The use of conebeam computed tomography (CBCT) carries with it medicolegal risks of which the practitioner should be aware. These include licensing and malpractice liability concerns. A practitioner who intends to take and/or use CBCT scans should seek advice from his malpractice carrier before doing so. All scans should be read by someone competent to interpret them. Using the services of an out-of-state radiologist to read scans poses its own set of risks. Consultation with a malpractice carrier and dental boards is advisable in this situation.
Key points
- •
The use of cone beam computed tomography (CBCT) carries with it medicolegal risks of which the practitioner should be aware. These include licensing and malpractice liability concerns.
- •
A practitioner who intends to take and/or use CBCT scans should seek advice from his malpractice carrier before doing so.
- •
All scans should be read by someone competent to interpret them.
- •
Using the services of an out-of-state radiologist to read scans poses its own set of risks.
- •
Consultation with a malpractice carrier and dental boards is advisable in this situation.
Introduction
As technology such as cone beam computed tomography (CBCT) advances apace in dentistry, clinicians who embrace it should understand the potential liabilities and risks associated with the technology. However, the decision to use or not to use new technologies within a practice or on an individual patient should be based on clinical considerations, not on legal ones. Nevertheless, once a decision has been made, clinicians would be well advised to understand the legal implications of their decision and how they use or do not use the new technology. Although the preceding statements apply to all aspects of dentistry, in this article the focus is on CBCT. The reader should bear in mind that in the United States, laws vary from state to state. Thus, a dentist should always seek the advice of an attorney or malpractice carrier to ascertain the law in his or her own state.
Introduction
As technology such as cone beam computed tomography (CBCT) advances apace in dentistry, clinicians who embrace it should understand the potential liabilities and risks associated with the technology. However, the decision to use or not to use new technologies within a practice or on an individual patient should be based on clinical considerations, not on legal ones. Nevertheless, once a decision has been made, clinicians would be well advised to understand the legal implications of their decision and how they use or do not use the new technology. Although the preceding statements apply to all aspects of dentistry, in this article the focus is on CBCT. The reader should bear in mind that in the United States, laws vary from state to state. Thus, a dentist should always seek the advice of an attorney or malpractice carrier to ascertain the law in his or her own state.
To scan or not to scan: the standard of care
Unlike drugs that must be approved by the Food and Drug Administration for specific indications before they can be put on the market, the same is not true of devices such as CBCT machines. Although all radiographic equipment has to meet federal and state guidelines, it is generally not approved for a particular purpose or indication. For new techniques and technologies for which there are no “standards of care” or long-established or accepted guidelines for their appropriate use, the issue of when and how to use them can be quite problematic for clinicians. A standard of care can be mandated only by a legislature, a court, and a dental board. It is rare, although not unheard of, for the first two to do so. For a case in which a court mandated a standard of care for eye examinations, see Helling v Carey.
Dental boards may create a standard of care through their regulations. For example, the Massachusetts Board of Registration in Dentistry specifies what the patient record shall contain. Such a regulation may set a standard of care. There is no private group or association, no matter how esteemed, that is recognized as having the legal authority to establish the standard of care. Neither is there any group that has the authority to mandate a formal process by which a new procedure becomes the standard of care. It is almost universally true that the standard of care is determined by what clinicians actually do in practice. By way of example, in Massachusetts the standard of care is determined by “the degree of care and skill of the average qualified practitioner.” In Washington State, the standard is determined by “a reasonably prudent practitioner.” It is thus up to the profession acting through individual practitioners to decide on the appropriate use of the technology. Professional groups, including speciality organizations, do, however, issue “guidelines for use” or “position papers” on new technologies to help clinicians understand accepted applications, although these do not have the force of law.
