The paranasal sinuses are 4 paired airspaces that border the nasal cavity. Dental professionals are most familiar with the maxillary sinuses as viewed in 2-D imaging (eg, periapical, panoramic projections). With increasing implementation of 3-D imaging, specifically cone beam CT, there is a high probability that much or all of the paranasal sinuses and nasal cavity will be captured in a scan. It is incumbent on practitioners to be familiar with all the structures contained within a scanned area. The purpose of this article is to provide an overview of the anatomy of the nasal cavity as well as common anatomic variants and pathologic entities.
Key points
- •
The paranasal sinuses are 4 paired airspaces that border the nasal cavity. The functions of the nasal cavity and paranasal sinuses include decreasing the weight of the skull, heating and humidifying inspired air, resonance in speech, regulation of intranasal pressure, and increasing surface area for olfaction.
- •
The paranasal sinuses have also been described as crumple zones or areas that absorb the energy from trauma and protect vital structures in the skull.
- •
Dental professionals are most familiar with the maxillary sinuses as viewed 2-D imaging (eg, periapical, panoramic projections). With the increasing implementation of 3-D imaging, however, specifically cone beam computed tomography (CBCT), there is a high probability that much or all of the paranasal sinuses and nasal cavity are captured in a scan.
Nasal cavity
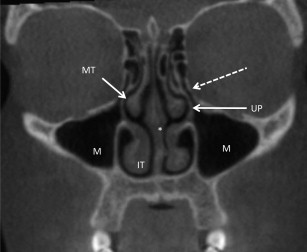
The nasal cavity is bounded inferiorly by the hard palate, laterally by the medial walls of the right and left maxillary sinus, and superiorly by the nasal, ethmoid, and sphenoid bones. The primary components of the lateral walls of the nasal cavity are the inferior middle and superior conchae (also termed, turbinates ). These structures protrude into the nasal cavity and act as baffles to help warm/cool, filter, and humidify inspired air. Another function of the nasal cavity is the sense of smell. The spaces between the conchae are referred to as meatuses . The inferior meatus is located beneath the inferior concha and is the site for drainage of the nasolacrimal duct. The middle meatus is the site of drainage for the frontal, anterior ethmoid, and maxillary sinuses. There is also a communication from the middle meatus to the maxillary sinus through an opening, called the ostium . The superior meatus communicates with the posterior ethmoid and sphenoid sinuses through the sphenoethmoidal recess ( Fig. 1 ). The nasal cavity is divided by the nasal septum. The anterior portion of the nasal septum is composed of cartilage. The posterior nasal septum is bony. The arterial blood supply for the nasal cavity comes from internal maxillary artery (branch of external carotid artery) and the anterior and posterior ethmoidal arteries (branches of the internal carotid artery). The vascularity of the nasal cavity accounts for the volume and intensity of bleeding when the region is injured. The nasal cavity is innervated by the olfactory (CN I), ophthalmic, and maxillary branches of the trigeminal (CN V) and facial (CN VII) nerves.
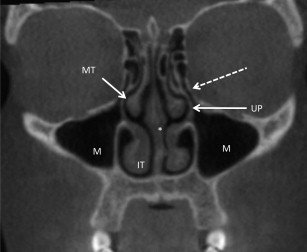
Nasal cavity
The nasal cavity is bounded inferiorly by the hard palate, laterally by the medial walls of the right and left maxillary sinus, and superiorly by the nasal, ethmoid, and sphenoid bones. The primary components of the lateral walls of the nasal cavity are the inferior middle and superior conchae (also termed, turbinates ). These structures protrude into the nasal cavity and act as baffles to help warm/cool, filter, and humidify inspired air. Another function of the nasal cavity is the sense of smell. The spaces between the conchae are referred to as meatuses . The inferior meatus is located beneath the inferior concha and is the site for drainage of the nasolacrimal duct. The middle meatus is the site of drainage for the frontal, anterior ethmoid, and maxillary sinuses. There is also a communication from the middle meatus to the maxillary sinus through an opening, called the ostium . The superior meatus communicates with the posterior ethmoid and sphenoid sinuses through the sphenoethmoidal recess ( Fig. 1 ). The nasal cavity is divided by the nasal septum. The anterior portion of the nasal septum is composed of cartilage. The posterior nasal septum is bony. The arterial blood supply for the nasal cavity comes from internal maxillary artery (branch of external carotid artery) and the anterior and posterior ethmoidal arteries (branches of the internal carotid artery). The vascularity of the nasal cavity accounts for the volume and intensity of bleeding when the region is injured. The nasal cavity is innervated by the olfactory (CN I), ophthalmic, and maxillary branches of the trigeminal (CN V) and facial (CN VII) nerves.
