The surgeon is confronted with the following options when faced with a protruding premaxilla at birth:
1.
Uniting the lip over the protruding premaxilla and considering later surgical setback and other surgical options
2.
External elastics attached to a head bonnet or elastic tape to the cheeks to ventroflex the premaxilla
3.
Early surgical premaxillary setback
4.
Complete removal (excision of the premaxilla)
5.
Early mechanical retrusion prior to lip surgery or presurgical orthopedic treatment (PSOT) without retraction and with or without primary bone grafting or periosteoplasty
6.
Lip adhesion followed by definitive lip surgery at a later age
7.1 Premaxillary Protrusion: Real or Apparent? Is the Palate Deficient in Bone?
A bilateral cleft of the lip and palate can be complete or incomplete on one or both sides (see Chap. 4). Any number of variations can exist. In both incomplete and complete bilateral clefts of the lip and alveolus, the size and shape of the premaxilla are dependent on the number of tooth buds and their distribution, making it symmetrical or asymmetrical (Fig. 7.1). Because clefts of the lip/alveolus and the hard and soft palate come from different embryological sources, the cleft may involve the lip and alveolus with or without involving the hard and soft palate.


Fig. 7.1
(a) Small premaxilla: three deciduous incisors with one unerupted permanent central incisor. (b) Large premaxilla: four deciduous incisors with two permanent unerupted incisors. (c) Occlusal radiographs of premaxillae showing variations in the number of anterior deciduous teeth and permanent tooth buds. (d) Occlusal radiographs of premaxillae showing variations in the number of anterior deciduous teeth and permanent tooth buds
Based on the observations of Veau and Borel (1931), Veau (1934) and Browne (1969) and the later work of Friede and Pruzansky (1972), Bergland and Borchgrevink (1974), Harvold (1954), Berkowitz (1959), Friede (1977, 1978), Atherton (1967, 1974), and Handelman and Pruzansky (1968), the cause of premaxillary protrusion is the result of tension and the resulting bony overgrowth produced at the premaxillary-vomerine suture (PVS) by displacement of that bone by the aberrant muscular forces of the detached outer musculature combined with the pushing force of the tongue fitting within the cleft (Fig. 7.2). These investigators, using cephalometric data, concluded that the premaxilla is postured forward in the facial profile at birth (Fig. 7.3).


Fig. 7.2
(a) Line drawing of a complete bilateral cleft lip and palate with an arrow pointing to the premaxillary-vomerine suture (PVS) (b) A small protruding premaxilla IBCLP extends forward of the facial profile and lateral palatal segments. (c) Variations in bilateral cleft lip and palate. The size of the premaxilla varies with the number of teeth it contains. Classification is dependent on the completeness of clefting of the lip and alveolus and whether there is a cleft of the hard and soft palate. Yet one or both sides of the hard palate may or may not be attached to the vomer. If it is attached to the vomer, it is classified as being incomplete. Even in complete clefts of the lip and alveolus, the extent of premaxillary protrusion will vary. (a) Incomplete bilateral cleft lip and palate. Complete cleft lip and palate – left side. Incomplete cleft lip and palate – right side. (b) Complete bilateral cleft lip and palate. Complete cleft palate – both sides. (c) Incomplete bilateral cleft lip and palate. Incomplete palatal clefts – both sides. (d) Complete bilateral cleft lip and palate. Incomplete right and complete left palate. (e) Incomplete bilateral cleft lip and palate. Incomplete left palate and complete right palate. (f) Complete bilateral cleft of the lip and palate. Incomplete right and left palatal segments (g) Complete bilateral cleft of lip and palate. Incomplete left palate and complete right palatal segment. (h) Complete bilateral cleft lip and palate. Incomplete left palate and complete right palate. (i) Incomplete bilateral cleft lip and alveolus. Normal palate
Fig. 7.3
Two-stage lip closure in a CBCLP. Ten months after lip closure, the angle of facial convexity changed from 108° to 142° as a result of the ventroflexion of the premaxilla at the premaxillary-vomerine suture (PVS) coupled with some additional mandibular growth. A two-stage lip closure is rarely necessary (Courtesy of S Pruzansky)
Bergland and Borchgrevink (1974) reported that, in complete bilateral clefts of the lip and alveolus with intact palates, the premaxilla was protrusive but palatal size was well within normal limits. In these cases, the septum was detached from the normally developed palates and the protrusion of the premaxilla was interpreted as representing a premature release of the normal growth potential of the septum. The premaxilla apparently reached its geometric position within the skull at an earlier time prior to birth, yet the palatal segments followed a normal growth rate. Berkowitz’s clinical records support the findings of Coup and Subtelny (1960), who reported marked palatal hypoplasia in bilateral clefts of the lip and palate. Berkowitz reports in this book that palatal growth rates are highly variable according to the amount of scarring created when closing the cleft space.
7.2 The Premaxillary-Vomerine Suture
Pruzansky (1953, 1971) and Friede and Morgan (1976) used metal implants on either side of the premaxillary-vomerine junction to demonstrate cephalometrically that this suture was a major site of bony overgrowth (Fig. 7.4). Earlier, Berkowitz (1959) and later Pruzansky (1971), Friede and Morgan (1976), Pruzansky and Friede (1975), Friede (1973), Vargervik (1983), and Berkowitz (1959) suggested that the overgrowth was probably a secondary reaction to the lack of restraint from the cleft orbicularis oris muscle. They showed that midfacial growth continued for 1–3 years even after the lip was united but at a slower rate. Berkowitz (1959) serial cephalometric tracings and digital cast study demonstrated that the midface continued to protrude for 2–3 years after the lip was united, then its forward growth slowed markedly (Fig. 7.5). Not surprisingly, in some instances, the facial convexity did not change due to the continued forward growth of the maxilla and premaxilla but was due to more vertical rather than forward growth of the mandible, maintaining the facial convexity (Figs. 7.6 and 7.7).
