Virtual, or computer-aided, surgery is a process that integrates computer-aided design (CAD) and computer-aided manufacturing (CAM) into surgical treatment planning by providing a means to (1) visualize and analyze 3-dimensional (3D) images of soft tissue and skeletal anatomy, (2) perform virtual manipulations (surgery) to idealize skeletal relationships or plan soft or hard tissue operations, and (3) transfer the virtual plan to patients at the time of surgery. The conventional computed tomography (CT) scan is imported into a proprietary software program, which allows 3D analysis of a defect or deformity. This abnormal region can then be altered by mirror imaging, segmentation, and insertion to create idealized skeletal proportions. Using a CAD/CAM process, a planning model, occlusal stent, cutting guide, or custom implant can be constructed based on the idealized virtual image, which is then translated to the patients. Computer-assisted surgery is particularly useful for achieving optimal functional and esthetic results in patients with complex craniomaxillofacial deformities.
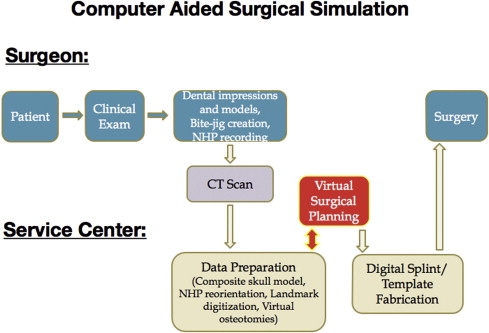
Xia and Gateno and colleagues have described a computer-aided surgical simulation (CASS) for use in treatment planning for complex cranio-maxillofacial deformities. A series of recent investigations performed at multiple institutions have confirmed the accuracy of the CASS, which is rapidly becoming state of the art for 2-jaw orthognathic surgery. As clinical experience with the use of CASS becomes more wide spread, it will have the potential to completely replace analytical model surgery with stone casts as the optimal method of treatment planning and implementing complex orthognathic surgery.
Most commercially available software systems are complex and too time consuming for a busy surgeon. Therefore, the senior author has used a third-party service provider to facilitate software manipulation and splint construction (Medical Modeling Inc, Golden, CO, USA). Various orthognathic software planning programs are available and others are currently in development, although SimPlant OMS (Materialise Dental NV, Leuven, Belgium) has been used by the authors for the last 3 years and provided predictable results. This article provides a step-by-step outline of CASS for orthognathic surgery procedures, with and without concomitant temporomandibular joint (TMJ) replacement.
Computer-aided surgical simulation
Virtual surgery generally consists of 4 phases:
- 1.
Data acquisition phase: clinical examination with bite registrations and anthropometric measurements; radiographic examination/CT scan
- 2.
Planning phase: importation of 3D CT data into proprietary planning software
- 3.
Surgical phase: translation of the virtual surgical plan to patients using stereolithographic models, cutting guide stents, occlusal splints, or intraoperative navigation
- 4.
Assessment phase: evaluation of the accuracy of virtual surgical plan transfer using intraoperative or postoperative CT imaging.
The first step of the CASS process is to create a composite skull model. This step is accomplished with a bite jig that is used to relate the upper and lower dental casts to each other and to support a set of fiducial markers. The fiducial markers, or reference points, are then used to register the digital dental models to the 3D CT skull model. After the bite jig is created, a CT of the patients’ craniofacial skeleton is obtained with the patients biting on the bite jig. Digital dental models are then created by scanning the plaster dental models with a laser surface scanner. Using the fiducial markers, the digital dental models are integrated into the CT data through superimposition. The result is a computerized composite skull model with an accurate rendition of the bone and teeth. The second step of the CASS is to quantify the deformity with cephalometric analyses and virtual anthropometric measurements. The third step in the process is to simulate the surgery in the computer, moving the bony segments to the desired position. Using this software, the maxilla and mandible can be repositioned in all 3 planes of space. Hence, deformities of yaw, pitch, and roll can be accurately corrected in a virtual environment. The final step is to transfer the virtual plan to the patients through surgical splints and templates that are created using a specialized CAD/CAM technique ( Fig. 1 ).