Anatomic variants—nasal cavity
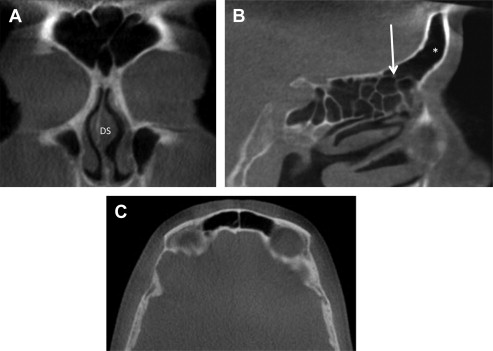
Deviated Nasal Septum
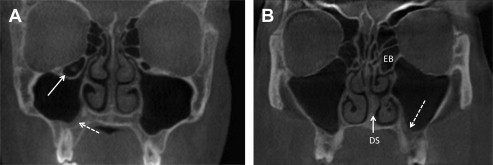
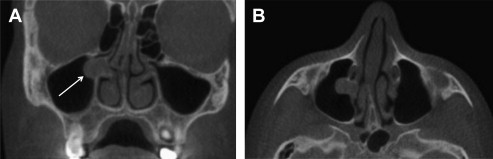
The deviated nasal septum is a common finding within the nasal cavity and occurs when the nasal septum is displaced toward one side of the nasal cavity. Deviated nasal septum may be congenital or due to trauma. The deviation may be mild with no symptoms or sequelae. When a deviation is severe, however, the flow of air through the nasal cavity is redirected and may manifest as nasal obstruction, noisy breathing during sleep, and/or epistaxis. Severe deviations can result in hypoplasia of the ipsilateral turbinates and/or hyperplasia of the contralateral turbinates ( Fig. 2 ). The nasal septum may also exhibit pneumatization. This is of little clinical significance unless it obstructs nasal airflow or surgical access to the paranasal sinuses.
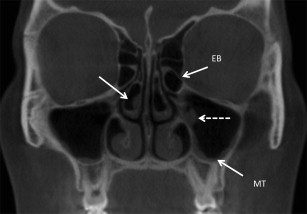
Concha Bullosa
Concha bullosa or pneumatization of the concha is seen in from 14% to 53.6% of the population ( Fig. 3 ). Concha bullosa are grouped according to the location of the pneumatization and are classified as lamellar, bulbous, or extensive. Concha bullosa are most commonly seen in the middle turbinate and may be unilateral or bilateral. Unilateral concha bullosa are frequently associated with a deviated nasal septum. A vast majority of concha bullosa are asymptomatic. There is ongoing debate regarding the association of concha bullosa with sinus disease, with the current view that concha bullosa are associated with sinus disease when they block or impinge on the ostiomeatal complex.
Paradoxic Turbinate
Paradoxic curvature of the middle turbinate refers to a convex curvature on the lateral, rather than medial side of the turbinate, and is seen in 4% to 27% of the population. Paradoxic turbinates may predispose patients to unilateral sinusitis if they block the middle meatus.
Paranasal sinuses
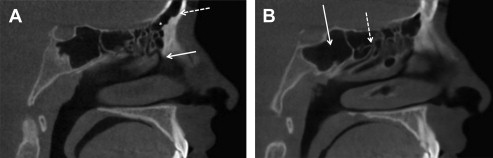
Frontal Sinus
The frontal sinuses are located within the frontal bone on either side of the midline superior to the orbits. The floor of the fontal sinus is bordered by the orbital portion of the frontal bone. The posterior wall separates the dura of the frontal lobe from the lining mucosa. The frontal sinuses extend to the most anterior aspect of the middle meatus and drain through the nasofrontal duct, which can, in turn, drain into either the frontal recess or ethmoid infundibulum ( Fig. 4 ). The ostia of the frontal sinuses are positioned approximately two-thirds up the posterior medial walls. This positioning makes complete clearing of the sinus after infection difficult. The middle meatal branch of the sphenopalatine and anterior ethmoid arteries provide the arterial supply to the frontal sinuses. The venous drainage of the frontal sinuses is through valveless transosseous channels that communicate with both the orbit and cranial vault. Branches of V1 and V2 innervate the frontal sinus mucosa. The frontal sinuses are usually paired but are often asymmetric and exhibit the greatest amount of developmental variation. These variations range from complete agenesis to pneumatization of the frontal bone.