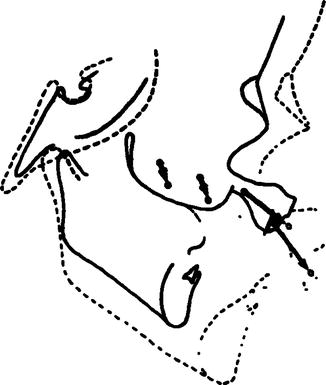
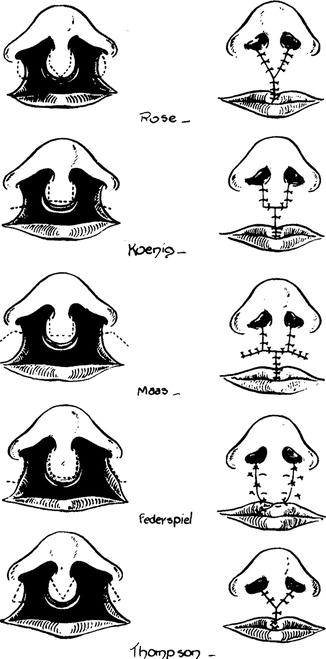
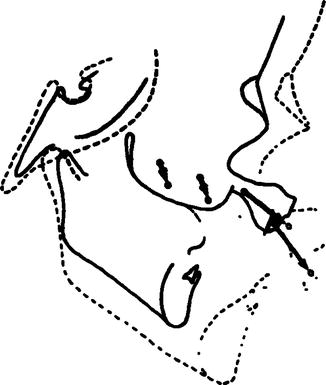
Fig. 7.4
To test growth at the premaxillar-vomerine suture (PVS) in complete bilateral cleft of the lip and palate, two pairs of metal pellets were placed on either side of the PVS at 6 months of age. At 3 years, 5 months of age, the distance between the anterior and posterior sets of pellets had increased with the growth at PVS. Note that there was no change in distance within each set of metal pellets (Courtesy of S Pruzansky)
Fig. 7.5
(a–f) A method used to show serial changes in facial growth and development in CBCLP using sella for registration while superimposing on the anterior cranial base. Facial angles and landmarks (upper left): nasion (N), pogonion (Po), gonion (Go), sella (S), alpha (a) most anterior point on the premaxilla, menton (Me), constructed Frankfort horizontal (FHc), anterior point of the lateral palatal processes (M), pterygomaxillary fissure (Ptm). Facial polygon (upper middle) drawn connecting landmarks S-N-a-Po-Me-Go-S. Landmark points (upper right) projected to a constructed Frankfort horizontal line which is drawn 6° from the anterior cranial base (SN) at S. (b) An example of excellent facial growth. The cultural standard for a good aesthetic Caucasian face is a “flat” face, having an angle of facial convexity of approximately 180°. Most newborn noncleft faces have a relatively acute facial profile associated with relative retrognathia which usually flattens with growth (d) Serial lateral cephalometric tracings showing changes in the angle of facial convexity (NaPo) from 113° to 154° in 8 11/42 years. (e) Facial polygon of the case shown in Fig. 7.5d. Each polygon showing profile changes is superimposed on SN and registered at Sella. The midfacial protrusion at a had not increased after 2 years, whereas both the anterior cranial base (SN) and mandible had increased in size. The mandible grew forward and downward, flattening the facial profile. The timing of these growth changes is variable (f) Projection of landmark points to the constructed Frankfort horizontal line drawn 6° from SN at S. This growth projection system also shows that the midfacial protrusion did not increase after 2 years, whereas the forward projection of the mandibular body increased markedly until 8 11/42 years of age. These are the main factors leading to the flattening of the facial profile. Good facial growth changes can occur early or late (From Millard 1980)
Fig. 7.6
(a, b) An example of “poor” profile growth changes. This evaluation is made when the acute facial profile seen at birth remains the same or worsens with time. (a) Serial cephalometric tracings showing poor facial growth leading to premaxillary excision. The acute angle of facial convexity remained the same after 2 years. This treatment plan should be abandoned at any age even with severe midfacial protrusion. In similar growing faces, some clinicians believe premaxillary surgical setback is preferable for psychosocial reasons prior to starting elementary school. (b) Superimposed polygons of case show a mandible that is growing vertically with very few horizontal growth increments. The premaxilla continued to grow forward although there was no forward growth between 3–0–14 and 4–2–0. Note the placement of the lower lip lingual to the premaxilla. The premaxilla was excised at 4–9. This case came from Pruzansky’s records (From Berkowitz 1959)
Fig. 7.7
The first 2 years of maxillary and mandibular tracings of the cases with good (see Fig. 7.5) and bad (see Fig. 7.6) facial growth are compared to show the reasons for these evaluations. CP-72: Good facial growth. In this case, the degree of premaxillary protrusion relative to the lateral palatal segments (the anterior cleft space) was markedly reduced with growth. Premaxillary protrusion relative to the anterior cranial base was reduced as well. CP-139: Poor facial growth. The degree of premaxillary protrusion relative to the lateral palatal segments remained the same, while the premaxillary protrusion relative to the anterior cranial base increased (Courtesy of S. Pruzansky). Comments: Although mandibular growth in the two cases was similar in degree, the superimposed polygons show that the vertical direction of growth of the “bad” grower’s mandible and not its size was the determining factor for the changes in the angle of facial convexity (NaPo). Tension at PVS created by the lower lip positioned lingual to the premaxilla increased premaxillary growth
