Cone beam computed tomography has gained acceptance in the endodontic community for assistance with diagnosis, treatment, and evaluation of outcomes. This article reviews a multitude of applications, from basic principles to clinical applications, using specific cases and supporting literature to demonstrate the benefits for both the specialist and general practitioner.
Key points
- •
Narrow field CBCT has many applications in Endodontics and reduces the negative effects of anatomic noise, geometric distortion and technique sensitivity observed on 2D images.
- •
Narrow field CBCT provides earlier detection of apical periodontitis than conventional 2D radiographs providing improved diagnostic value, treatment efficiency and outcome assessment.
- •
Narrow field CBCT provides excellent image resolution at reduced radiation exposure as compared to mid or large field of view CBCT.
- •
CBCT assists the practitioner to identify canal morphology, numbers of canals and relative positioning even in the presence of calcific metamorphosis and dystrophic calcifications.
- •
Identification and treatment of lateral canals is supported by viewing their specific location with the use of narrow field of view CBCT before or during endodontic therapy.
Introduction
According to the Merriam-Webster dictionary, the term “diagnosis” is defined as: “the art or act of identifying a disease from its signs and symptoms.” In the field of endodontics, dentists review a multitude of signs and symptoms to formulate their diagnosis. These include, but are not limited to: sensitivity to heat, sensitivity to cold, percussion, palpation, bite, swelling, caries, periodontal disease, presence of sinus tracts, and unstimulated pain. In addition to these symptoms, tests are used to identify variations from normal such as electric pulp tests, laser Doppler, and radiographs (first used in 1896 by Otto Walkhoff). In the early 1960s Seltzer and Bender identified several discrepancies using 2-dimensional (2D) radiographs for observing apical periodontitis (AP). These included: (a) a delayed appearance of radiographic evidence of AP until 40% cortical plate demineralization developed and (b) a lack of correlation between the size of the histologic defect and AP image.
In addition, according to Durack and Patel, 2D radiographs are of limited value due to the compression of 3-dimensional (3D) structures, geometric distortion, anatomic noise, and temporal perspectives.
Radiographs are used to identify the changes inside visually opaque objects. Although interpretations of these images are only part of the diagnostic process, the dental community places great emphasis on this information. In the early 1970s, Brynolf studied the benefit of using radiographs from multiple angles to increase their diagnostic value. She found that using 3 images improved diagnosis significantly. Later that decade, grave concerns developed. Many articles published supported the idea that reading dental radiographs was too subjective. To this concern, Orstavik and colleagues developed a guide to standardize apical observations called the Periapical Index. Despite these efforts, 2D radiographs were still limited in diagnostic value due to the factors previously listed.
Computer-assisted tomographic imaging or cone beam computed tomography (CBCT), a technology borrowed from medicine, previously focused on the need for better surgical guidance during implant placement. The principle of ALARA (As Low As Reasonably Achievable) as related to radiation exposure and the lack of resolution initially limited CBCT use in endodontics. A new area of research emerged, and old paradigms were shifting. These advances solved many of the listed 2D limitations. Specific applications of this technology developed and the Endodontic community embraced them.
The current narrow field of view CBCT provides a 3D, low-radiation/high-resolution solution to many endodontic diagnostic and treatment problems. This article will display specific case scenarios and supporting literature for the application of CBCT technology.
Introduction
According to the Merriam-Webster dictionary, the term “diagnosis” is defined as: “the art or act of identifying a disease from its signs and symptoms.” In the field of endodontics, dentists review a multitude of signs and symptoms to formulate their diagnosis. These include, but are not limited to: sensitivity to heat, sensitivity to cold, percussion, palpation, bite, swelling, caries, periodontal disease, presence of sinus tracts, and unstimulated pain. In addition to these symptoms, tests are used to identify variations from normal such as electric pulp tests, laser Doppler, and radiographs (first used in 1896 by Otto Walkhoff). In the early 1960s Seltzer and Bender identified several discrepancies using 2-dimensional (2D) radiographs for observing apical periodontitis (AP). These included: (a) a delayed appearance of radiographic evidence of AP until 40% cortical plate demineralization developed and (b) a lack of correlation between the size of the histologic defect and AP image.
In addition, according to Durack and Patel, 2D radiographs are of limited value due to the compression of 3-dimensional (3D) structures, geometric distortion, anatomic noise, and temporal perspectives.
Radiographs are used to identify the changes inside visually opaque objects. Although interpretations of these images are only part of the diagnostic process, the dental community places great emphasis on this information. In the early 1970s, Brynolf studied the benefit of using radiographs from multiple angles to increase their diagnostic value. She found that using 3 images improved diagnosis significantly. Later that decade, grave concerns developed. Many articles published supported the idea that reading dental radiographs was too subjective. To this concern, Orstavik and colleagues developed a guide to standardize apical observations called the Periapical Index. Despite these efforts, 2D radiographs were still limited in diagnostic value due to the factors previously listed.
Computer-assisted tomographic imaging or cone beam computed tomography (CBCT), a technology borrowed from medicine, previously focused on the need for better surgical guidance during implant placement. The principle of ALARA (As Low As Reasonably Achievable) as related to radiation exposure and the lack of resolution initially limited CBCT use in endodontics. A new area of research emerged, and old paradigms were shifting. These advances solved many of the listed 2D limitations. Specific applications of this technology developed and the Endodontic community embraced them.
The current narrow field of view CBCT provides a 3D, low-radiation/high-resolution solution to many endodontic diagnostic and treatment problems. This article will display specific case scenarios and supporting literature for the application of CBCT technology.
Roots: anatomic noise hides anatomy
Case #1: Maxillary Left First Bicuspid—Diagnosis: Pulpal Necrosis/Symptomatic Apical Periodontitis
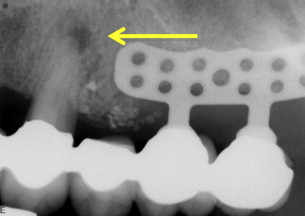
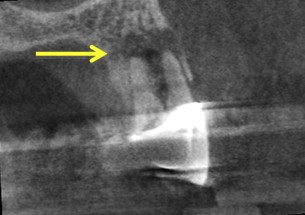
Identification of root structure, curvature, and location are hampered in 2D radiographs by anatomic noise ( Fig. 1 ). In this case, CBCT ( Figs. 2 and 3 ) assisted with the preoperative identification of the presence, location, shape, and lengths of 3 separate distinct roots. Note the accurate orientation, size, and location of apical periodontitis clearly observed on sagittal (see Fig. 2 ) and coronal views (see Fig. 3 ). Treatment is clearly supported by preoperative knowledge of root anatomy.