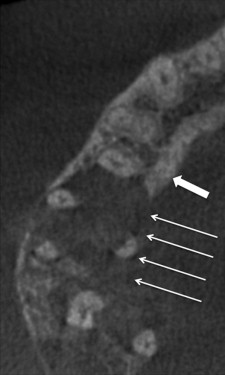
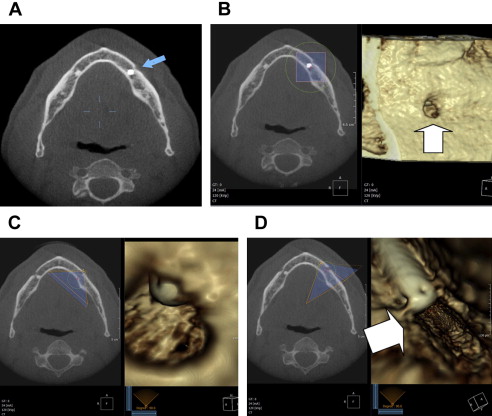
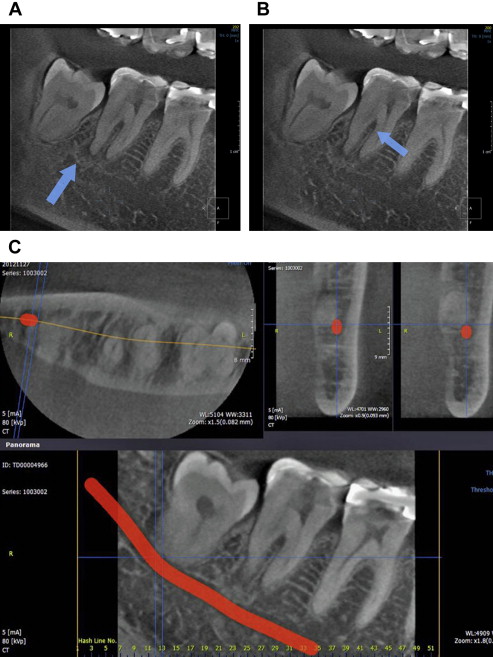
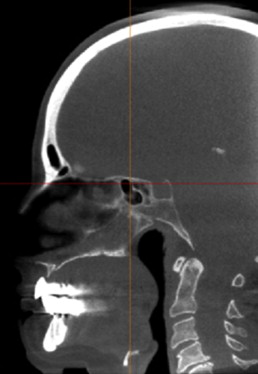
In practice, the use of CBCT may be driven in part by vendors of the equipment, who have a pecuniary interest in their sale and use. Although their interest is legitimate, it is not a legitimate interest for practitioners. At the present time, it can be stated that the use of CBCT is well accepted in implant planning ( Fig. 1 ) and endodontics ( Fig. 2 ), for each of which a position paper exists. The use of CBCT is also well accepted to evaluate impacted teeth. A patient with multiple impactions ( Fig. 3 ) illustrates this application. CBCT’s use in the evaluation of complex orthodontic and orthognathic cases, such as patients with asymmetries and syndromes, is accepted. Indeed, medical CT was used in such patients long before CBCT became available. Parenthetically, it should be emphasized that to say that the use of CBCT is well accepted is not to imply that its use is mandatory in all or even most cases in any of the dental disciplines.
In the early stages of a new modality, in this case CBCT, a reasonable starting point for a clinician trying to decide when a scan is indicated would be to follow position statements that are endorsed by professional organizations, as well as to ascertain what other dentists in practice are doing. The latter can be done by asking colleagues, by attending conferences, and by reading reputable journals. Unfortunately, in the American system of jurisprudence, a practitioner is far more likely to be sued for not using technology as opposed to being sued for using it. Thus, the inclination to use new technologies, including CBCT, is driven in part by the fear of malpractice.
Another indication that a procedure has become clinically accepted is when third-party payers decide to cover the cost of such care. In medicine, Medicare and Medicaid usually lead the way, with private payers often following their leads on whether to cover a procedure. Decisions by third parties, governmental or private, are not the final word on whether a procedure is clinically accepted or constitutes the standard of care; that is decided by what the average qualified practitioner does. However, a decision to pay is more meaningful than a decision not to cover a procedure, as the motivation for the latter may be primarily a cost-containment measure. In dentistry, where the use of the word insurance is really misleading, a decision not to cover a procedure commonly involves primarily or exclusively financial considerations for third party payers. Thus, in dentistry, the decision to cover a procedure is much more significant than a decision to deny coverage.