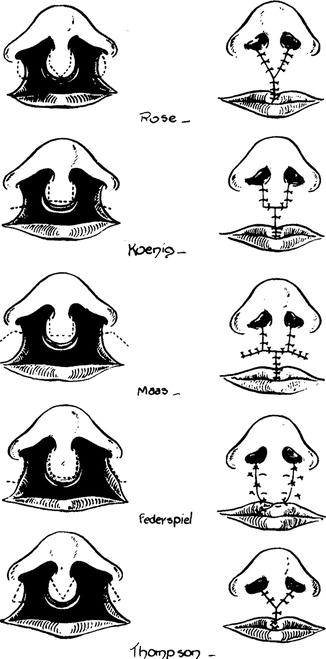
Fig. 7.8
Various surgical techniques used to unite the lip in BCLP. Experience has shown that the best results are obtained when the prolabium is used to construct the entire midportion of the lip (From Millard 1980)
Pruzansky (1953, 1971), Friede (1973), and Atherton (1967, 1974) described the premaxillary-vomerine suture as resembling other facial sutures. Friede and Morgan (1976) confirmed the presence of small islands of cartilage in the suture; these were secondary occurrences resulting from mechanical stresses and not part of a force system causing growth.
Burston (1960, 1967) and Latham (1969, 1973) following Scott (Scott 1956a, b) “Nasal Septum Growth” thesis, believe that the displacement is not real but only apparent. Burston thought that the lateral segments of the maxilla were retroplaced and considered the premaxilla to be in normal position. Latham suggested that a contributing factor in producing the projecting premaxilla was the shortening of the septomaxillary ligament which drew it forward.
Pruzansky and Friede (1975) roentgencephalometric data confirmed the existence of a true, rather than a relative, premaxillary protrusion. Metallic implants were inserted on either side of the PVS at the time of initial surgery and were followed up roentgencephalometrically. Although continuous growth was recorded in the PVS, there was a postsurgical decrease in the premaxillary protrusion. On the basis of both histology and cephalometrics, Friede (1973) concluded that traumatic surgery involving the PVS would be likely to contribute to the impaired midfacial growth. This has been verified by Berkowitz’s more recent follow-up studies of the effects of mechanical premaxillary retraction on profile development. He has observed similar midfacial problems of impaired growth (see Chap. 21).
Berkowitz speculated that severe pressure at the PVS would cause a hemorrhage followed by fibrosis and synostosis with cellular destruction, both acting to inhibit sutural growth. In contrast, a united lip across the protruding premaxilla exerts a more tolerant retrusive force within the PVS, acting well within its physiologic threshold level for slowing down bone growth but not totally inhibiting it.
Based on conclusions drawn from his clinical findings and those of Pruzansky and Friede (1975) research, Berkowitz rejects Latham (1969, 1973) “force of the cartilaginous septum via the septo-premaxillary ligament” as the cause of premaxillary protrusion. Enlow (1982) description of the nasomaxillary complex’s growth is worth repeating:
The nasomaxillary complex is in contact with the floor of the cranium. The whole maxillary region in total is displaced downward and forward away from the cranium by the expansive growth of the soft tissues in the midfacial region. This then triggers new bone growth at the various sutural contact surfaces between the nasomaxillary composite and the cranial floor. Displacement thus proceeds downward and forward as growth by bone deposition simultaneously takes place in an opposite upward and backward direction.
McNeil (1950) mistakenly had stated that the detached palatal segments from the nasal septum are not only reduced in mass but also are not brought forward with the developing nasal septum.
This failure of the palatal segments to move forward with growth would lead to a retrusive midface with a Class III malocclusion (he did not want to blame the suggestions).
7.3 Facial Growth Studies Show That Midfacial Retrusion Is Not Predictable
Semb (1991) and Ross (1987) established that, in the cleft population, both the maxilla and mandible – not solely the maxilla – are retropositioned within the face. If McNeil (1950) belief that the bilateral cleft palatal segments are left behind in their growth was accurate, a greater proportion of the cases must show a Class III malocclusion of one or both sides. As previously mentioned, Berkowitz (1982) mixed cross-sectional study of the occlusion in CBCLP determined that the maxillary complex was not positioned posteriorly relative to the mandible. Also, a buccal crossbite is not a predictable outcome, as McNeil had suggested. Semb (1991) and Ross (1987) concluded that, although the midface and mandible are positioned posteriorly within the face, the maxilla is not retropositioned relative to the mandible and that McNeil’s hypothesis that the maxilla in complete clefts of the lip and palate is retruded and needs to be brought forward was in error.
