Introduction
The aim of this study was to compare the effectiveness of Twin-block and Dynamax appliances for the treatment of Class II Division 1 malocclusion.
Methods
This was a randomized controlled trial involving 32 boys and 32 girls aged 10 to 14 years with Class II Division 1 malocclusion. They were randomly allocated to either the Dynamax appliance group or the Twin-block appliance group. Treatment was provided by 4 clinicians at 2 centers. Records were taken at the start and the end of the functional phase and after all treatment. In addition, incisal overjet, the number of appliance breakages, and adverse events or side effects of the treatment were recorded at each patient visit.
Results
The data monitoring committee in an interim analysis at 18 months after the start of the trial found significantly greater overjet reduction in the Twin-block group than in the Dynamax group and more breakages and adverse events with the Dynamax appliance. As a result, treatment with the Dynamax appliance was terminated, and those patients completed treatment with the Twin-block or a fixed appliance. Regression analysis showed a statistically significant difference in the performance over time between the Twin-block and Dynamax appliances in terms of reduction in overjet, with the Twin-block appliance performing significantly better than the Dynamax. The incidence of adverse events was greater in the Dynamax group (82%) than in the Twin-block group (16%), with a statistically significant difference ( P <0.001) between the 2 groups.
Conclusions
The Twin-block appliance was more effective than the Dynamax appliance when overjet was evaluated and the Dynamax appliance patients reported greater incidence of adverse events with their appliance than those who were treated with the Twin-block appliance.
In this article, we describe a study that compared the effectiveness of the Twin-block and the Dynamax appliances for the correction of Class II Division 1 malocclusion. The Dynamax appliance was developed in 2003 for the treatment of Class II malocclusion. It was designed to (1) allow the operator to simply activate incremental mandibular advancement, (2) simultaneously provide the functional and mandibular arch fixed appliance phases of treatment, (3) limit both mandibular incisor proclination and maxillary incisor retroclination, and (4) minimize any increase in lower facial height.
There has been limited research about the effectiveness of this appliance; only 1 randomized controlled trial (RCT) has been carried out to date. The effects of the Dynamax appliance were compared with the Twin-block appliance in Class II Division 1 patients, and interesting findings were reported. However, the trial did not use the CONSORT guidelines; thus, it was impossible to evaluate several important factors. For example, the potential noncompliance rate was not accounted for in the sample size calculation, the method of random sequence generation was not clearly stated, the investigators did not carry out an intention-to-treat analysis, and the statistical analysis was simplistic. Importantly, the study was carried out in 1 dental school setting, and this raises the question whether the Dynamax is an effective treatment in a “real world” setting.
To add to the scientific evidence about the relative effectiveness of these 2 appliances, we undertook an RCT to compare the effectiveness of the Dynamax and the Twin-block appliances for the treatment of Class II Division 1 malocclusion in a setting that was not a dental school. The null hypotheses were that there was no significant difference between the Twin-block and Dynamax appliances with regard to treatment duration, dentoocclusal outcome, skeletal and soft-tissue profiles, and patient discomfort.
Material and methods
This RCT was coordinated by the University of Manchester. Treatment was provided by 4 clinicians at 2 centers in the United Kingdom: Chesterfield Royal Hospital North Derbyshire and Derbyshire Royal Infirmary. The study was approved by the Central Research Ethics Committee of the United Kingdom in 2007.
The sample size calculation was based on the data from a previous investigation into the effectiveness of the Twin-block and Herbst appliances. We considered that a minimum clinically meaningful difference in treatment duration between 2 competing treatments was 4 months (common SD, 4.61). For a trial with a power of 80% and an alpha of 0.05, a sample of 32 patients in each group was required, with an estimated noncompliance rate of 30%.
The inclusion criteria were overjet greater than 6 mm, age 10 to 14 years, no craniofacial syndrome, and no previous orthodontic treatment or premolar extractions.
All patients who satisfied these criteria were asked whether they were willing to participate in the trial. Treatment allocation was performed centrally by independent research assistants at the University of Manchester, thereby ensuring that recruitment and treatment allocation were completely independent.
When a patient agreed (or the patient’s parent gave permission for the child) to take part, the clinician contacted the central telephone line for the trial and gave the patient the details of the study. Patients were then allocated by using minimization to one of the treatments by using MINIM software, with sex as a prognostic factor.
