tooth difficult. The CBCT image allows a more exacting view to help determine the presence and position of these unwanted surprises.
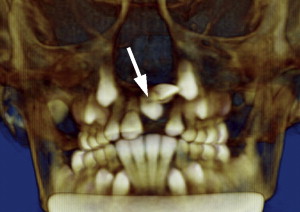
Second molars can also become impacted and malpositioned, which can be caused by ectopically positioned adjacent third molars or second molar follicles that are inexplicably tipped in an oblique or horizontal orientation. If impinging third molars are not diagnosed and extracted appropriately, temporary or permanent delay in the eruptions of the second molars can be the result. Early diagnosis of these problems can lead to a significantly better prognosis of acceptable second molar eruption lending itself to orthodontic positioning on entry into the oral cavity. The author has found no other technique to compare with the diagnostic ability of the CBCT image in these situations. Fig. 3 shows a deviantly positioned third molar (#16) that was inhibiting proper eruption of tooth #15.

At times, the orthodontist desires to reposition the maxillary anterior teeth slightly in a first phase of treatment. On viewing the records, a mesiodens can be an unanticipated finding. If the oral surgeon wants to leave this mesiodens, and postpone its removal until a later date, the position of the mesiodens can be important. Delaying tooth movement must be considered if the mesiodens is in close proximity to the roots of the incisors. The orthodontist may pursue limited movement without significant fear of complications if the mesiodens in question is some distance from the roots. Using these images, the orthodontist and oral surgeon can combine their knowledge to establish a treatment plan that directs attention to the timing of mesiodens removal.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