7.4 Long-Term Facial Growth Findings Show Class III Outcomes Are Not Predictable
Semb (1991) conducted a serial lateral and frontal cephalometric study of 90 cases from the Oslo archives with bilateral cleft lip and palate. Since 1962, the treatment procedure has involved uniting the lip and closing the hard palate cleft space in two stages. No presurgical orthodontics were utilized because the surgeon and Bergland, an orthodontist and director of the program, believed that any bilateral cleft lip can be closed without presurgical palatal manipulation. In the period spanning 1950–1960, a von Langenbeck procedure was performed to close the hard palate cleft between 3 and 4 years of age; after 1960, the timing of the closure was reduced to 18 months of age. Secondary alveolar bone grafting using cancellous iliac crest bone was performed prior to the eruption of the permanent canine teeth.
Twenty-five percent of the cases needed superior-based pharyngeal flaps, which were performed before the child started school. No orthodontics were utilized in the deciduous dentition. Protraction headgear was used in the mixed dentition in one third of the cases. Fixed retention was necessary in all cases. Semb’s study showed that: (1) the maxilla progressively receded over time, (2) the mandible was retrusive with a steep mandibular plane with an increased gonial angle, (3) anterior lower face height was elongated and posterior facial height reduced, and (4) the facial growth pattern was notably different from the normal Bolton standards: (a) Male and female facial growth patterns were similar except that the males’ linear dimensions were larger, (b) the prominent premaxilla would gradually realign in the preschool years, and (c) surgical premaxillary setback was never required. Berkowitz’s unpublished serial cast cephalometric data support these statements (unpublished data).
Vargervik (1983) cross-sectional study of 51 males with BCLP treated with a variety of primary procedures (excluding premaxillary setback) showed profile values similar to those reported by Hellquist et al. (1983), Dahl (1970), Smahel (1984), Semb (1991), and Friede and Johanson (1977). The Oslo team’s average for maxillary prominence and lower face height were slightly more favorable. Narula and Ross (1970), reporting cross-sectional data on thirty 6-year-old subjects and mixed longitudinal data on 34 subjects with BCLP treated conventionally without surgical setback and vomer flap, concluded the maxillary length reached normal values at 16 years of age.
In the Swedish sample followed longitudinally by Hellquist et al. (1983), similar facial convexity was also noted, although both the maxilla and mandible were reported to be slightly more prominent. The patients analyzed by Hellquist et al. (1983) had a two-stage lip closure, pushback palatoplasty, and, at an average age of 6, a delayed periosteoplasty.
Friede and Johanson (1977) reported facial growth in 13 Swedish children with bilateral clefts of the lip and palate (BCLP), five at age 7 and eight at age 10 years. The patients, who had had lip adhesion and vomer flap (without premaxillary setback) and velar closure with pushback, also exhibited facial convexity similar to the Oslo sample.
Friede and Pruzansky (1972), Bergland and Borchgrevink (1974) cephalometric reports of 27 North American children in three treatment groups who were followed to 17 years of age do, however, show some differences in comparison with the Oslo sample. Six subjects treated by early premaxillary setback and seven treated by late setback (3–8 years of age) had profile values similar to those reported by the Oslo group. However, 14 subjects with no premaxillary setback had average values significantly more convex than those reported for the Oslo and other samples. None of the North American subjects had had vomer flaps, and it is implied that a more convex facial profile will be obtained if vomerplasty is excluded from primary surgery.
Also, the negative growth affect of the surgical premaxillary setback may become evident at a later age.
7.5 The Vomer Flap: Good or Bad? Are All Vomer Flaps the Same?
Semb (1991) report on the longitudinal data of the Oslo group is critical of those who condemn the vomer flap. She states that the possible growth-retarding effect of a vomer flap has been discussed by several authors (Friede and Pruzansky 1972; Friede and Morgan 1976; Friede and Johanson 1977; Pruzansky and Aduss 1967; Blocksma et al. 1975; Delaire and Precious 1985, 1986; Friede et al. 1987; Molsted 1987; Enmark et al. 1990). Friede and Pruzansky (1972) observed more favorable growth in patients treated without a vomer flap; however, this is not a uniform finding in the comparative studies. Some clinical centers not using a vomer flap have shown results similar to those where a vomer flap has been utilized. The extent to which the observation of a growth-retarding effect of a vomer flap can be generalized remains in some doubt and may reflect other variations in sample composition or surgery.
The effects of a vomer flap on facial growth have also been considered by the Oslo CLP team (Molsted 1987) which reported the flap to be clinically insignificant. Only one patient in their sample of 90 cases exhibited any degree of maxillary retrusion where surgical maxillary advancement was judged necessary.
In the opinion of the Oslo team, a vomer flap provides the particular advantages of early separation of the nasal and oral cavities without artificial obturators, a low prevalence of symptomatic fistulae, an acceptable arch form, and a good foundation for mixed dentition alveolar bone grafting (Bergland et al. 1986).
Berkowitz’s finding of serial complete bilateral cleft lip show results similar to those of the Oslo group. A modified vomer flap was used in conjunction with a von Langenbeck procedure. He believes that the negative effect of a vomer flap on midfacial growth and arch form, as described by Prysdo et al. (1974), has not been conclusively proven. Patients who have needed LeFort I advancement of only the lateral palatal segments have had very large anterior cleft spaces in the permanent dentition even after the posterior hard palate had been surgically closed at 18–24 months of age with a vomer flap. The premaxillae in these cases were in good overbite-overjet relationships prior to moving the palatal segments into a Class II relationship to close the missing lateral incisor(s) space. Other times, the lateral incisor spaces are left open.