Data acquisition phase
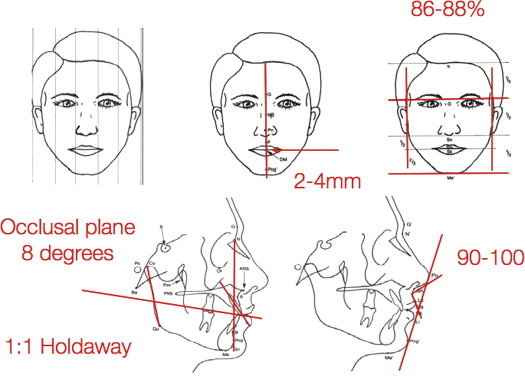
Precise preoperative data acquisition for orthognathic surgery planning is of paramount importance to achieve optimal clinical outcomes. A thorough clinical examination that details the facial symmetry, lip-to-tooth ratio, anterior two-thirds face height to bizygomatic width, nasolabial angle and nasal projection, as well as occlusal information, such as overjet, overbite, and maxillary and dental midline position relative to each other and to the facial and chin midlines, is performed. Conventional cephalometric data measurements are also useful in treatment planning, particularly the angulation of the occlusal plane, the posterior face height/ramus length, the incisor angulation, and the holdaway ratio ( Fig. 2 ).
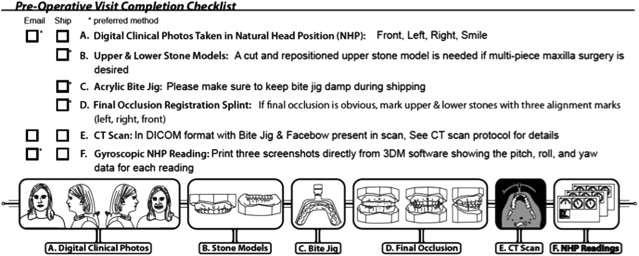
The data that must be collected for computer-planned cases are summarized in Fig. 3 and include the following: (1) anthropometric measurements; (2) a centric relation registration, which should be obtained before CT imaging using polyvinyl siloxane in a prefabricated bite jig ( Fig. 4 ); (3) digital clinical photographs taken in the natural head position (NHP); (4) upper and lower stone dental models, which should be segmentalized if segmental maxillary surgery is to be performed. Although the Le Fort osteotomy is segmentalized in the software, the final occlusion cannot be accurately predicted without tactile clinical information. Therefore, stone models are still required for accurate final occlusion. The segmental cuts are then mimicked in the software based on the models; (5) a final occlusion registration splint using stone models; (6) an orientation sensor NHP reading using 3DM (Micro Strain Inc, Williston, VT, USA) software, generating a numerical value for pitch, roll, and yaw ( Fig. 5 ); (7) a CT/cone-beam CT (CBCT) scan, in Digital Imaging and Communications in Medicine (DICOM) format, with the bite jig present in the scan. The CT scan is obtained with a specific format using a matrix of 512 × 512 at a 0.625-mm slice thickness, 25 cm or lesser field of view (FOV), 0° gantry tilt, and 1:1 pitch. If using CBCT, it is recommended that the longest available scan time, a setting of 0.3 to 0.5 voxels, and the largest FOV be used. The CT images are then transferred to the appropriate surgical planning software in DICOM format.
Data acquisition phase
Precise preoperative data acquisition for orthognathic surgery planning is of paramount importance to achieve optimal clinical outcomes. A thorough clinical examination that details the facial symmetry, lip-to-tooth ratio, anterior two-thirds face height to bizygomatic width, nasolabial angle and nasal projection, as well as occlusal information, such as overjet, overbite, and maxillary and dental midline position relative to each other and to the facial and chin midlines, is performed. Conventional cephalometric data measurements are also useful in treatment planning, particularly the angulation of the occlusal plane, the posterior face height/ramus length, the incisor angulation, and the holdaway ratio ( Fig. 2 ).