Canals: hidden canal morphology
Case #2: Mandibular Left First Molar, Diagnosis: Irreversible Pulpitis/Symptomatic Periodontitis
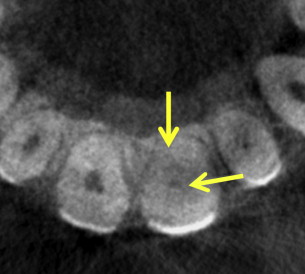
Preoperative identification of the number, location, and length of canals is facilitated with a CBCT scan ( Figs. 4–7 ). Successful endodontic treatment depends on treating all canals (see Fig. 7 ). In tooth #19, a midmesial canal is observed on the preoperative axial scan (see Fig. 5 ) and verified clinically (see Fig. 6 ).




Calcifications
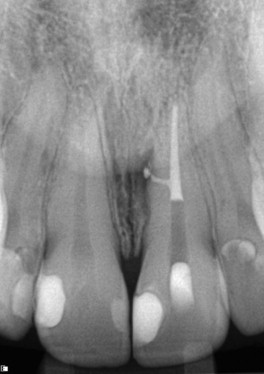
Case #3: Maxillary Left Central Incisor Diagnosis—Pulpal Necrosis/Symptomatic Apical Periodontitis
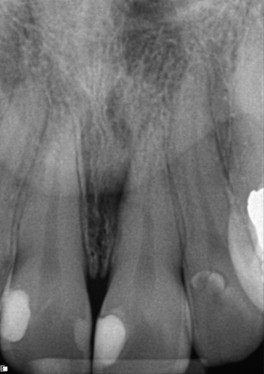
Canal obliteration may represent dystrophic calcifications (DC, calcification of degenerating or necrotic tissue pulp stones ) or calcific metamorphosis (CM, A process of mineralization after trauma ) ( Figs. 8–11 ). The mechanism for dentin deposition in CM has been debated by the profession and is still unclear. It has been suggested that the severity of the injury may be related to the rate of deposition. The predominance of literature suggests that despite the appearance of CM on a 2D radiograph, a narrow pulp canal space persists (see Figs. 9 and 10 ). With the development of CBCT, pretreatment identification and location of this narrow pulp space can facilitate minimally invasive treatment.



Lateral canals
Case #4: Maxillary Left Central Incisor Diagnosis—Pulpal Necrosis/Symptomatic Apical Periodontitis
Treatment of lateral canals requires pretreatment knowledge of their presence and location ( Figs. 12–15 ). 2D radiology does not provide adequate information to predictably locate and treat this entity. Successful endodontic treatment depends on the adequate debridement of bacteria from all spaces. CBCT technology assists the practitioner with identifying the specific location of lateral canals (see Figs. 13 and 14 ). Overcoming the obstacle of identifying and locating lateral canals enhances the ability to treat these difficult cases (see Fig. 15 ).


Bone morphology identifiable on CBCT
Fenestration Case #5
Identification of a fenestration can assist in planning apical surgery ( Figs. 16–18 ). CBCT offers the opportunity to accurately evaluate an area of apical periodontitis for size, volume, and location before surgery. Some studies find no value in apical grafting, while others advocate that the need for grafting is based on the volume of the space to be grafted. These studies suggest that larger lesions may not heal successfully from apical surgery without grafting, due to a lack of clot stability. CBCT can be used to determine the volume of the apical periodontitis lesion. Future research may be able to identify the specific volumetric limits for clot stability and graft usage as opposed to the linear measurement currently used.