7.5.1 External Elastics Attached to a Head Bonnet or Elastic Tape Strapped to the Cheeks (Fig. 7.9)
Fig. 7.9
(a–c) A head bonnet with an elastic strap (external facial traction) placed against premaxilla is an efficient and painless procedure to ventroflex the premaxilla prior to lip surgery. (a) At birth. (b) With head bonnet in place. (c) After lip repair. The head bonnet aids the surgeon in reducing tension at the lip suture site. The force generated at PVS is less than that created by using mechanical premaxillary retraction (see Chap. 20)
These force delivery systems will reduce premaxillary protrusion prior to lip surgery and only need to be utilized for approximately 1 or 2 weeks. Elastic forces exert the same backward pressure against the protruding premaxilla as a lip adhesion. There are no valid reasons to object to the use of external facial elastic traction with arm restrains to prevent its removal forces for 1–2 weeks prior to lip surgery.
7.5.2 Uniting the Lip (Figs. 7.8, 7.9, and 7.10)
Fig. 7.10
(a–c) Use of the prolabium for the center portion of the lip. IBCLP. (a–c) Facial photographs at 20 days, 3 and 18 months. The banked forked flap (Millard): the tissue in the nostril is used to lengthen the columella at a later date. The procedure avoids going back to a good lip for tissue to reconstruct the columella
Fig. 7.11
Before and after line drawings demonstrating the use of orthopedics for the correction of a malocclusion in a BCLP. 5–9 Frontal and lateral tracings of a child with a bilateral cleft lip and palate before orthopedic treatment. Intracuspid width was 17 mm, intramolar width was 27 mm, and the interincisal angle was 183°. 7–6 After premaxillary advancement and buccal expansion, the intracuspid width changed to 25 mm, intramolar width to 37 mm, and the interincisal angle to 145°. All changes in measurements were dependent on the bodily (orthopedic) movement of the bony segments and not on the movement of teeth (orthodontics). After the palatal segments are properly aligned, the movement of teeth will follow. While waiting for the permanent teeth to erupt, the new arch form needs to be retained with a fixed appliance
Fig. 7.12
(a–f) Millard’s surgical lip procedure uses the prolabium to construct the entire midportion of the lip over the protruding premaxilla. This case was selected to show an example of upper lip protrusion that can result due to a severely protruding premaxilla. This case and others presented in this chapter will show how the face improves with time, that is, facial growth
Fig. 7.13
In 1956–1957, Millard designed a secondary forked flap for columella lengthening. He believed at times it is best to take a little tissue from the prolabium and the lip and store it in the area for later use in reconstructing the columella. The forked flap was originally designed as a secondary procedure; however, it can be used as a primary procedure when the columella is extremely short and the prolabium is of reasonable size. Top: In the primary forked flap, the fork flap is elevated and advanced into the columella with release of the nasal tip. Bottom: The whisker fork flap involves joining the lip muscle and banking the fork. The alar bases are joined together in the midline, and the forks partially tubed on themselves and led into the transverse incisions between the lip and alar bases, whisker fashion. This surgery is delayed several years. Millard likes this procedure best of all
In all complete clefts of the lip and palate at birth, the wide dislocation of the lateral palatal segments coupled with the protruding premaxilla can be gradually overcome by following a treatment protocol that allows the palatal segments to move into proper orientation by the application of the physiological forces of a united lip without the need for presurgical orthopedic treatment. Lip adhesion is followed by definitive lip surgery and observation of facial and palatal changes (Fig. 7.8). If necessary, later surgical premaxillary setback, or surgically moving the lateral palatal segments forward to close a very large persistent anterior cleft space, can be considered.
Clinicians who favor this procedure believe the degree of midfacial protrusion will decrease with facial growth under the influence of the midfacial growth-restraining forces of the united lip (Friede and Pruzansky 1972; Berkowitz 1959; Coup and Subtelny 1960; Pruzansky 1953; Vargervik 1983; Wolfe and Berkowitz 1983; Mazaheri et al. 1971; Bishara and Olin 1972; Aduss et al. 1974).
Findings by Bishara and Olin (1972) and Aduss et al. (1974) support the conclusions drawn from earlier facial growth studies by Berkowitz (1959), Friede and Pruzansky (1972), Handelman and Pruzansky (1968), and Vargervik (1983) that the protruding premaxilla tends to be molded back by lip pressure and can sometimes be aligned within the lateral palatal segments without resorting to neonatal maxillary orthopedics. If not, then the premaxilla in most cases can be aligned within the arch in the deciduous dentition using a fixed orthodontic quad helix appliance.
The use of lip adhesion within the first 3 months followed by a definitive lip revision, usually within the first 6 months of age, permits the surgeon to perform surgery in stages as the face changes. Logan’s bow can be used to reduce the strain at the lip suture when the definitive lip surgery is performed. Surgeons who favor stage treatment procedure are willing to postpone obtaining a maximum early aesthetic result for what they believe will offer superior long-term benefits. The most severe unaesthetic premaxillary overbite in the deciduous and mixed (transitional) dentition, even with a buccal crossbite, will not interfere with dental function or swallowing or have any long-term deleterious effects on speech and midfacial growth.