For a comprehensive discussion on how new technologies and procedures may become the standard of care, see the article by Friedland.
Technical parameters
Proper technical parameters are important to obtain a clinically acceptable scan. Improper technical parameters also may lead to liability. These include selecting a low-resolution setting (0.3 mm voxel or higher) for a task requiring high resolution (0.2 mm voxel and lower) and selecting an inappropriate field of view (FOV). The reader should be aware that when it comes to resolution, a higher number means that the resolution is worse, and vice versa. For example, a scan done at a resolution of 0.3 mm voxel has a higher resolution than a scan done at 0.4 mm voxel. Spatial resolution is expressed in line pairs/millimeters or voxel size. For practical purposes, it can be defined as the ability of an imaging modality to differentiate 2 objects, or as the fineness of detail that can be observed in an image. Low spatial resolution techniques will be unable to differentiate between 2 objects that are close together and may be unable to discern a small object, such as a fracture in a tooth. The FOV refers to the physical size of the anatomy that is covered by the exposure, usually selectable from about 37 × 50 mm (typically for a single endodontic procedure) up to as large as 20 × 20 cm (eg, an orthodontic or oral and maxillofacial surgery patient).
Owners and operators of CBCT equipment should be familiar with the technical parameters required for a specific examination. Unfortunately, many dentists who install a machine are not adequately trained to fully understand and take advantage of their machine’s capabilities. Common errors include a scan with an FOV that is too large or too small. A larger FOV than is necessary has at least 2 deleterious effects. It results in a less optimal image (the larger the FOV, the greater the scatter and the less detailed the image) and a greater patient dose. Although increased scatter and dose are not likely to result in liability, a wider FOV than is necessary does have medicolegal implications as far as interpretation of the image is concerned, an issue that is discussed later in this article. A too small FOV may preclude the ability to interpret the image correctly. Some machines also allow the operator to control or select the kilovoltage and milliamperage. Selecting too low a milliamperage setting may result in a poor scan by reducing the number of resultant x-ray photons available, resulting in a less than optimal scan, often with much soft tissue scatter, and thus poor image quality for interpretation. Too high a milliamperage setting will result in increased dose. Understanding these parameters is critical to producing the best diagnostic quality scan.
Resolution
When one is looking at very small structures, such as individual canals or fractures of teeth, it stands to reason that a high-resolution image is necessary. In a 2009 article, it was stated that for endodontics the minimally acceptable resolution should not exceed 200 μm (0.2 mm). With current machines capable of much higher resolutions, in the range of 0.07 mm and better, endodontic scans today should be done at or near the highest resolution possible. Should a practitioner do a scan for endodontic purposes at too low a resolution, the information being sought may not be depicted. Such a scan would be inadequate for the purpose for which it was taken and could result in liability for anything missed that would have been visible on a scan done with appropriate resolution. In addition to the resolution selected by the operator, the smaller the scan volume or FOV the better the resolution; thus, endodontic scans should be done with the smallest reasonable FOV.
FOV
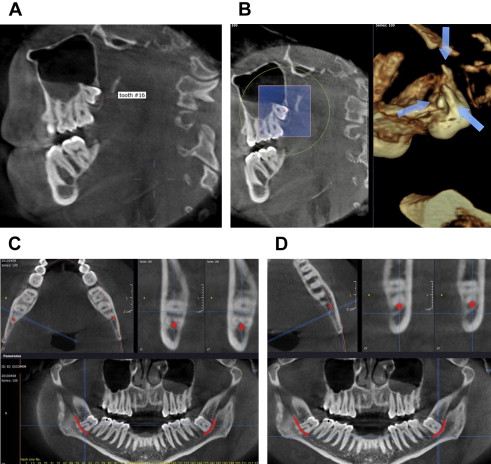
An important consideration for a scan is what to include within the FOV. On the one hand, one wants to keep the FOV as small as possible, both to reduce patient x-ray dose and to improve spatial resolution in the images. On the other hand, the FOV should include a sufficient view of the anatomic area so that one acquires the necessary information. Examples of scans that are underinclusive and overinclusive are common. Fig. 4 is a sagittal slice of a scan that was done for the purpose of planning mandibular implants. Clearly, anything below the inferior cortex of the mandible and 2 to 3 mm superior to the occlusal plane is superfluous. The potential liability issue that arises is that the dentist is responsible for reading the entire scan. Thus, even though the maxilla and skull were not required in this case, once they are included in the scan, the dentist is responsible for pathology missed in either location.