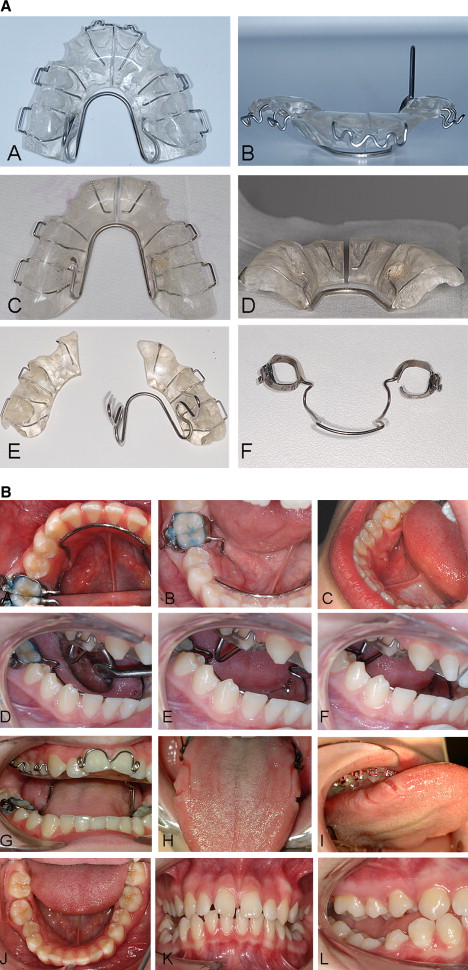
We used a modified Twin-block appliance design, with an angle of 75° for the posterior bite blocks. Retention was provided by 0.7-mm Adams clasps on all first premolars and first molars and 0.9-mm ball-end clasps between the mandibular incisors. An expansion screw was used in the maxillary appliance for any necessary arch expansion. All appliances were similar. Headgear was not used with the Twin-block appliance. All patients were advised to wear the appliance 24 hours a day (except during contact sports and swimming). Reactivation of the blocks was carried out when considered necessary by the treating clinician.
The Dynamax appliance consisted of a removable appliance in the maxillary arch, with 0.7-mm Adams clasps on the maxillary first molars and first premolars, a 0.7-mm anterior torque spring on the maxillary central incisors, and a 1.0-mm fixed lingual arch in the mandible ( Figs 1 and 2 ).
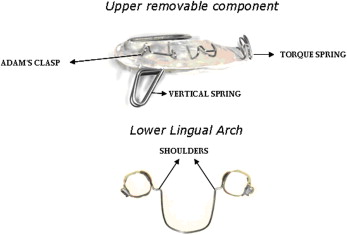

The maxillary removable acrylic plate had a midline split with a 1.0-mm stainless steel Coffin-type spring incorporated to achieve expansion. The mandibular lingual arch had “shoulders” (lingual projections) of 3 mm, formed on the lingual aspect of the molar bands, at right angles to the bands. The occlusal surface of the maxillary posterior teeth was covered with acrylic 1 mm thick. A 14-mm vertical spring was incorporated in the maxillary removable appliance, which fitted behind the “shoulders” of the mandibular lingual arch and induced an avoidance mechanism to ensure that the patient held his or her mandible in the advanced position slightly ahead of the point of contact of the lingual shoulder and the vertical arm. The design of the vertical spring was meant to ensure that chair-side reactivation of the appliance was quick and easy. Reactivations of 2 to 3 mm were carried out every 6 weeks, or when the desired overjet change was achieved. Headgear was not used in any of the appliances.
All operators were highly experienced in the use of functional appliances. However, to address possible unfamiliarity with the Dynamax, they attended a course in its clinical use given by its developer.
The patients were followed up every 6 weeks after appliance placement, and overjet, overbite, molar width, and canine and molar relationship measurements were recorded at every visit. For this trial, patients were followed for 9 months.
According to the trial protocol, the operator recorded a patient as noncompliant if he or she refused to wear the appliance, the appliance broke or was damaged more than 3 times so that further treatment with that appliance was impractical, or the routine measurements indicated no clinical improvement after 9 months of appliance wear.