7.6 Profile Changes (Figs. 7.14, 7.15, 7.16, 7.17, and 7.18)
Fig. 7.14
Computerized digital tracings of the perimeter of the outline of CBCLP palatal casts superimposed on the palatal rugae and registered on the vomer. Palatal cleft closure between 18 and 24 months using a von Langenbeck and vomer flap. Note that the premaxilla is held in place, while the palate grows in all directions; posterior palatal growth occurs to accommodate the developing molars. None of these cases were treated with presurgical orthopedics
Fig. 7.15
In spite of the lip surgery performed, the position of the premaxilla in the anterior dentition is determined by the facial pattern and tonicity of the surrounding facial musculature. Case #746: Protruding premaxilla surrounded by hypotonic lip musculature. Case #742: Retrognathic mandible with protrusive premaxilla. The lower lip is positioned between the upper and lower incisors creating a forward force at the PVS. The resulting increase in tension at the PVS stimulates additional growth and causes increase in inclination of the upper incisors. Case #174: Retrognathic mandible with less premaxillary protrusion hypertonic lip musculature creating severe lip pressure which ventroflexes the premaxilla. Variations in premaxillary position are unpredictable (Handelman 1968)
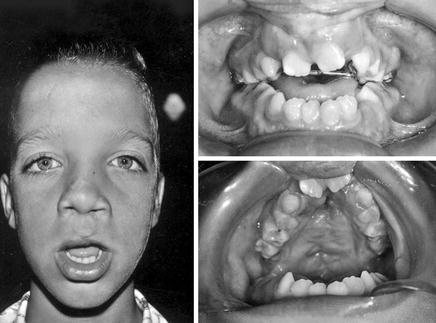
Fig. 7.16
Early premaxillary surgical setback and palatal cleft closure at 7 months of age. The lateral lip elements were brought together below the prolabium. Results at 7 years of age: (1) long tight upper lip, (2) anterior open bite due to failure of the premaxilla to descend with the palate, and (3) the surgery (pushback) used to close the palatal cleft at 7 months obliterated the vault space interfering with tongue posture. The tongue is, therefore, being carried forward with the tongue tip protruding, preventing the incisors from reaching the occlusal plane
Fig. 7.17
(a–c) The lateral lip elements were brought below the prolabium creating a long tight lip
Fig. 7.18
(a, b) Good facial growth pattern with hypertonic lip musculature. a Lateral cephalometric tracing shows a gradual increase in the angle of facial convexity (NaPo) from 116° to 169° with the greatest change (159–169°) occurring between 5 and 6 years, 5 months of age. At 5 years, the axial inclination of the anterior teeth is vertical with an appreciable incisor overjet. However, at 6 years, 5 months, the premaxilla is palatally inclined, placing the upper and lower incisors in a tip-to-tip relationship. This usually occurs with a relatively retrognathic mandible when the lower lip also overlaps the upper incisors, increasing the muscle pressure against the premaxilla. If the lower lip is positioned between the upper and lower incisors, the premaxilla with its incisors will flare. (b) Superimposed polygons show a very small mandible with a protruding premaxilla at 0–1–18. There is a marked anterior growth of the anterior cranial base (N) and, together with the mandible’s vertical and horizontal growth changes, a reduction in the angle of facial convexity. Note that there is very little change in premaxillary protrusion within the face between ages 1–2–22 and 7–8–12
Hanada and Krogman (1975), Berkowitz (1959), Bishara and Olin (1972), Boyne (1974), Vargervik (1983), Handelman and Pruzansky (1968), Friede (1977), Semb (1991), and Narula and Ross (1970) all have performed longitudinal studies of the changing soft tissue profile of bilateral cleft lip and/or palate (BCL/P) and reported that, with the slow resolution of the protruding premaxilla with growth, the profile became more harmonious in appearance. In the Oslo study of BCLP, Semb (1991) concluded that early dentofacial orthopedics were not a necessary precursor to lip and palate closure in order to attain long-term positive profile changes.
Serial profile analyses of cast and cephalographs reported in Berkowitz’s earlier studies and the serial studies presented in this text demonstrate that, during the first 2 years following surgery, the united lip exerts a posteriorly directed pressure force on the protruding premaxilla. He speculates that this force is exerted through the nasal septum to the premaxillary-vomerine suture, gradually retarding the forward and vertical growth of the nasal septum with the attached premaxilla. The growth of the lateral palatal segments does not appear to be affected by this force. Inhibition of midfacial growth coupled with forward and vertical growth of the upper face and mandible is responsible for the eventual flattening of the facial profile (Figs. 7.5 and 7.6).
Protrusion of the midface is only slightly reduced by the reduction-remodeling of the labile surface of the premaxilla associated with the eruption of the permanent incisors. Facial growth data suggest that the tendency toward mandibular prognathism can be considered advantageous, insofar as it reduces the earlier protrusion of the premaxilla. Comparison of the profile changes in children whose lips were united at 6 years with infants whose lips were united soon after birth showed less premaxillary protrusion for children whose lips were repaired in infancy. This suggests that the beneficial effect of lip repair is long-acting in that it continues to exert a restraint on the growth of the premaxillary-vomerine complex long after the lip is repaired (Friede and Pruzansky 1972; Berkowitz 1959; Vargervik 1983).