Too small an FOV carries its own risk. This is seen most commonly in the maxilla. Fig. 5 A shows a large FOV CBCT scan performed for maxillary implant planning purposes. The panoramic reconstruction shows a large mucous retention cyst in the right maxillary sinus. The diagnosis can be made from the dome-shaped superior aspect of the lesion. Blood, exudates, transudates, thickened mucosa, and other soft tissue in the sinus have a similar opacity on CBCT scans. Thus, one must rely on the shape and distribution of the lesions to differentiate between them. Importantly, when it comes to the shape, it is the superior aspect of the lesion (eg, dome-shaped, straight, meniscus) that is significant and that allows one to distinguish among the various conditions. It follows then that to be able to make this differentiation, one must image the entire sinus, up to the orbital floor, as lesions may fill the entire or almost the entire sinus. If a dentist takes a small FOV scan and sees pathology in the maxillary sinus, but is unable to visualize the superior border of the pathology, then the dentist is obligated to obtain a second scan that includes the entire sinus. This is necessary for 2 reasons. First, the clinician will be not be able to ascertain from the small FOV scan whether the pathology is impinging on the ostium or may do so after surgery such as a sinus augmentation. Second, the clinician will not be able to identify the nature of the pathology.
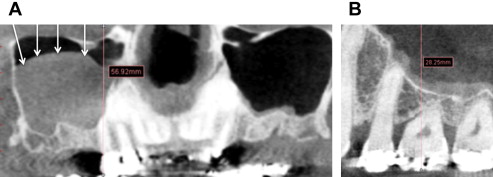
Fig. 5 B shows a small FOV scan in a different patient from that in Fig. 5 A. Assume that the same size mucous retention cyst was present in the patient on whom the small FOV scan was taken. From the images, it is readily evident that the superior aspect of the mucous retention cyst would not have been visible on the small FOV scan. In this case, one would have needed to take a second scan, this time a large FOV scan. For this reason, although small FOV scans are adequate when planning mandibular implants, a larger FOV that encompasses the entire maxillary sinus is preferable in the maxilla.
This principle is based on the fact that sinus pathology is common even in asymptomatic patients. The symptoms of sinusitis may be “subclinical” and manifest only at the next insult, such as an allergen or common rhinovirus. The prevalence of pathologic findings on CBCT scans of asymptomatic patients has been reported to vary from 24.6% to 56.3%. Pette and colleagues reported sinus pathology in 61.95% of patients on whom a CBCT scan had been done for implant planning purposes, although Rege and colleagues reported findings in 68.2% of cases of asymptomatic patients. A large FOV does not imply that both sides should be included in a scan, as is seen in Fig. 5 A. If surgery is going to be undertaken on only one side, and the CBCT machine allows for imaging only one side while including the entire sinus, then that is preferable.
It is generally true that dentists prefer small FOV scans because they believe that it is not unlike a periapical scan in size and scope and that they are therefore able to read it themselves. This, they believe, limits their liability by excluding anatomy that they are not comfortable interpreting. Although small FOV scans are preferable because they reduce patient dose and improve spatial resolution, the motivation for selecting a small FOV should not be to limit a dentist’s liability. Further, serious pathology may present even on small FOV scans. Fig. 6 shows a cropped axial image of a small FOV scan undertaken for endodontic purposes. The image raised the possibility of a malignant lesion, which was later confirmed on biopsy.