For data collection, we took study models, cephalometric radiographs, and extraoral and intraoral photographs at the start of treatment, the end of functional appliance treatment, and the end of all orthodontic treatment. In addition, incisal overjet, the number of appliance breakages, and any adverse or side effects of the treatment were recorded at each patient visit. This latter category could include any emergency appointment other than for breakages—eg, severe appliance trauma, sore tongue, mandibular lingual arch impinging on the lingual mucosa, and decementation of the appliance ( Fig 3 ).
The trial conformed to the United Kingdom’s Medical Research Council good clinical practice guideline recommendations for clinical trials, and a data monitoring committee (DMC) was set up to monitor the progress of the trial and perform interim analyses when appropriate. This DMC included an independent statistician and an orthodontist who were not involved in the trial.
Statistical analysis
The data were analyzed by using SPSS (version 15.0, SPSS, Chicago, Ill) and STATA (StataCorp, College Station, Tex) software. The data were analyzed on an intention-to-treat basis. The DMC assessors and the trial statistician were blinded to treatment allocation.
An interim analysis and a final analysis were proposed. By using the rule of O’Brien and Fleming, significance levels of 0.0054 for the interim analysis and 0.049 for the final analysis were used, instead of a significance level of 0.05.
A linear mixed model was estimated with the STATA software to examine the overall pattern of, and individual differences in, overjet reduction from baseline over 6 visits (9 months). For categorical data, the chi-square analysis was used, with an alpha level of 0.05.
Results
Patient recruitment was started in January 2007 and completed in January 2008. Sixty-four patients were enrolled. Thirty-two (16 girls, 16 boys) were allocated to the Twin-block group, and 32 (16 girls, 16 boys) were in the Dynamax group. Figure 4 illustrates the flow of patients through the project.

The DMC conducted an interim analysis 18 months after the start of the trial and used changes in overjet, frequency of breakages, and the number of problems that the patients experienced with their appliances as outcome measures. They concluded that the changes in overjet were significantly greater in the Twin-block group than in the Dynamax group and that there were greater incidences of breakages and other problems with the Dynamax than with the Twin-block. As a result, the committee decided that it was unethical to continue the Dynamax arm of the trial, since the patients’ treatments were being compromised. Consequently, the patients in the Dynamax group were transferred to complete their treatment with the Twin-block appliance or a fixed appliance. All patients initially allocated to the Dynamax group had worn their appliance for at least 9 months before transfer.
When the trial was stopped, 17 Twin-block patients and 5 Dynamax patients had completed the first functional phase of treatment. Seven Twin-block patients and 3 Dynamax patients had dropped out of the trial. In the Dynamax group, the clinicians decided to transfer 11 patients to Twin-block treatment, because they had too many breakages (3 patients), or overjet reduction was either minimal or nonexistent (8 patients). Seven patients were transferred to fixed appliance treatment. One patient in the Twin-block group was moved to headgear treatment. Even though the trial was stopped early, we carried out the data analysis for all 64 patients who started treatment with the primary outcome measure being overjet with secondary outcomes of appliance breakages and other adverse effects.
The individual and mean reductions in overjet by treatment allocation are shown in Figure 5 . The mean value for the Twin-block group was slightly elevated at 36 weeks (visit 6), because the patients who completed the functional phase of treatment are not included.
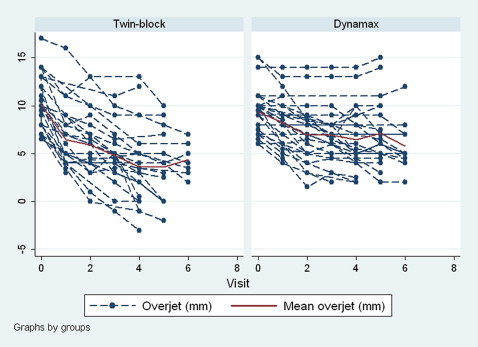
For the mixed-effects regression analysis, time was treated as semicontinuous (7 values from 0 [baseline] to 6 [36 weeks]) to evaluate whether there was a differential trend between the groups for overjet reduction. The coefficient for the effect of “visit” suggested overjet changes of –1.34 mm per visit for the Twin-block group and –0.63 for the Dynamax group. The difference of slopes according to appliance is highly significant with a coefficient of 0.71 ( Table I ). From the predicted slopes ( Fig 6 ), the overall change (reduction) was greater (steeper) for the Twin-block group than for the Dynamax group.