After the lip is united, there are no documented long-term benefits to using intraoral neonatal maxillary orthopedics to control the premaxilla’s position relative to the lateral palatal segments (i.e., to inhibit the palatal segments from spontaneously moving together) nor is it important that the premaxilla be accommodated within the arch at this time. There is no evidence that overlapping palatal segments suffer growth inhibition. In most cases, proper premaxillary alignment within the lateral palatal segments can be easily achieved with orthodontics in deciduous or mixed dentition without resorting to neonatal maxillary orthopedics. The following cases show that orthodontics in the permanent dentition, in the absence of growth-inhibiting palatal surgery, and with a good or poor facial growth pattern eventually will lead to excellent facial aesthetics and dental function. Any resulting buccal crossbite can be easily corrected at 4 or 5 years of age, when the child is manageable in a dental chair, using fixed tooth-borne or even removable arch expansion appliances. The author strongly favors the use of fixed appliances for arch expansion and retention.
There are many occasions when the profile shows midfacial retrusion due to severe ventroflexion of the premaxilla. As long as during the mixed dentition gingivoperiosteoplasty has not been performed (see Chap. 20), the premaxilla can easily be brought forward orthodontically and held in place until alveolar bone grafting is performed. Retention of the corrected maxillary arch is still necessary until orthodontics are completed (Fig. 7.11).
7.6.1 Why Some Premaxillae Continue to Project Following Lip Repair and Others Do Not
The cases being presented will show that there are a number of treatment planning facial factors. For example, the patient’s facial growth pattern and the amount of palatal osteogenic deficiency are beyond the control of the surgeon. The integrated growth of the entire face is important to resolve the profile deformity. When the end result is unfavorable – that is, the facial profile remains highly convex – the premaxilla and the body of the maxilla usually have grown forward with limited forward mandibular projection or tension has been created at the PVS, causing further premaxillary protrusion.
Facial growth studies by Handelman and Pruzansky (1968) and by Berkowitz (presented in this chapter) have shown that, in highly convex facial profiles with a moderately protrusive premaxilla and a recessive mandible, the lip musculature usually is hypertonic and positioned over the upper incisor teeth, resulting in severe premaxillary ventroflexion. In mesognathic faces with isotonic or hypotonic lip musculature and a severely projecting premaxilla, the lower lip may be positioned lingual to the premaxilla and between the upper and lower incisors, creating an anterior component of force at the premaxillary-vomerine suture (PVS). This may cause additional bony growth at the suture, leading to greater premaxillary protrusion with a normal maxillary incisal axial inclination. The lower incisors may be tipped lingually (Figs. 7.11 and 7.12).
The serial record present in the case reports to follow will show that it can be anticipated that in most cases (53 out of 59 CBCLP; S Berkowitz, unpublished data), good faces will have developed at adolescence. Figure 7.14 shows serial computer-generated CBCLP palatal cast outlines which were superimposed on the palatal rugae and registered on the vomer. All of these cases had the palate closed between 18 and 24 months using a von Langenbeck with modified vomer flap (it was readily observed at every age period).
This illustration clearly demonstrates that the premaxilla is in the same place in the palate at adolescence as it was at birth. It is retained in place by the surrounding facial musculature in most cases. There are exceptions, usually dependent on the balance of the facial musculature.
7.6.2 Dental Occlusion
Analyses of the dental occlusion of many patients with complete bilateral clefts of the lip and palate at 6 years of age rarely show retruded maxillary shelves (i.e., a Class III relationship) (Berkowitz 1959). The buccal teeth are most often in a Class I or II relationship. A Class III relationship exists only if the maxilla is retrusive due to severely retarded growth caused by traumatic surgery and/or the patient’s phenotype. The mandible is rarely prognathic at this age. In many cases, due to palatal osteogenic deficiency and severe dental crowding in the maxillary arch, some teeth may need to be extracted. This may or may not have to be done in the mandibular arch. There is conclusive evidence to suggest that the cleft palatal shelves may be deficient in mass, but there is no evidence that they have lost their growth impetus from having been detached from the growing nasal septum.
Until proven otherwise, the surgeon should have confidence that the severe facial convexity seen at birth can diminish with time as the united lip restrains the forward development of the midface, while the mandible increases in size and is positioned more downward and forward relative to the growing anterior cranial base and midface.
7.6.2.1 After Birth
In general, no presurgical orthopedics were provided other than the use of a head bonnet. In complete bilateral cases only, an external facial elastic may be utilized to ventroflex the protruding premaxilla to reduce tension at the surgical site when utilizing lip adhesion. External traction is usually not necessary in incomplete clefts of the lip and palate.
The Forked Flap (Fig. 7.13)
All of the bilateral cases were treated with Millard’s forked flap (Millard 1978a). It was designed to lengthen the columella as a primary or secondary procedure. Advantages include:
-
Release of depressed nasal tip
-
Lengthen the short columella
-
Reduce an unattractive wide prolabium
-
Revision of bilateral lip scars
-
Reduction of flaring alar bases
Millard (1978a, b) suggests that the primary fork flap procedure is not appropriate for all bilateral cleft cases. Whether to use the procedure depends on: (1) The position of the premaxilla. It should not be used when the premaxilla is severely protruded. (2) The size of the prolabium. The width of the prolabium determines whether the flap is possible, and the vertical length indicates the amount of columella lengthening available. (3) Columella length. This discrepancy must be measured not only in actual length in millimeters of the columella, but an estimation of the patient’s desired final length must also be made.
There are occasions where the forked flaps from the prolabium are banked with a subalar incision, whisker fashion. The alar base is not advanced medially in an attempt to leave a subalar gap in which to store the forks. Millard delays shifting of the banked forked flap into the columella for several years (from 6 months to 6 years).