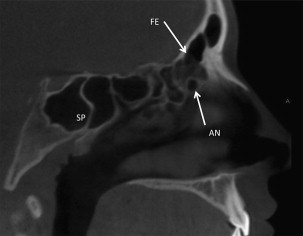
Ethmoid Sinuses (Ethmoid Air Cells)
The ethmoid sinuses, or ethmoid labyrinth, are contained within the ethmoid bone. The ethmoid sinus is divided into anterior and posterior components due to the separate drainage of these components. The anterior ethmoid sinus drains into the middle meatus. The posterior ethmoids drain into the sphenoethmoidal recess ( Fig. 5 ). The lateral borders are the lamina papyracea of the orbit. The medial border of the anterior ethmoid sinuses is the middle turbinate. The medial border of the posterior ethmoid sinuses is the superior turbinate. The roof of the ethmoid sinuses is called the fovea ethmoidalis . The ethmoid roof is immediately adjacent to the cribriform plate and is often the point of entry of the anterior cranial fossa during endoscopic surgery. The anterior ethmoid sinuses are supplied by the sphenopalatine and anterior ethmoid arteries. The posterior ethmoid sinus is supplied by the superior conchal branch of the sphenopalatine artery and the posterior ethmoid artery. The posterior ethmoid sinus is innervated by the superior nasal branches of V2 and anterior ethmoid branch of V1.
There are several ethmoid air cells that serve as anatomic markers. The largest and most prominent air cell in the anterior ethmoid sinus is referred to as the ethmoid bulla. The agger nasi cells are the most anterior of the anterior ethmoid air cells and are found anterior and superior to the middle turbinate. The agger nasi cell is the landmark through which the frontoethmoidal recess is entered during endoscopic surgery. Haller cells are found along the inferior border of the orbits. The Haller cells can be of clinical significance if they enlarge to the point where they impinge on the ethmoid infundibulum. The Onodi cells are derived from the posterior ethmoids and represent pneumatization of air cells lateral and superior to the sphenoid sinus.
The Ostiomeatal Complex
The ostiomeatal complex is not a discrete anatomic entity. Ostiomeatal complex refers to a collection of middle meatal structures and consists of the uncinate process, ethmoid infundibulum, and anterior ethmoid cells. It also represents the final common pathway of drainage for the frontal, anterior ethmoid, and maxillary sinuses. The uncinate process is a sickle or hook-shaped bone of the lateral nasal wall. Anteriorly, the uncinate process attaches to the lacrimal bone; inferiorly, the uncinate process attaches to the ethmoidal process of the inferior turbinate. The posterior margin sits in the hiatus semilunaris inferioris. Superiorly, the uncinate process may attach to the middle turbinate, lamina papyracea, and/or the skull base. The ethmoid infundibulum is a space bordered laterally by the bony orbit and medially by the uncinate process. The maxillary sinus drains into this space.
Sphenoid Sinus
The sphenoid sinus is found in the sphenoid bone. The pituitary fossa sits superior to the sinus along with the olfactory nerves and optic chiasm. The pterygoid canal often courses beneath the mucosa along the floor of the sinus. The cavernous portion of the internal carotid artery runs along the lateral wall of the sphenoid sinus. The ostium of the sphenoid sinus is positioned in the center of the anterior wall of the sinus toward the superior aspect of the sinus. The sphenoid sinus drains into the sphenoethmoidal recess ( Fig. 6 ). Branches of the sphenopalatine and nasopalatine arteries provide the arterial blood supply of the sphenoid sinus. The sphenoid sinus is innervated by the posterior ethmoid branch of V1 and the posterior superior nasal branches of V2.
Pneumatization is a common anatomic variant of the sphenoid sinus. Pneumatization can occur in the lateral or superior direction and involve the greater and lesser winds of the sphenoid bone as well as the pterygoid processes and anterior clinoid process. This pneumatization increases the size of the air space but more importantly thins the bone and, given the proximity of numerous vital structures, can increase the risk of surgical misadventures ( Fig. 12 ). Onodi cells from the posterior ethmoids can also extend superior and lateral to the sphenoid sinus further thinning the bone.
Maxillary Sinus
The maxillary sinuses are the largest of the paranasal sinuses and the most familiar to dental professionals. The maxillary sinus is viewed in images that are used daily (eg, periapical, panoramic projections). The maxillary sinuses are contained within the maxilla. The roof of the maxillary sinus is the orbital floor. The infraorbital canal traverses the roof of the maxillary sinus. The floor of the maxillary sinuses closely approximates the roots of the posterior maxillary teeth. The ostium of the maxillary sinus is located in the medial wall and drains into the ethmoid infundibulum ( Fig. 7 ). The nasolacrimal ducts pass adjacent to the maxillary sinuses and drain into the inferior meatus. The ethmoid arteries and middle meatal branch of the sphenopalatine artery provide the arterial blood supply for the maxillary sinus. The maxillary sinus is innervated by branches of the infraorbital and branches of the posterior superior nasal nerves. Anatomic variants of the maxillary sinuses include pneumatization, septations, and accessory ostia.