7.6.2.2 In the Deciduous Dentition (3–6 Years of Age)
The purpose of treatment at this age is to align the palatal segments in order to obtain a more normal contour to the alveolar ridge, reshape the palatal vault, and provide a more symmetrical foundation for the support of the lips and nose. These changes are possible because orthodontic treatment in cleft palate allows for the movement of palatal segments when using a von Langenbeck procedure in addition to altering the position of the teeth within the alveolus. Because the roof of the mouth is also the floor of the nose, realignment of the palatal processes not only produces desirable alteration in the contour of the palate but also induces similar changes within the floor of the nose.
Most clinicians agree that nontraumatic conservative surgery will not solve all problems for all complete bilateral cleft lip and palate cases. Although buccal crossbites can be corrected in the deciduous dentition, some advocate orthodontic/orthopedic repositioning of the premaxilla at a later age (in the mixed dentition prior to or after secondary alveolar bone grafting) when the facial growth pattern leaves no alternative and dictates that it is the procedure of choice. Some orthodontists prefer to do this in the permanent dentition.
7.6.2.3 Mixed Dentition (6–11 Years of Age)
When a child with a cleft starts elementary school, even if the protruding premaxilla still extends far forward of the lateral palatal segment creating a severe convex facial profile, a surgical premaxillary setback should be considered solely for aesthetic reasons because there can be long-term deleterious effects. This decision is a difficult one. One is damned if one does or doesn’t! One has to balance the child’s social and psychological needs with long-term facial developmental factors.
In the last 20 years, many reports published with improved documentation were critical of surgical premaxillary setback performed in the newborn period, or even in early adolescence prior to the prepubertal growth spurt. Fortunately, these criticisms led to abandonment of this procedure (Vargervik 1983).
Orthodontics applied during the mixed dentition, in preparation for or after secondary alveolar bone grafting (the placement of bone in the alveolar cleft after the first year of age), can aid in reducing the premaxillary overbite and maintaining the premaxilla within the lateral palatal segments. Eliminating the alveolar cleft permits the unerupted teeth (lateral incisors and cuspids) adjacent to the cleft to erupt or be moved into proper position.
In Berkowitz’s experience, a protruding premaxilla – with or without a large anterior cleft space – at 6–7 years of age does not signify that the same unpleasant aesthetic conditions will persist into adolescence. After the pubertal facial growth spurt, when the facial convexity is markedly reduced because of increased mandibular and upper facial growth, facial aesthetics will be greatly improved in most patients.
There is strong psychosocial pressure on clinicians to improve facial aesthetics as soon as possible, even when the premaxilla cannot be retropositioned in the absence of an anterior cleft space. For this reason, many unsuccessful attempts have been made to surgically or mechanically set the premaxilla back at an early age in the hope of preventing an unaesthetic midface at a later age, believing the midfacial growth would still be normal. At this difficult period, every effort should be made to convince both the parents and the child, using before and after photographs, that facial aesthetics will greatly improve as the face grows and that the long-term benefits far outweigh any early improvements at the expense of future good facial growth.
7.6.2.4 At Adolescence
If a poor facial growth pattern at adolescence with a large anterior cleft space leads to a protruding premaxilla set well forward in the facial profile and the mandibular incisors, the premaxilla can be surgically set back. A secondary alveolar bone graft is simultaneously performed to close the remaining anterior cleft space. A fixed palatal retainer or a heavy labile arch wire must be utilized for at least 2 months as a supporting splint for the three segments during the healing period.
There are cases in which both buccal segments are in a Class I relationship, a large anterior cleft space is present, and the premaxilla is missing one or both lateral incisors, yet it is in an ideal overjet and overbite relationship. If the surgeon believes that the anterior cleft space is too large to be successfully closed by a secondary alveolar bone graft, the only remaining option is to surgically advance one or both palatal segments, placing the buccal teeth in a Class II relationship with at least one, but sometimes both, of the cuspids in the lateral incisor space. This usually necessitates the surgical increase in posterior transpalatal width. A secondary alveolar bone graft is performed at the same time (Posnick and Tompson 1993).
There are too many variations of orthodontic problems to review each of the treatment plans separately. However, in most cases, a common treatment sequence is usually followed. First, the posterior palatal crossbite needs to be orthopedically corrected in the deciduous or mixed dentition using quadhelix mechanics. Reducing maxillary arch crowding by tooth extractions may be necessary due to the lack of palatal osteogenic tissue. Achieving ideal anterior teeth aesthetics often requires that the lost lateral incisor spaces be recovered for the eruption of impacted lateral incisors or cuspids. In most cases, establishing room for four maxillary incisors by expansion and slight incisor advancement is the ideal treatment. A slightly retrusive maxilla with mild crowding may require the advancement of the upper jaw using protraction forces for at least 6–12 months to obtain an ideal anterior overbite-overjet relationship. In some instances, the extraction of one lower incisor to correct the mandibular anterior arch will be necessary to reduce an anterior crossbite.
In all cleft types, involving the lip and palate, orthodontic surgical treatment decisions are often dictated by the relationship of the premaxilla to the lateral palatal segments and the facial growth pattern (i.e., whether the face is prognathic, mesognathic, or retrognathic). For example, if a slightly retruded maxilla and a retrognathic mandible coexist, it may be necessary to surgically advance the lower jaw with or without doing the same to the maxilla. In most cases, orthopedic protraction to move the maxilla should be considered first.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