Pathology
Nasal Obstruction
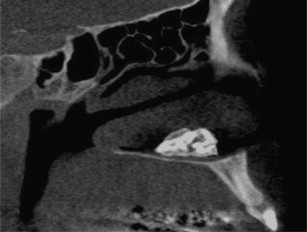
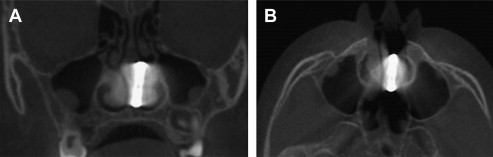
The most common form of nasal obstruction is hyperplasia of the turbinates. This can be caused by chronic inflammation and infection. Many times, nasal obstructions can, in turn, obstruct the flow of air into the paranasal sinuses. Other causes of nasal obstruction are nasal polyps; antrochoanal polyps; benign tumors, such as osteoma, papilloma, or angiofibroma; rhinoliths ( Fig. 8 ); foreign bodies ( Fig. 9 ); and malignant tumors (most commonly squamous cell carcinoma). Rhinoliths are calcifications of endogenous materials, such as pus, epithelial cells, or bone or exogenous materials–foreign bodies. The long-standing presence of either rhinoliths or foreign bodies can cause ipsilateral hypoplasia of the turbinates.
Hyperplastic Turbinates
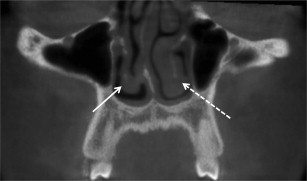
Hyperplastic turbinates are thought to be the result of chronic inflammatory conditions, such as allergic rhinitis. The increase in turbinate size may be due to either soft tissue or bony enlargement. Hyperplastic turbinates are of clinical significance when they impinge on airflow through the nasal cavity and into the paranasal sinuses ( Fig. 10 ).
Nasal Polyps
Nasal polyps are aggregates of soft tissue that arise within the nasal cavity. The tissue enlargement is not neoplastic but is most likely the result of chronic inflammation/infection of the nasal mucosa. When nasal polyps are small they have minimal clinical significance. Large polyps can produce obstruction of the nasal airway and block sinus ostia. The radiographic appearance of a nasal polyp is a homogeneous relative radiopacity that arises in an air space. Polyps can also appear in the maxillary sinuses ( Fig. 11 ).

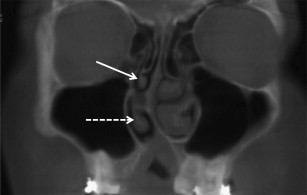
Antrochoanal Polyps
Antrochoanal polyps arise in the maxillary sinus and extrude through the ostiomeatal complex into the nasal cavity. Antrochoanal polyps have a similar radiographic appearance as nasal polyps. The extension from the maxillary sinus differentiates the antrochoanal polyp from the nasal polyp (see Fig. 12 ). Antrochoanal polyps are more commonly seen in children and are usually unilateral. Obstruction of the maxillary ostium is the most common complication of the antrochoanal polyp.
Papilloma
Papillomas can arise from the epithelium within the nasal cavity and are considered true neoplasms. The radiographic appearance of a nasal papilloma is a unilateral, irregularly shaped relative radiopacity. A subtype of nasal papilloma is termed, inverted papilloma . The inverted descriptor refers to the histopathology rather than the clinical or radiographic presentation. A small percentage of these inverted polyps can undergo malignant transformation into squamous cell carcinoma. In addition to the soft tissue radiopacity, these entities may cause some bony resorption as they enlarge. An infrequent finding is hyperostosis of the bone adjacent to the base of the inverted papilla.
Juvenile Nasal Angiofibroma
The juvenile nasal angiofibroma (JNA) is a tumor of fibrous connective tissue with a propensity for brisk bleeding. JNA is seen almost exclusively in males in the second decade. JNA presents as a fast-growing soft tissue mass that originates from the area of the posterior aspect of the middle turbinate. JNA can produce bony destruction. One of the classic radiographic findings is bowing of the posterior bony wall of the maxillary sinus.
Cleft Palate
Palatal clefts can extend into the nasal cavity and appear as discontinuities of the nasal floor. Additionally, the morphology of the nose and the nasal cavity can be altered due to the palatal cleft. Deviated nasal septum and nasal asymmetry are commonly seen with cleft palate ( Fig. 13 ).